The current European Society of Cardiology guidelines for revascularization confer a Class I indication (level of evidence A) for coronary artery bypass grafting (CABG) in multi-vessel coronary artery disease (MVD).1 However, due to recent advances in percutaneous coronary intervention (PCI), with new generation drug-eluting stents (DES) and more potent antiplatelet agents, in addition to increasing operator experience and availability of adjunctive tools (intravascular ultrasound and fractional flow reserve guidance), the frequency of PCI for MVD has increased. Indeed, there is a Class IIa (level of evidence B) indication for PCI with a “SYNergy between PCI with TAXus and cardiac surgery” (SYNTAX) score ≤22 in those patients with chronic stable MVD.1
Both clinical and anatomical characteristics of the patient have to be taken into account in the decision making regarding the optimal method of revascularization for a patient with MVD. Careful risk stratification and active discussion with a multidisciplinary Heart Team is recommended in this patient subset.1 Not all MVD is the same and as such each patient should be assessed on an individual basis to ensure that the most appropriate revascularization modality is chosen to provide favourable long-term outcomes.
Individuals with MVD presenting as an acute coronary syndrome (ACS) require clinical decision making that also takes into account the urgency of revascularization, and such studies have not been included in this article. The aim of this editorial is to discuss factors influencing the decision making between PCI and CABG in patients with chronic MVD.
CURRENT EVIDENCEHistorically, CABG has been the gold standard treatment for patients with MVD; a large meta-analysis of major CABG studies demonstrated a definite benefit of surgery in high- and medium-risk patients compared with medical therapy.2 More recently, several studies have compared the long term outcomes of PCI versus CABG for the treatment of MVD, with results demonstrating no difference in mortality but a greater need for revascularization in the PCI cohorts. A large pooled analysis of 3051 patients from 4 randomized trials comparing PCI using bare metal stents with CABG confirmed a persistently higher need for repeat revascularization with PCI to 5 years follow-up (PCI 29.0% vs CABG 7.9%; hazard ratio [HR]=0.23; 95% confidence interval [95%CI], 0.45-0.61; P<.001). Of note in this study, there was no difference in the incidence of death (PCI 8.5% vs CABG 8.2%; HR=0.95; 95%CI, 0.73-1.23; P=.69) or stroke (PCI 3.1% vs CABG 3.6%; HR=1.16; 95%CI, 0.73-1.83; P=.54).3
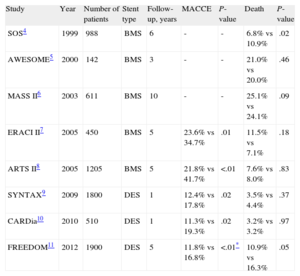
The introduction of the DES in 2003 and subsequent demonstration in randomized trials of a significant reduction in the rate of restenosis compared to bare metal stents has led to an increased confidence by the interventional cardiologist to tackle more complex MVD, which had previously been the realm of the cardiothoracic surgeons. Table illustrates outcomes of major studies comparing PCI with CABG in MVD.4–11
Studies of Coronary Artery Bypass Grafting Versus Percutaneous Coronary Intervention in Multi-vessel Disease
| Study | Year | Number of patients | Stent type | Follow-up, years | MACCE | P-value | Death | P-value |
| SOS4 | 1999 | 988 | BMS | 6 | - | - | 6.8% vs 10.9% | .02 |
| AWESOME5 | 2000 | 142 | BMS | 3 | - | - | 21.0% vs 20.0% | .46 |
| MASS II6 | 2003 | 611 | BMS | 10 | - | - | 25.1% vs 24.1% | .09 |
| ERACI II7 | 2005 | 450 | BMS | 5 | 23.6% vs 34.7% | .01 | 11.5% vs 7.1% | .18 |
| ARTS II8 | 2005 | 1205 | BMS | 5 | 21.8% vs 41.7% | <.01 | 7.6% vs 8.0% | .83 |
| SYNTAX9 | 2009 | 1800 | DES | 1 | 12.4% vs 17.8% | .02 | 3.5% vs 4.4% | .37 |
| CARDia10 | 2010 | 510 | DES | 1 | 11.3% vs 19.3% | .02 | 3.2% vs 3.2% | .97 |
| FREEDOM11 | 2012 | 1900 | DES | 5 | 11.8% vs 16.8% | <.01* | 10.9% vs 16.3% | .05 |
ARTS, Arterial Revascularization Therapies Study; AWESOME, Angina With Extremely Serious Operative Mortality Evalution; BMS, bare metal stents; CARDia, Coronary Artery Revascularization in Diabetes; DES, drug eluting stents; ERACI, Argentine Randomized Trial of Coronary Angioplasty With Stenting Versus Coronary Bypass Surgery in Patients With Multiple Vessel Disease; FREEDOM, Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal management of Multi-Vessel Disease; MACCE, major adverse cardiovascular and cerebrovascular events; MASS, Medicine, Angioplasty of Surgery; SOS, Stent or Surgery; SYNTAX, SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery.
A large registry study of 17 400 patients reported a lower occurrence of death at 18 months follow-up in patients undergoing CABG for three-vessel coronary disease (adjusted HR=0.80; 95%CI, 0.65-0.97; P=.03).12 However, this study was limited in the retrospective design and covariate imbalances.
The landmark clinical trial comparing PCI with DES versus CABG in MVD was the SYNTAX study. This was an all-comers, international, prospective randomized clinical trial, including 1800 patients with MVD (57% chronic stable angina) randomized to receive PCI with paclitaxel-eluting stent vs CABG. The primary study endpoint, noninferiority of PCI in major adverse cardiovascular and cerebrovascular events (MACCE) at 1 year, was not met (PCI 17.8% vs CABG 12.1%; P=.002), mainly due to a significantly higher rate of repeat revascularization (13.7% vs 5.9%; P<.001). However, a higher rate of stroke was reported in the CABG group (0.6% vs 2.2%; P=.003). Of note, there was no difference between groups in the occurrence of death, stroke, or myocardial infarction (MI) (PCI 7.6% vs CABG 7.7%; P=.98).9
The 5-year results of this study have recently been published, showing a continued difference in MACCE favouring CABG (PCI 37.3% vs 26.9%; P<.0001) due to higher revascularization rates with PCI (9.7% vs 3.8%; P<.0001). However, there were still no differences in all-cause mortality (PCI 11.4% vs CABG 13.9%; P=.10) or stroke (PCI 2.4% vs 3.7%; P=.09).13
It must be taken into account that this study was performed utilizing first generation DES, which have subsequently been shown to be inferior to the new generation DES, both with regards to the need for revascularization and also in the incidence of stent thrombosis. The ‘Clinical Evaluation of the Xience V Everolimus Eluting Coronary Stent System in the Treatment of Patients with de novo Native Coronary Artery Lesions’ (SPIRIT) III and IV randomized trials pooled the data from 4689 patients with MVD. This demonstrated that the new generation everolimus-eluting stents, compared with the first generation paclitaxel-eluting stents (as used in the SYNTAX study), resulted in reduced rates of ischemia-driven target lesion revascularization in those with MVD (4.2% vs 8.0%; P=.04), including in those undergoing multi-lesion stenting (3.7% vs 7.4%; P=.01). Indeed, the absolute benefits of the new generation stent were greater than in those undergoing single lesion, single vessel PCI.14
RISK STRATIFICATION IN MULTI-VESSEL CORONARY ARTERY DISEASERisk stratification is an important component in the determination of the most appropriate revascularization modality in conjunction with the ‘Heart Team’. Within cardiothoracic surgical practice, the use of risk scores is well established and predominantly related to clinical factors, such as the Society of Thoracic Surgeons (STS) Score and the Logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE).
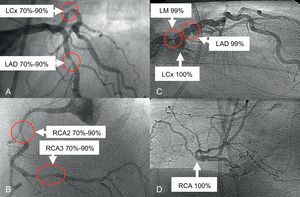
In the field of PCI, risk scores have continued to evolve over recent years. The SYNTAX study introduced the ‘SYNTAX Score,’ which is anatomically based, to assess coronary lesion complexity. Further analyses of the SYNTAX study were performed dependent on the determination of low risk (SYNTAX score <23), intermediate risk (23-32), or high risk (>32). At 5 years, in the overall cohort of high-risk patients, there remained a significant difference favouring CABG in MACCE (PCI 44.0% vs CABG 26.8%; P<.0001), with similar differences in the intermediate risk group (36.0% vs 25.8%; P=.008). Importantly, in the low anatomical risk group, there was no difference in the occurrence of MACCE (32.1% vs 28.6%; P=.43).13 This suggests that not all MVD is the same, as illustrated in Figure. Figures A and B shows a patient with MVD and a SYNTAX score of 21 who, due to low anatomical risk, underwent successful PCI with everolimus-eluting stents. Conversely, Figures C and D shows a patient with complex MVD (SYNTAX score 52) who was referred for CABG following ‘Heart Team’ discussion.
A and B: Illustrate a patient with multi-vessel disease and a SYNTAX score of 21. C and D: Show a patient with more complex anatomy and a SYNTAX score of 52, demonstrating not all multi-vessel disease is the same. Following a Heart Team discussion, patient 1 was treated with percutaneous coronary intervention with implantation of everolimus-eluting stents and patient 2 underwent coronary artery bypass grafting. LAD, left anterior descending; LCx, circumflex; LM, left main; RCA, right coronary artery.
There are a number of other risk scores that have been developed for the assessment of MVD patients, including the New Risk Classification Score consisting of 54 variables (17 clinical, 33 angiographic, and 4 procedural factors), which has yet to be validated in a large randomized population of patients. There is also a Global Risk Score, which combines the SYNTAX score with the additive EuroSCORE combining historically accepted clinical variables with the angiographic variables.
In order to overcome the limitations of the widely used SYNTAX score, namely the absence of clinical variables, the SYNTAX Score II has most recently been developed. It incorporates features which have previously been captured in the traditional surgical scoring systems and aims to provide a more reliable means to help in assessment of patients with MVD. Baseline clinical features with strong associations with mortality at 4 years in the SYNTAX Study were added to the original anatomical SYNTAX Score, including age, creatinine clearance, left ventricular ejection fraction, peripheral vascular disease, female sex, and chronic obstructive pulmonary disease. It is believed that this approach may better guide decision making between PCI and CABG in complex patient groups. Undeniably, a combination of both clinical and anatomical characteristics is necessary for an effective risk stratification model for patients with complex MVD considering PCI.
MULTI-VESSEL CORONARY ARTERY DISEASE AND DIABETES MELLITUSPatients with diabetes mellitus pose a particular challenge in view of the extent and the aggressive nature of the disease, with smaller coronary arteries and diffuse disease. These characteristics are associated with a higher degree of restenosis following PCI and less favourable long-term survival with both revascularization strategies compared to those patients without diabetes mellitus.
The first study directly comparing PCI with CABG in 510 patients with diabetes mellitus was the ‘Coronary Artery Revascularization in Diabetes’ (CARDia) trial, which demonstrated no difference in the primary composite endpoint of death, MI and stroke at 1 year (PCI 13.0% vs CABG 10.5%; HR=1.25; 95%CI, 0.75-2.09; P=.39), however when repeat revascularization was added to this endpoint, the results were favourable with CABG (19.3% vs 11.3%; HR, 1.77; 95%CI, 1.11-2.82; P=.02).10 Of note, in this study, first generation DES (sirolimus-eluting stents) were used in 69% of patients, with the remainder undergoing bare metal stents implantation.
The ‘Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal management of Multi-Vessel Disease’ (FREEDOM) study was recently reported, which randomized 1900 patients with MVD and diabetes mellitus to PCI with first-generation DES versus CABG. At 5 years, the primary composite outcome of all cause mortality, nonfatal MI, or nonfatal stroke occurred more frequently in the PCI group (PCI, 26.6% vs 18.7%; P=.005), which was driven by differences in mortality (16.3% vs 10.9%; P=.049) and MI (13.9% vs 6.0%; P<.001), with conversely more stroke in the CABG group (2.4% vs 5.2%; P=.03). Interestingly, the greater benefit of CABG was consistent across all three SYNTAX tertiles.11 This was the first study which demonstrated favourable outcomes with one treatment strategy when considering the need for revascularization.
COMPLETE VERSUS INCOMPLETE REVASCULARIZATIONThe revascularization strategy depends to a certain extent on whether the aim is complete revascularization, functional revascularization, or purely for symptomatic benefit. Complete revascularization is more likely to occur with CABG and although this is the aim in the majority of patients with MVD, incomplete revascularization may be chosen in view of the presence of concurrent medical conditions, chronic total occlusions with no viability, or left ventricular systolic dysfunction. A recent meta-analysis of 37 116 patients with MVD who received either complete (n=11 596) or incomplete (n=25 520) revascularization demonstrated a lower risk of mortality (RR=0.82; 95%CI, 0.68-0.99; P=.05) and nonfatal MI (RR=0.67; 95%CI, 0.53-0.84; P<.01) with complete revascularization.15 Moreover, a substudy of the SYNTAX trial showed that a higher residual SYNTAX score was a marker of increasing clinical co-morbidity and anatomic complexity and a score >8 following revascularization was associated with a 35.3% mortality at 5 years, compared with 8.7% mortality with score 0-4 and 11.4% mortality with score 4-8 (P<.001).16
A number of studies aim to clarify the decision regarding complete versus incomplete revascularization and whether this should be anatomical or functional. The landmark study in the assessment of functional revascularization was the ‘Fractional Flow reserve versus Angiography for Multivessel Evaluation’ (FAME) study, which prospectively randomized 1005 patients with at least 2 vessels with >50% lesions to angiographic guided or fractional flow reserve guided procedures. There was a significant reduction in MACCE in the fractional flow reserve guided group (22.8% vs 14.9%; P=.02) and one third of angiographically deemed significant lesions were found not to be functionally significant by fractional flow reserve.17 It may therefore be that improved outcomes would be demonstrated in those with MVD undergoing perceived complete revascularization if this was done on a functional rather than anatomical basis. The fractional flow reserve measurement could be incorporated into the SYNTAX score, the so-called ‘functional SYNTAX score,’ and this has been evaluated in a pilot study.
THE PIVOTAL ROLE OF THE HEART TEAM IN MULTI-VESSEL CORONARY ARTERY DISEASEThe current European Guidelines emphasize the role of the ‘Heart Team,’ consisting of clinical cardiologists, interventional cardiologists, and cardiothoracic surgeons in order to decide upon the optimal therapeutic strategy for a patient with MVD.1 The ‘Heart Team’ decision should be taken considering both the clinical and anatomical characteristics of the patient with careful risk stratification. Hence, a tailored approach on a patient to patient basis, taking into account the goals of the therapy and expected quality of life improvement by considering individual preference and local expertise, is therefore recommended.
CONCLUSIONSThe majority of MVD studies demonstrate no significant differences between PCI and CABG in the hard endpoints of death, stroke, or MI, except in the subset of diabetes mellitus. Indeed, evidence suggests that PCI in selected patients can be performed not only safely but with comparable outcomes to CABG. Patients with MVD are complex and treatment should be tailored on an individual basis, taking into account both anatomical and clinical factors. Therefore, it is important to involve the patient in the decision-making process, following a discussion with the ‘Heart Team’.
The majority of previous studies have compared CABG with PCI with the first generation DES. New generation stents have subsequently been developed with encouraging results and require further assessment in this area. The ongoing ‘Bypass Surgery Versus Everolimus Eluting Stent Implantation for Multi-Vessel Coronary Artery Disease’ (BEST) study will attempt to answer some of these issues, randomizing 1776 patients with newer generation DES versus CABG with a primary composite endpoint of death, nonfatal MI and ischemia-driven target vessel revascularization at 2 years. In addition, the SYNTAX II multi-centre trial will include 450 all-comers with de novo 3-vessel disease without left main stem involvement following screening with the SYNTAX II score and the ‘Heart Team’. If patients are deemed suitable for PCI, following assessment with fractional flow reserve and iFR, the SYNERGY™ stent (Boston Scientific, Natick, Massachusetts, United States) will be used with a primary endpoint of MACCE at 12 months. In addition, more assessment will be performed of strategies such as hybrid revascularization, which may develop an increasing role in the future.
CONFLICTS OF INTERESTNone declared.