Because of the lack of scientific evidence on the effect of cardiovascular treatment on the infectivity of SARS-CoV-2 and on COVID-19 disease progression, the mechanisms that increase the risk of cardiac damage and thrombosis in patients with COVID-19, and the cardiotoxicity of antiviral treatment, we must consider the need for diagnostic tests that help health care professionals when making therapeutic decisions. Important aspects to consider are the following 5 points:
- 1.
Hypertension, diabetes, and cardiovascular disease are the most prevalent comorbidities in patients with COVID-19.1 Although they do not appear to affect the infectivity of the virus,2 they do increase disease severity. One of the common mechanisms of this effect is via the renin-angiotensin-aldosterone system. Their treatment reduces levels and activity of angiotensin II, as it contributes to inflammation and endothelial dysfunction. SARS-CoV-2 uses angiotensin-converting enzyme 2 (ACE2) and the protease TMPRSS2 to enter the host cell. ACE2 converts angiotensin II into an isoform with anti-inflammatory and vasodilator activity. It has not yet been ascertained whether the overexpression of tissue ACE2, in pathological states or induced by treatment, increases infection with SARS-CoV-2 or makes up for its deficiency to reduce cardiac, pulmonary, and renal inflammation and vasoconstriction. It is also necessary to study the regulation of serum ACE2 levels and its role in reducing the affinity of SARS-CoV-2 for tissue ACE2 and, consequently, infection (figure 1).
Figure 1.Representation of the importance of angiotensin-converting enzyme 2 (ACE2) and the protease TMPRSS2 for the initial infection with SARS-CoV-2. Polymorphisms of ACE2 or soluble ACE2 may affect its cell binding. The increase in tissue expression of ACE2 may increase the infectivity or have a protective effect, converting angiotensin II to angiotensin (1-7). Ang, angiotensin.
(0.32MB). - 2.
Determination of the genetic variants of ACE2 in the population could identify which group has least risk of infection with SARS-CoV-2. Of particular interest would be those described as being associated with essential hypertension (rs2074192) and atrial fibrillation (rs4240157, rs4646155, rs4830542).3 The variants SLCO1B1 and BDKRB2,4 associated with patients with toxicity from angiotensin-converting enzyme inhibitors and with symptoms similar to COVID-19, could also be used to exclude false positives.
- 3.
A high percentage of patients with COVID-19 have cardiac events while in hospital. Therefore, there is a strong need for plasma markers of cardiac damage such as high-sensitivity cardiac troponin I or lactate dehydrogenase and markers of cardiac function.
- 4.
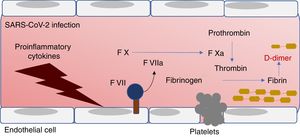
There is also a high prevalence of macrovascular and microvascular thrombotic events in patients with COVID-19. High concentrations of D-dimer, a protein degradation product of coagulation, have been shown to be predictors of mortality.5 However, determination of markers in the initial phase of coagulation could alert to cardiovascular, cerebrovascular, pulmonary, and renal events. We must not forget that ACE2 is expressed in the endothelium and its activation by proinflammatory cytokines triggers the production of tissue factor, platelet adhesion, and activation of the clotting cascade (figure 2).
- 5.
The treatments used in patients with COVID-19 are based on reducing viral reproduction and inflammation (such as 4-aminoquinolone antimalarial agents). However, these drugs could cause cardiotoxicity, with systolic dysfunction and prolongation of the QT interval.6 Therefore, early markers are required to prevent irreversible cardiotoxicity.
In conclusion, the preventative and therapeutic strategies for COVID-19 will improve with markers that identify those patients with greater pathological, genetic or pharmacological susceptibility to infection with SARS-CoV-2 (ACE2 regulation) and that monitor the mechanisms involved in disease progression (cardiac damage, thrombosis, and cardiotoxicity).
.