Keywords
INTRODUCTION
The ostium secundum atrial septal defect (OSASD) is an abnormal opening that requires early closure because of the anatomical and hemodynamic changes it produces in right ventricle and the pulmonary arterial bed.1 Percutaneous closure using the Amplatzer occluder has proved to be an effective therapeutic alternative since 1997.2-5 For the proper implantation of the device, the echocardiographic image must show that it is positioned transversely to the rim of the defect. The perpendicular positioning of the Amplatzer occluder over the rim of the defect, reported as far back as the earliest studies, impedes its self-centering capacity and correct implantation.2,3 This complication has been recorded in 7% of the cases and can lead to excessive manipulation of catheters, embolization and the failure of the procedure.3-8 Here, we describe an ancillary technique involving a balloon catheter that prevents the failure of defect closure resulting from the perpendicular positioning of the occluder device.
METHODS
Echocardiographic images corresponding to six patients revealed that the occluder device (Amplatzer AGA Medical Corporation, Golden Valley, Minnesota) was persistently positioned perpendicular to the rim of the defect, complicating the procedure and, thus, its implantation. The patients were accepted for percutaneous closure of the defect, during a session involving medical and surgical personnel from the cardiology and cardiac surgery departments, in accordance with the guidelines established in the medical literature.2-8 We recorded their age, sex and weight, as well as the diameter and rim of the defect, determined by transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE).
The hemodynamic study carried out prior to closure of the septal defect provided information on blood oxygen saturation and superior vena cava, inferior vena cava, right atrial, left atrial, pulmonary vein, right ventricular and main pulmonary artery pressures, the pulmonary to systemic flow ratio (Qp:Qs) and pulmonary vascular resistance.
Conventional Technique
The continuous electrocardiographic recording was performed using 1 bipolar lead (II) and 1 unipolar lead (V5) and arterial blood pressure was recorded with a wrist sphygmomanometer. The patients were sedated with fentanyl citrate (1 µg/kg body weight [BW]) and midazolam hydrochloride (100 µg/kg BW). Heparin (100 IU/kg BW) and cephalothin (100 mg/kg BW) were administered. The diagnosis was verified and the OSASD rim assessed by means of TEE. The Seldinger technique was employed for femoral vein access, and a multipurpose catheter was advanced to left upper pulmonary vein. The four-chamber view of the heart was obtained by means of contrast echocardiography using Optiray 350 (1 mL/kg BW), which was injected into right upper pulmonary vein to enable the determination of the diameter of the OSASD and assessment of the arteriovenous shunt flow. The size of the device to be employed was determined on the basis of the stretched diameter of the defect using a Meditech balloon (Boston Scientific, Watertown, Massachusetts), in agreement with the sizing plate of the device (AGA Medical) and with the size of the defect estimated by means of echocardiography.
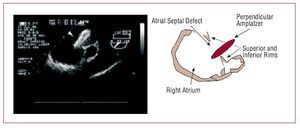
The release system was advanced until it crossed the OSASD into the left atrium; once the occluder was loaded, a conventional technique was employed to advance the device through the release system toward the heart. During fluoroscopy, the expansion of the left disc and part of the waist was initiated within the left atrium, after which the device was pulled towards the right atrium. The transverse position was ensured under TEE guidance, as were the attachment and self-centering of the device over the rim of the defect. However, in the six cases reported here, the position was persistently perpendicular, and the left disc was located on the posteroinferior margin of the septal defect, without achieving self-centering (Figure 1). After three attempts to rotate and free the device, we employed the balloon-assisted technique.
Figure 1. Transesophageal echocardiographic (TEE) image showing the Amplatzer device located on the inferior rim of the atrial septal defect. The diagram to the right represents the TEE image.
Alternative Balloon-Assisted Technique
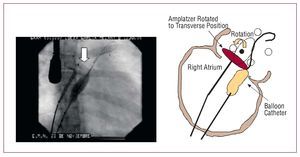
A 24-mm sizing balloon catheter (AGA Medical Corporation) was introduced through a contralateral femoral vein access. It was drawn across the OSASD and its distal end was advanced to the orifice of left upper pulmonary vein. The balloon was then inflated with a mixture of 1 mL of saline solution and 3 mL of contrast medium, and was positioned at the lower rim of the defect. The inflated balloon provided transient support to the lower edge of the Amplatzer occluder and the deployment of the device was initiated. The transverse position and self-centering of the occluder were achieved (Figure 2) and its discs were correctly attached on either side of the septal rim, ensuring the successful closure of the OSASD (Figure 3).
Figure 2. Fluoroscopic image showing the maneuver in which the balloon lends support to the lower edge of the Amplatzer device to correct the perpendicular position to a transverse position. The diagram to the right represents the fluoroscopic image.
Figure 3. Transesophageal echocardiographic (TEE) image showing the discs of the Amplatzer device attached to either side of the septal defect rim. The arrow indicates the device closing the atrial septal defect. The diagram to the right represents the TEE image.
RESULTS
Of 58 patients who underwent percutaneous closure of an OSASD, the procedure had to be suspended in five cases due to a posteroinferior margin of less than 5 mm, as determined by TEE during the procedure. In eight cases, echocardiographic images revealed that the device had remained perpendicular to the rim of the defect; in the first 2 cases, defect closure was unsuccessful, whereas in the remaining 6, the balloon-assisted technique was performed and closure was achieved.
The ages and weights of the patients ranged between 2 and 26 years and 11 and 72 kg, respectively. The sizes of the OSASD ranged from 16 to 28 mm according to TTE and from 16 to 26 mm according to TEE. The measurements of the rims of the defects ranged as follows: posterior, 4-11 mm; aortic, 2-5 mm; inferior vena cava, 5-7 mm; and superior vena cava, 5-14 mm. The diameters of the devices implanted ranged between 18 and 32 mm (Table 1).
The hemodynamic study demonstrated that all the patients presented normal blood oxygen saturation and right heart chamber and pulmonary pressures. The pulmonary to systemic flow ratio (Qp:Qs) and pulmonary vascular resistance were adequate for closure of the defect (Table 2).
DISCUSSION
Percutaneous closure of OSASD in humans was initially performed with rigid, difficult to manage devices.9-11
Technological advances and medical creativity led to the development of occluders, introducing improvements in the design and materials of which they are made. The Amplatzer device consists of a single component with 2 retention discs, joined by a waist that makes it possible to expand and retrieve the discs as many times as necessary until proper self-centering and implantation is achieved.12-20
At this point, the technique for the implantation of the Amplatzer device for OSASD closure has been standardized, and its practice is safe and effective in most tertiary care hospitals; however, in some cases, the incorrect position of the device over the rim of the defect impedes its successful implantation. In some series, the perpendicular position of the device over the margins of the defect is reported in 7% of the cases,2,3 making it necessary to repeat the attempted implantation several times. This leads to excessive manipulation of catheters and maneuvers that increase the risks of perforating cardiac chambers, tearing the septal margins, embolization and failure of the procedure.12-20 In our series, we observed an incidence of 13%, although we should consider the number of patients to be low with respect to other published series.
During the maneuver to release the first disc of the device, the disc must attach to the inferolateral margin of the defect to favor the transverse position of the device over the rim of the defect, as observed in TEE images, and thus enable its self-centering, an indispensable condition for its implantation. A number of authors mention the incorrect position of the device over the septal rim, and they correct it by means of rotational maneuvers during the sequence in which the device is expanded. However, these maneuvers involve risks of embolization and perforation of the cardiac tissue.21-29 Kannan et al26 and Wahab et al27 indicate that cutting the Mullins sheath makes it possible to achieve the proper angulation of the device and the perpendicular position is corrected, although, during the implantation process, it increases the risk of air embolism and of vascular lesion upon introduction of the cut sheath. It is remarkable that, despite there being over 100 published cases, this correction technique has not produced either of these complications.29
Certain factors contribute to the anomalous position of the device over the OSASD, one of the most common of which is the presence of an inadequate posteroinferior rim.30 Varma et al31 reported that the failure of the implantation of the device due to incorrect positioning occurs when the inferior rim is unable to support the device, especially if it is combined with a small anterior rim. In four of our cases, the aortic rim measured 3 mm or less and, although the inferior rims were of adequate size, reduced tension in the tissue may have resulted in a lack of sufficient support for the device, increasing the likelihood of it adopting a perpendicular position over the septal defect.27-30 In addition, Dalvi et al30 pointed out that the presence of a small left atrium can lead to the poor position of the device since it does not permit the rotation of the disc within the posterior curvature of the atrium at the level of the pulmonary veins or anteriorly because of the atrial appendage. This may have been the cause of the persistent perpendicular position of the device in some of our cases (in patients 1, 4, and 5), as they presented small septal defects and rims.
In the Catheterization Laboratory for Congenital Heart Diseases at Centro Médico Nacional 20 de Noviembre of the Instituto de Seguridad y Servicios Sociales de los Trabadajores del Estado (ISSSTE; Government Workers´ Social Security and Services Institute, Mexico), in the first 2 cases of perpendicular positioning of the Amplatzer occluder, observed in sagittal plane TEE images, we carried out the maneuvers described by other authors, with excessive manipulation of the catheters and of the occluder,25-29 but the incorrect position of the device persisted and, consequently, the OSASD closure was unsuccessful. In the remaining 6 cases, we employed the balloon-assisted technique, which proved to be useful and enabled us to achieve the transverse position, with self-centering of the device and successful closure of the OSASD.
The technique, in which a balloon is employed to support the inferolateral edge of the device, described by Masura et al,2 Dalvi et al,30 and Varma et al31 adds the inconvenience of having to employ another femoral access, with the risk of complications in the process of puncture and the introduction of the balloon catheter. Fortunately, these authors reported no complications, nor did we observe them in our experience. We consider these risks to be minor when compared with the risks of thromboembolism, perforation of cardiac structures and tearing of the septal margins secondary to the excessive manipulation of the catheters that is required with other techniques utilized to correct the improper position of the device over the OSASD rim.12,19-22
The balloon-assisted technique is useful for correcting the poor positioning of the Amplatzer device, but we do not know if it could be applied to other types of devices. The number of patients in whom this technique has been applied is small and it can not be compared with other techniques described in the literature. Nonetheless, it may represent a better alternative since, in the published series and in our experience, no complications have been observed.
CONCLUSIONS
The balloon-assisted technique is a useful and feasible alternative for the percutaneous closure of OSASD when echographic images demonstrate the Amplatzer device to be persistently orientated perpendicular to the rim of the septal defect.
ABBREVIATIONS
OSASD: ostium secundum atrial septal defect
TEE: transesophageal echocardiography
TTE: transthoracic echocardiography
Correspondence: Dr. J.L. Aceves Chimal.
Laboratorio de Intervencionismo en Cardiopatías Congénitas. Avda. Félix Cuevas, 540. Col del Valle CP 03100, México.
E-mail: aceves996@hotmail.com
Received July 25, 2007.
Accepted for publication March 6, 2008.