This document summarizes the concept of focused cardiac ultrasound, the basic technical aspects related to this technique, and its diagnostic objectives. It also defines training requisites in focused cardiac ultrasound. This consensus document has been endorsed by the Spanish Society of Internal Medicine (SEMI), the Spanish Society of Family and Community Medicine (semFYC), the Spanish Society of Neurology (SEN), and the Spanish Society of Cardiology (SEC).
Keywords
With the advent of hand-carried devices, ultrasound has evolved from a bedside procedure into an essential mobile imaging test in several specialties.1 In recent years, the term “focused cardiac ultrasound” has been introduced to describe the use of ultrasound by the treating physician to complement the standard cardiac physical examination. This application of ultrasound is diagnostically valuable and has a relatively short theoretical and practical learning curve.2 The fundamental characteristics of focused cardiac ultrasound are as follows:
- •
The technique serves to guide the diagnosis of a specific and clinically important problem. It should be integrated into the decision tree and guide the physician in patient diagnosis and treatment.3
- •
It is indicated in specific clinical situations, mainly defined by patient symptoms (eg, dyspnea, chest pain) and the clinical setting (eg, critical patient, medical emergency, asymptomatic patient).
- •
It is a limited (nonexhaustive) technique, uses fewer slices than a complete study, and its main goal is to provide a high negative predictive value. Focused cardiac ultrasound generally does not require the technical specifications of more advanced equipment (pulsed, continuous, and tissue Doppler, etc.).
- •
It is fast and repeatable, and can thus be used to analyze the clinical course of defined parameters related to the patient's condition.
- •
Focused cardiac ultrasound can be used by any physician who has completed the necessary theoretical and practical training.4 To obtain the maximum benefit, it is essential to first review the patient's medical history and conduct a physical examination, in order to propose a reasonable differential diagnosis.
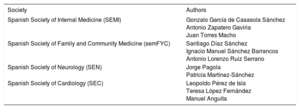
In Spain, cardiologists and other specialists have increasingly incorporated focused cardiac ultrasound into their daily clinical practice,4-11 creating the need for a consensus on its use among the various scientific societies affected. To this end, the present document has been prepared by a joint committee of the Spanish Society of Internal Medicine (Sociedad Española de Medicina Interna, SEMI), the Spanish Society of Family and Community Medicine (Sociedad Española de Medicina Familiar y Comunitaria, semFYC), the Spanish Society of Neurology (Sociedad Española de Neurología, SEN), and the Spanish Society of Cardiology (Sociedad Española de Cardiología, SEC) (Table 1).
Author Membership of the Endorsing Scientific Societies
| Society | Authors |
|---|---|
| Spanish Society of Internal Medicine (SEMI) | Gonzalo García de Casasola Sánchez Antonio Zapatero Gaviria Juan Torres Macho |
| Spanish Society of Family and Community Medicine (semFYC) | Santiago Díaz Sánchez Ignacio Manuel Sánchez Barrancos Antonio Lorenzo Ruiz Serrano |
| Spanish Society of Neurology (SEN) | Jorge Pagola Patricia Martínez-Sánchez |
| Spanish Society of Cardiology (SEC) | Leopoldo Pérez de Isla Teresa López Fernández Manuel Anguita |
Focused cardiac ultrasound is the limited and targeted use of echocardiography as an extension of the physical examination by cardiologists or noncardiologist physicians. As such, its goal is to improve the diagnostic, prognostic, and therapeutic evaluation obtained during the standard physical examination.12 As with other imaging techniques, it is essential to establish an agreed training and accreditation program that equips operators with the skills they need to carry out the procedure.
When using focused cardiac ultrasound, it is important to keep in mind the following guiding principles7:
- 1.
Focused cardiac ultrasound is not a substitute for a complete echocardiographic examination.
- 2.
Patients should be informed about the limitations of the technique and the possible need to extend the study to a complete echocardiographic examination.
- 3.
The procedure is indicated for the detection of defined cardiac abnormalities specified in the scientific literature and in the training and accreditation program, with the aim of helping the physician to make an accurate diagnosis.
- 4.
As with the physical examination, focused cardiac ultrasound studies should be assessed within the context of the patient's medical history. This assessment can never take the place of a full echocardiographic evaluation, and should be restricted to the parameters outlined in this document.
- 5.
As with any other imaging technique, it is essential for operators to undergo specific, accredited training in order to ensure the quality and reliability of the results.
- 6.
When focused cardiac ultrasound detects abnormalities suggesting heart disease or produces inconclusive results, the patient should undergo a complete echocardiographic examination.
- 7.
To ensure quality control focused cardiac ultrasound operators should be supervised by an accredited echocardiography laboratory linked to their institution.
Information related to the diagnostic goals of focused cardiac ultrasound can be obtained with a low number of views (Table 2). Nonetheless, to ensure correct patient evaluation, good image quality should generally be obtained in at least 2 views.4,13–21 The most useful are the parasternal longitudinal view and 4-chamber apical views because they allow the evaluation of multiple cardiac structures and the diagnosis of disease.
Training Objectives in Focused Cardiac Ultrasound and Common Clinical Settings in Which They Can Be Achieved
| Training objective | Clinical setting | Skills and applications |
|---|---|---|
| Acquisition of essential ultrasound views and measurement of heart chambers | Evaluation of patients with X-ray-detected cardiomegaly Evaluation of left ventricular dilatation in patients with idiopathic stroke All patients with an indication for focused cardiac ultrasound | Basic ultrasound views: parasternal long and short axis; 4-,3-and 2-chamber apical; and subcostal It is useful to measure the size of the ventricles, atria (area and volume), interventricular septum, ascending aorta, and vena cava |
| LVEF estimation | Evaluation of patients with dyspnea Evaluation of hemodynamically unstable patients Evaluation of patients with abnormalities on the ECG or chest X-ray Evaluation of patients with cardioembolic stroke Comprehensive evaluation of patients at high cardiovascular risk | To strengthen diagnosis of ventricular systolic dysfunction, an indirect parameter can be included, such as LV telediastolic diameter or MAPSE Detection of the absence of mechanical activity during cardiopulmonary resuscitation |
| Evaluation of RV function and estimation of RV pressure or volume overload | Evaluation of patients with dyspnea Evaluation of patients with suspected pulmonary embolism Evaluation of patients with hypotension or shock Screening for pulmonary hypertension | Estimation of right chamber dimensions, vena cava size, RD:LV ratio in 4-chamber apical view, and RV thickness in subcostal view Operators can include visual evaluation of RV systolic function and TAPSE as a quantitative measure of general RV function |
| Detection of significant valve disease | Initial evaluation of patients with dyspnea Initial evaluation of patients with suspected heart failure Evaluation of patients with hypotension or shock Evaluation of patients with significant heart murmur in the physical examination Evaluation of patients with cardioembolic stroke | The goal is to identify when a valve lesion could be related to the patient's clinical status If focused cardiac ultrasound indicates suspected valve disease or related uncertainty, the patient should undergo a complete echocardiographic study |
| Detection of pericardiac effusion and identification of patients with cardiac tamponade | Evaluation of patients with dyspnea Evaluation of patients with hypertension or shock Evaluation of patients with X-ray-detected cardiomegaly Patients with acute pericarditis | Operators will be able to identify the presence of pericardiac effusison and discern whether this has repercussions on the heart chambers (chamber collapse, swinging heart syndrome) Practioners must recognize that the indication for emergency pericardiocentesis is the patient's clinical and hemodynamic status and not the focused cardiac ultrsound findings |
| Estimation of LVH and suspected diastolic dysfunction | Evaluation of patients with dyspnea Suspicion of hypertensive heart disease Comprehensive evaluation of patients at high cardiovascular risk | For patients with dyspnea on exertion in whom focused cardiac ultrasound shows marked ventricular wall thickening and left ventricular dilatation |
| Evaluation of blood volume | Hypotension or shock | Evaluation of the presence or absence of chamber dilatation and inferior vena cava diameter and collapsibility |
| Detection of aortic plaques and cardiac masses | Evaluation of patients with embolic stroke | Aortic or valve plaques and cardiac masses that require confirmation in a complete echocardiographic study |
ECG, electrocardiogram; LV, left ventricle; LVEF, left ventricular ejection fraction; LVH, left ventricular hypertrophy; MAPSE, mitral annular plane systolic excursion; RV, right ventricle; TAPSE, tricuspid annular plane systolic excursion.
As with other imaging techniques, it is advisable to systematize the sequence for acquiring views and the essential information sought in each one.22 Videos and images should be stored so that the findings can be reviewed and confirmed, increasing the degree of competence in complex cases with a study review by expert echocardiographers.4
DIAGNOSTIC GOALSThe diagnostic goals of focused cardiac ultrasound are closely aligned with those of complete echocardiographic studies and are influenced by the technique's relatively short learning curve and its usefulness in clinical practice. The goals outlined here are based on key studies conducted with diverse methodologies and varying levels of evidence, as well as the consensus documents of several scientific societies (Table 2).
Left Ventricular Systolic FunctionFocused cardiac ultrasound provides a visual estimate of left ventricular size and overall systolic function at an acceptable level of agreement with quantitative methods. Moreover, from a clinical standpoint, it is sufficient to distinguish between normal function and dysfunction.4,6,13,18,19,23–33
Quantification of ejection fraction falls outside the scope of focused cardiac ultrasound. Nonetheless, left ventricular systolic function can be assessed visually, especially from the 4-chamber view, which can be used to obtain a semiquantitative estimate by applying the following classification system: normal, probably reduced, and severely reduced. Another semiquantitative parameter that can provide an index of systolic function is mitral annular plane systolic excursion (MAPSE).34-39 However, the use of annular plane systolic excursion is limited; in particular, it cannot be used in patients with mitral valve calcification.
Detection of Pericardial Effusion Suspected TamponadeUltrasound is the method of choice for the diagnosis of pericardial effusion. Numerous studies have demonstrated the ability of “noncardiologists” to detect pericardial effusion in different clinical settings (eg, shock, electromechanical dissociation, X-ray detected cardiomegaly, patients on hospital wards). It is important to emphasize that tamponade is diagnosed clinically from a constellation of symptoms including hypertension, tachycardia, and elevated venous pressure; ultrasound findings such as significant pericardial effusion, right heart collapse, and swinging heart syndrome serve to confirm the clinical diagnosis.40–45
Estimation of Heart-chamber DimensionsFocused cardiac ultrasound is a relatively straightforward way to screen for structural cardiac alterations such as left ventricular dilatation,2,44 moderate-to-severe left ventricular hypertrophy,43,46 or dilatation of the left atrium29,44,45,47,48; the information obtained can make a major contribution to the comprehensive evaluation of patients with cardiovascular disease.21,49–52 Focused cardiac ultrasound can also be used to evaluate other structures, such as the ascending aorta.53
Evaluation of Right Ventricular Size and FunctionDespite the complexity of right ventricular abnormalities, focused cardiac ultrasound can be used for the subjective detection of right ventricular dysfunction and a dilated right ventricle, principally based on the finding of a right-to-left ratio of the ventricular telediastolic diameters > 1 in the apical 4-chamber view.19,23 The measurement of tricuspid annular plane systolic excursion (TAPSE) is a relatively simple and reproducible method that provides prognostic information in clinical settings such as heart failure and acute pulmonary embolism.54
Evaluation of the right ventricle is probably of most value in patients in shock or with pulseless electrical activity and suspected massive pulmonary thromboembolism. In noncritical patients, right ventricle parameters are of less significance.55,56
Estimation of Inferior Vena Cava Diameter and CollapsibilityIn spontaneously ventilated patients, noncardiologists have a proven ability to determine blood volume and, indirectly, central venous pressure from ultrasound estimates of the diameter and collapsibility of the inferior vena cava. It is nonetheless important to be aware of the many factors that can influence these estimates.57 This application of focused cardiac ultrasound can be used to identify patients who require “volume repositioning” when the vena cava diameter is decreasing and the collapsibility index is > 50%.57-59 In patients on invasive or noninvasive mechanical ventilation, the parameters for evaluating the inferior vena cava should be interpreted with caution.16,60–65
Detection of Significant Heart-valve AbnormalitiesThe detection of heart-valve abnormalities is a frequent and feasible application of focused cardiac ultrasound that can be used as a screening method.43,51,66–70 The early detection of severe valve lesions in shock or heart-failure patients can speed up diagnosis and therapy, with positive repercussions on morbidity and mortality.71–73 The use of quantitative methods such as blood flow velocity analysis to estimate the severity of valve lesions falls outside the scope of focused cardiac ultrasound.4 Nonetheless, operators should be able to visually identify decreases in valve aperture and the presence of regurgitation from color Doppler ultrasound. Although focused cardiac ultrasound cannot quantify the severity of valve disease, it can be used to classify valve lesions into levels: absence, trivial or minimal, and severe. When this approach detects valve lesions that appear to be more than mild, the patient should undergo a conventional echocardiographic examination.
Other Diagnostic PossibilitiesFocused cardiac ultrasound can detect segmentary contraction abnormalities in the left ventricle, cardiac masses, thrombi, vegetations, or signs of aortic dissection, such as the presence of a dilated ascending aorta or significant pericardial effusion in a patient with chest pain, stroke, or syncope. These applications require a sufficient level of experience. Obviously, these findings should be confirmed by a complete echocardiographic study unless this is not available and a therapeutic decision needs to be taken immediately. The failure to detect these abnormalities by focused cardiac ultrasound does not exclude their diagnosis.5,53
The parameters that can be evaluated by focused cardiac ultrasound are applicable to many clinical settings, some of them common and others characteristic of a specific specialty. These clinical settings are listed in Table 2.
TRAINING AND SKILL ACQUISITION IN FOCUSED CARDIAC ULTRASOUNDRegulated training and accreditation exists to ensure that physicians acquire the skills needed to complete the procedures they are tasked with performing. Accreditation in any activity, and specifically in imaging techniques, is of the utmost importance in ensuring that the professional using the technique is equipped with the knowledge and skills needed to carry out the study, in terms of both image acquisition and interpretation. These concerns are reflected in the central recommendation of this consensus document endorsed by the SEC, SEMI, SEN, and semFYC: focused cardiac ultrasound studies must be performed in accordance with qualtity-control and accreditation criteria in order to guarantee the best care and maximum benefit for the patient.
Numerous studies published in recent years have proposed different training routes in focused cardiac ultrasound and the number of training hours needed to achieve specific objectives.18,29,31,42–44,49,51,69,70,74–77 After an initial basic training in theory and practice, skills can be acquired progressively through experience at the patient bedside.42,49,78
There is no agreed consensus on the training needed to attain a basic level of competence in focused cardiac ultrasound; however, several studies concur in recommending at least 50hours of supervised real-world training with patients in a variety of clinical situations.4,5,23,49,76 To achieve this, it is essential to organize training in coordination with the cardiology service.5 After completing their training, noncardiologists should incorporate focused cardiac ultrasound into their daily clinical practice; within a few months they will have acquired experience in evaluating patients with very diverse cardiac lesions.76 This approach will give operators the optimal competence level suited to the specific requirements of their specialty (emergency medicine, internal medicine, vascular neurology, primary care, telemedicine, etc.).5,13,79,80
The SEC, SEMI, SEN, and semFYC have designed a training program in focused cardiac ultrasound that includes online theoretical instruction and a practical training course in which the trainee must carry out a minimum of 50 supervised real-world patient studies. Accreditation is conditional on successful completion of an objective practical evaluation. After completing their training, newly accredited focused cardiac ultrasound practitioners are strongly advised to maintain contact with echocardiography laboratories in the cardiac imaging units. This will facilitate consultations about ultrasound images and patient diagnosis and will also aid decision-making about which patients require a complete echocardiography study.
CONCLUSIONSFocused cardiac ultrasound is an invaluable diagnostic tool that complements physical examination in patients with cardiovascular disease. This technique can also be used for prognostic stratification and follow-up.
The uptake and expansion of focused cardiac ultrasound is to be encouraged due to its benefits for patients; however, its widespread use requires proper training and accreditation for operators.
CONFLICTS OF INTERESTNone declared.
.