Patients who have undergone angioplasty with stenting can be reintegrated into normal life at an early stage, thanks to the absence of sequelae associated with the procedure itself. Consequently, these patients can be involved earlier in the second stage of cardiac rehabilitation. Although rehabilitation for coronary patients follows the general guidelines used for all patients, which were developed with the secondary prevention of coronary artery atherosclerosis in mind, the specific form of rehabilitation adopted for each individual with ischemic heart disease will depend on the patient's circumstances, including the revascularization technique used. Regular physical exercise (i.e. physical training), in itself, has substantial cardiovascular benefits for both primary and secondary cardiovascular prevention. In patients who have had a myocardial infarction, training decreases mortality, increases functional capacity and improves ventricular function and remodeling. It is also thought to boost the collateral circulation. In addition, training improves endothelial function and stimulates the circulation of stem cells. It has been shown that physical training after percutaneous revascularization decreases the number of cardiac events. Moreover, in patients with stable angina, it results in fewer events than percutaneous revascularization.
Keywords
The guidelines of the European Society of Cardiology (ESC) are endorsed by the Spanish Society of Cardiology (SEC). Since 2011, the publication of the translation of the guidelines in Revista Española de Cardiología has been accompanied by a critical review article that is written by a group of authors coordinated by the SEC Guidelines Committee.1
This article discusses the 2015 ESC guidelines for the management of non–ST-segment elevation acute coronary syndromes (NSTEACS).2 The Guidelines Committee designated a working group composed of members nominated by the SEC and the Spanish Society of Thoracic and Cardiovascular Surgery. The document was divided into parts that were sent to the members of the working group and, based on their comments, a manuscript was written and reevaluated by the group and by reviewers proposed by the SEC Working Group on Ischemic Heart Disease and Acute Cardiovascular Care.
GENERAL COMMENTS ON THE METHODOLOGYThe recommendations of the guidelines are summarized in tables that include: a) the class of recommendation, depending on whether there is evidence or agreement that a treatment or procedure is indicated (class I), should be considered (class IIa), may be considered (class IIb) or is not recommended (class III); b) the level of evidence, which can consist of multiple clinical trials or meta-analyses (level of evidence A), a single trial or large nonrandomized studies (level of evidence B), or expert consensus or small studies (level of evidence C); and c) literature references. Sixteen Tables are presented with 134 recommendations, less than two thirds of which are categorical (79 in class I, 8 in class III) and 40% are supported by level of evidence C, showing that there remain areas of uncertainty in the management of these patients.
One new feature is the inclusion of extensive supplementary material in an online Appendix, as well as a series of questions and responses taken from case reports, which will be useful to clarify concepts that appear in the guidelines.
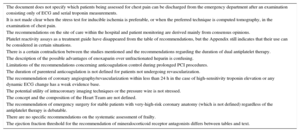
SUMMARY OF THE MAJOR SECTIONS OF THE GUIDELINESIn the present article, Table 1 summarizes the most relevant or novel aspects and Table 2, the most debatable aspects, according to the working group.
The Most Novel or Relevant Aspects of the 2015 ESC Guidelines for Non–ST-segment Elevation Acute Coronary Syndromes
| Definitions, pathophysiology and epidemiology |
| • The universal definition for acute myocardial infarction is adopted. |
| Diagnosis |
| • An ultrarapid algorithm for the evaluation of chest pain, based on 2 determinations of high-sensitivity troponin separated by 1 h, is introduced, and the previous algorithm, involving 2 determinations separated by 3 h, remains in use (I-B) . |
| Risk assessment and outcomes |
| • Formal risk assessment with standardized scoring systems continue to be recommended (I-B). The class of recommendation of the CRUSADE score calculation has been lowered to IIb-B. |
| • The recommended hospital unit to which the patient should be admitted is indicated (I-C). |
| • It is recommended that all the patients with NSTEACS be admitted to a monitored unit (I-C). |
| Platelet inhibition |
| • The recommendation of ticagrelor is maintained, in the absence of contraindications, for patients with intermediate-to-high risk for ischemic events, regardless of the initial management strategy (I-B). |
| • The recommendation of prasugrel is maintained for patients with known coronary anatomy, and PCI is indicated (I-B). Clopidogrel is still recommended for patients who need oral anticoagulation but cannot take ticagrelor or prasugrel (I-B). |
| • The recommended duration of dual antiplatelet therapy in the absence of contraindications is 12 months (I-A); shortening or prolonging it could be considered, depending on the ischemic and bleeding risk (IIb-A). |
| • If P2Y inhibitor discontinuation is necessary, it can be considered no sooner than 1 month after implantation of a bare-metal stent and no sooner than 3 months after implantation of a new-generation drug-eluting stent (IIb-C). |
| • The use of GPIIb/IIIa inhibitors is restricted to the catheterization laboratory and in specific situations (IIa-C). Its use prior to coronary angiography is contraindicated (III-A). |
| • Cangrelor is now recommended as a rapid-acting, and very transient, intravenous antiplatelet agent (IIb-A). |
| Anticoagulation |
| • The doses of parenteral anticoagulants are given for patients with normal renal function and renal failure. |
| • Both enoxaparin and unfractionated heparin are class I-B recommendations when fondaparinux is not available. |
| • The class I-B recommendation of bivalirudin for patients with high bleeding risk, and indication for an urgent or early invasive strategy, has been deleted. |
| • The use of rivaroxaban (IIb-B), together with aspirin and clopidogrel, can be considered for patients without a history of stroke or transient stroke and are at high ischemic risk and low bleeding risk, after interruption of parenteral anticoagulation. |
| Management of antiplatelet therapy in patients receiving oral anticoagulation |
| • For the first time, a specific section is included for patients of this type. |
| • There is consensus on the benefit of anticoagulation therapy at discharge for most patients, but the duration of triple therapy should be minimized. |
| • The use of the new antiplatelet agents, ticagrelor and prasugrel, is not recommended as part of triple therapy (III-C). |
| • The duration of dual antiplatelet therapy can be shortened with the third-generation drug-eluting stents (IIb-A). |
| Management of acute bleeding complications |
| • A series of strategies to reduce bleeding risk in patients undergoing PCI is described. |
| • The Appendix provides general measures and practical recommendations for the management of bleeding and the treatment of bleeding associated with different drugs; prothrombin complex is often recommended. |
| • Recommendations to restrict transfusions (IIb-C) for anemic patients (hematocrit < 25% or hemoglobin < 7 g/dL). |
| Invasive coronary angiography and revascularization |
| • Patients are classified into 4 risk categories with different timings for the invasive strategy: immediate (< 2 h), early (< 24 h), delayed (< 72 h) or elective (I-A/I-C). |
| • Clear recommendations are given on antiplatelet therapy before and after surgical revascularization. |
| • Radial access is recommended for coronary angiography at experienced centers (I-A). |
| • The new-generation drug-eluting stents are recommended (I-A). |
| • The consideration of the new-generation drug-eluting stents as an alternative to bare-metal stents is accepted for patients scheduled to receive dual antiplatelet therapy for no longer than 1 month (IIb-B). |
| • For patients with multivessel disease, it is recommended that the revascularization strategy be chosen according to the clinical and angiographic features and in accordance with the protocol of the local Heart Team (I-C). |
| Special populations and conditions |
| • The section on sex-specific management of the patients has been deleted. |
| Long-term management |
| • The consideration of the addition of a second lipid-lowering drug (ezetimibe) is recommended if LDL-C is ≥ 70 mg/dL with the maximum tolerated statin doses (IIa-B). |
| ESC, European Society of Cardiology; GP, glycoprotein; LDL-C, low-density lipoprotein cholesterol; NSTEACS, non–ST-elevation acute coronary syndrome; PCI, percutaneous coronary intervention. |
Debatable Aspects of the 2015 ESC Guidelines for Non–ST-segment Elevation Acute Coronary Syndrome
| The document does not specify which patients being assessed for chest pain can be discharged from the emergency department after an examination consisting only of ECG and serial troponin measurements. |
| It is not made clear when the stress test for inducible ischemia is preferable, or when the preferred technique is computed tomography, in the examination of chest pain. |
| The recommendations on the site of care within the hospital and patient monitoring are derived mainly from consensus opinions. |
| Platelet reactivity assays as a treatment guide have disappeared from the table of recommendations, but the Appendix still indicates that their use can be considered in certain situations. |
| There is a certain contradiction between the studies mentioned and the recommendations regarding the duration of dual antiplatelet therapy. |
| The description of the possible advantages of enoxaparin over unfractionated heparin is confusing. |
| Limitations of the recommendations concerning anticoagulation control during prolonged PCI procedures. |
| The duration of parenteral anticoagulation is not defined for patients not undergoing revascularization. |
| The recommendation of coronary angiography/revascularization within less than 24 h in the case of high-sensitivity troponin elevation or any dynamic ECG change has a weak evidence base. |
| The potential utility of intracoronary imaging techniques or the pressure wire is not stressed. |
| The concept and the composition of the Heart Team are not defined. |
| The recommendation of emergency surgery for stable patients with very-high-risk coronary anatomy (which is not defined) regardless of the antiplatelet therapy is debatable. |
| There are no specific recommendations on the systematic assessment of frailty. |
| The ejection fraction threshold for the recommendation of mineralocorticoid receptor antagonists differs between tables and text. |
ECG, electrocardiogram; ESC, European Society of Cardiology; PCI, percutaneous coronary intervention.
The guidelines adopt the universal definition of acute myocardial infarction (AMI). For troponin measurement, high-sensitivity methods are recommended over conventional approaches because of their higher negative predictive value for AMI and because they facilitate an earlier diagnosis. Of the remaining biomarkers, the guidelines mention only creatine kinase MB fraction, which can aid in estimating the timing of myocardial injury and detect early reinfarction, and copeptin, a marker of endogenous stress that may have added value in enabling the early rule-out of AMI.
Although high-sensitivity troponin is the biomarker of choice, it has limitations. Slight elevations have a moderate positive predictive value for AMI and may be due to other causes. Moreover, although the rising and falling pattern in biomarker levels (delta) could allow differentiation between acute and chronic injury, the guidelines do not specify the significant delta values. These values differ widely from one study to another and may vary according to the reagents used,3 although the guidelines mention that the higher these values, the greater the probability of AMI.
The 0 h/3 h algorithm has been retained (2 high-sensitivity troponin assays separated by a 3-hour interval) and the ultrarapid 0 h/1 h algorithm has been introduced (2 assays separated by 1 hour) to rule-in or rule out AMI. These algorithms have an excellent negative predictive value (around 98%) and a lower positive predictive value (75%-80%).2 Some studies report that the limit of the 99th percentile is too high to rule out AMI and recommend troponin levels as low as the limit of detection for this purpose. The cut-off points should be optimized according to each reagent and according to the methodology of each hospital. The 0 h/1 h algorithm is unreliable in patients presenting very early (< 1 hour from chest pain onset) and there is a need for more information on the prognostic value of both algorithms. That is to say, irrespective of the diagnostic label, it is crucial to know whether direct hospital discharge is safe. As mentioned in the guidelines, the algorithms should only be used in combination with the available clinical information, including an analysis of the pain characteristics, risk factors and the electrocardiogram (ECG) results.
Figure 2 of the guidelines indicates the possibility of direct discharge for certain patients. However, the text mentions that those without signs of ischemia on ECG and with normal troponin levels, who have been asymptomatic for several hours after the index pain, are candidates for a noninvasive test for ischemia or noninvasive coronary angiography by multidetector computed tomography (MDCT). Multidetector computed tomography has a high negative predictive value, but the clinical context should be considered in its interpretation, because it may lead to an overuse of invasive coronary angiography and revascularization.4 It is not clear when a stress technique or MDCT is preferable, a decision that will probably depend on the availability at each center. The systematic performance of echocardiography continues to be recommended.
PROGNOSTIC ASSESSMENTRisk assessment using standardized scoring systems also continues to be recommended, and GRACE—now presented in its 2.0 version—is still considered to be the best risk score. The discussion of the prognostic implications of the clinical and ECG presentation, stress tests for inducible ischemia, ST monitoring, and biomarkers has been shortened. This simplifies the guidelines, although skimming over the clinical and ECG features associated with high risk may not be helpful to less experienced clinicians. Standardized scores predict the overall patient risk, but they are supplementary to clinical judgement. Decision-making can be aided by some of the clinical and ECG features associated with the severity of coronary artery disease and the probability of ischemia recurrence 5 that are not included in the scoring systems.
A section is devoted to the risk of ventricular arrhythmias and a table indicating the recommended site of care (regular ward or intermediate care, coronary care or intensive care unit) to which the patient should be admitted. Continuous rhythm monitoring is recommended until the diagnosis of non-ST elevation acute myocardial infarction (NSTEMI) is established or ruled out and the patients with NSTEMI are admitted to a monitored unit. Monitoring should be maintained for 24hours or until percutaneous coronary intervention (PCI) in those patients at low risk for arrhythmias, or longer in those with intermediate or high risk, and in certain cases of unstable angina. These recommendations may have an impact on hospital organization, increasing the demand for beds in intermediate care, although the level of the available evidence is low and the indications are based on consensus.
To assess bleeding risk, the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) score is preferred. However, its modest discriminatory power in patients managed conservatively or receiving oral anticoagulation therapy should be stressed. For these reasons, and despite its acceptable predictive value in patients undergoing invasive management, the recommendation for its use it has decreased from I-B to IIb-B.
TREATMENTPharmacological Treatment of IschemiaThe guidelines recommend that oxygen therapy be reserved for patients with saturation < 90% or respiratory distress, and opiates should be restricted to the greatest possible extent, as they slow the absorption of antiplatelet agents. Nitrates are recommended to relieve angina or to treat hypertension or heart failure, but their continuous systematic use is advised against, and they are contraindicated after recent intake of phosphodiesterase-5 inhibitors.
On the basis of a recent meta-analysis, the guidelines recommend beta-blocker administration, in the absence of contraindications, to all the patients with symptoms of ischemia. The factors that predispose to shock following early administration of beta-blockers are specified. Calcium channel blockers are indicated in vasospastic angina. Aside from this, calcium channel blockers and ranolazine are only mentioned in the Appendix for selected patients and the reference to ivabradine in the acute phase has disappeared.
Platelet InhibitionThe use of aspirin continues to be a universal recommendation. The guidelines stress the variability in the response to clopidogrel, which has been associated with an increased risk of ischemic events. Reference is made to a subanalysis of TRITON (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel) in patients with NSTEACS who had undergone PCI, which reproduced the results of the main study. The subanalysis revealed a reduction of the primary endpoint with prasugrel, due mainly to a significant decrease in reinfarction with respect to clopidogrel, and an increase in bleeding events. The guidelines also mention a subanalysis of the PLATO (PLATelet inhibition and patient Outcomes) trial, carried out in patients with NSTEACS treated with invasive and noninvasive strategies, in which the primary endpoint and cardiovascular and all-cause mortality were significantly reduced with ticagrelor compared with clopidogrel, with an increase in spontaneous bleeding.
With respect to the timing of the introduction of P2Y12 inhibitors, the recommendation to administer these drugs as early as possible has disappeared. Presugrel initiation is recommended once the coronary anatomy is known and prior to PCI, which agrees with the results of the ACCOAST (Comparison of Prasugrel at the Time of Percutaneous Coronary Intervention or as Pretreatment at the Time of Diagnosis in Patients with Non-ST Elevation Myocardial Infarction) trial. In that study, pretreatment with prasugrel offered no advantages over its initiation after determination of the coronary anatomy, and the risk of bleeding was increased. The guidelines do not mention the optimal timing of ticagrelor or clopidogrel initiation because of a lack of trials comparing early initiation with later treatment.
The guidelines no longer discuss personalized treatment based on the platelet reactivity test or on carrying out genetic testing to detect polymorphisms related to the risk of ischemic events in patients treated with clopidogrel. The results of the ANTARCTIC (Tailored Antiplatelet Therapy Versus Recommended Dose of Prasugrel) trial are still pending. This ongoing study involves elderly patients treated with several doses of prasugrel depending on the results of a platelet reactivity test. Notably, the Appendix still indicates that these tests should be considered for patients treated with clopidogrel in certain situations.
With respect to the early discontinuation of dual antiplatelet therapy because of surgery or a bleeding complication, interruption is considered acceptable after completion of at least 1 month in patients revascularized with bare-metal stents and after 3 months of treatment in those with new-generation drug-eluting stents. This problem occurs frequently and is clinically relevant, and perhaps the reasons for this recommendation should have been better explained. The idea is to perform the intervention in these patients in hospitals with continuous availability of a catheterization laboratory, as well as to prolong the interruption of the P2Y12 inhibitors prior to interventions in which the risk of bleeding is very high. Bridging therapy with glycoprotein (GP) IIb/IIIa inhibitors (tirofiban or eptifibatide) is skimmed over, without specifying in which patients it can be recommended and how it is provided. Finally, the guidelines stress the importance of educating patients, relatives, and physicians about maintaining adherence to the dual antiplatelet regimen, even in the case of surgical interventions without a high risk of bleeding.
The guidelines summarize studies comparing different durations of dual antiplatelet therapy and include a discussion on a recent meta-analysis showing that, in comparison with a 12-month duration after the implantation of drug-eluting stents, a shorter duration was accompanied by less bleeding, with no significant differences in ischemic events, whereas, a longer duration was accompanied by fewer events, but with a higher risk of bleeding, and even a higher mortality rate. The final recommendations maintain 12 months of dual antiplatelet therapy, in the absence of contraindications, which could be shortened or extended, depending on the individual ischemic risk and bleeding profiles. Importantly, the recommendation to extend the dual antiplatelet therapy was based on 2 trials (DAPT and PEGASUS-TIMI 54) that did not focus on patients with NSTEACS, and the latter is a study on secondary prevention.
Glycoprotein IIb/IIIa inhibitors are confined to the catheterization laboratory for use in bailout situations or thrombotic complications during PCI, and their administration prior to coronary anatomy identification is contraindicated. The guidelines stress the lack of data on the role of GPIIb/IIIa inhibitors in patients treated with prasugrel or ticagrelor. In the wake of the negative results of the TRACER (Thrombin Receptor Antagonist for Clinical Event Reduction in Acute Coronary Syndrome) trial, vorapaxar is not recommended for the management of NSTEACS, although it is authorized in secondary prevention. Indications are provided for the use of proton pump inhibitors in combination with dual antiplatelet therapy, although no one inhibitor has priority over the others.
For the first time, the guidelines admit the possibility (IIb-A) of using cangrelor, a reversible P2Y12 receptor inhibitor with a short half-life. It is administered intravenously to patients undergoing PCI who have not received other P2Y12 inhibitors. In a meta-analysis of 3 clinical trials, cangrelor was superior to clopidogrel in a variable combination of events, with an increase in bleeding. The interpretation of those studies is complicated by the heterogeneity of the population included and by the fact that clopidogrel is administered during PCI, or even afterwards. The possible indication of cangrelor as a bridging therapy to surgery is mentioned.
AnticoagulationThere are slight changes with regard to anticoagulation, but a section is included in the Appendix with practical recommendations for the management of bleeding in general and bleeding associated with distinct anticoagulants in the diverse revascularization scenarios. The doses of parenteral anticoagulants are listed for patients with normal renal function and for those with renal failure.
Fondaparinux continues to be the preferred anticoagulant, although the recommendation for its use has gone from I-A to I-B, and the guidelines maintain their insistence on the need to administer boluses of unfractionated heparin to patients who undergo PCI. If fondaparinux is not available, enoxaparin is recommended, with the same class and level of evidence as unfractionated heparin (I-B). Bivalirudin is recommended during PCI as an alternative to the combination of unfractionated heparin and GPIIb/IIIa inhibitors. However, the guidelines have eliminated the recommendation of bivalirudin for patients with a high bleeding risk planned for an emergency or early invasive strategy. On the other hand, the guidelines now consider administrating low-dose rivaroxaban, together with aspirin and clopidogrel, to patients with high ischemic risk, low bleeding risk, and with no prior stroke, after discontinuation of parenteral anticoagulation, if ticagrelor or prasugrel is not available (IIb-B).
The description of the possible advantages of enoxaparin over unfractionated heparin may create some confusion, as it is based on 2 meta-analyses that jointly analyze the scenarios of NSTEACS and acute coronary syndrome with ST elevation, but reach different conclusions. Among the debatable aspects, the guidelines do not establish how to control the level of anticoagulation during long PCI procedures. Based on a meta-analysis, they consider administration of additional unfractionated heparin boluses guided by the activated clotting time (IIb-B). Another aspect they do not define is the duration of parenteral anticoagulation for nonrevascularized patients. The results of the MATRIX (Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and Systemic Implementation of angioX) trial, which showed a rate of adverse events similar to those of bivalirudin and of unfractionated heparin in acute coronary syndrome patients undergoing PCI, have not been incorporated because their presentation coincided with that of the new guidelines.
Management of Antiplatelet Therapy in Patients Requiring Oral AnticoagulationFor the first time, there is a specific section on this subject. The recommendations are based on a recent consensus document.6 In all, 6% to 8% of patients with NSTEACS require oral anticoagulation for other reasons. In those patients, the dual antiplatelet therapy necessary to prevent stent thrombosis does not effectively prevent embolic risk, but triple therapy with dual antiplatelet therapy and oral anticoagulation substantially increases the risk of bleeding.
There is consensus on the benefits of anticoagulation therapy at discharge for patients, but the duration of triple therapy should be minimized. If the patient receives vitamin K antagonists, close monitoring of the international normalized ratio (INR) is recommended, keeping in mind the therapeutic range of 2.0 to 2.5 (with the exception of patients with prosthetic valves). If the patient is taking any of the new oral anticoagulants, with which there is less experience in the context of triple therapy, the prescriptions should be for the lowest tested doses. The use of ticagrelor or prasugrel is advised against in these patients.
Antithrombotic therapy should be based on the clinical situation, the revascularization strategy, and risk of bleeding, estimated in this context using the HAS-BLED (score hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile international normalized ratio, elderly (> 65 years), drugs/alcohol concomitantly). Patients with low bleeding risk (HAS-BLED 0-2) who undergo PCI should receive triple therapy (anticoagulation, aspirin, and clopidogrel) for 6 months, and subsequently, continue with anticoagulation and a single antiplatelet agent until the end of month 12. For patients with high bleeding risk (HAS-BLED ≥ 3), triple therapy should be limited to 4 weeks and, again, they should continue with anticoagulation and a single antiplatelet agent until the end of month 12. Patients treated conservatively or with surgical revascularization should receive anticoagulation and a single antiplatelet agent for the first year. After that, single-drug anticoagulation is probably sufficient for all patients.
The choice of the type of stent should be individualized. As previously mentioned, third-generation drug-eluting stents could shorten the duration of dual antiplatelet therapy. This may be an attractive option for patients receiving anticoagulation therapy. Based on the results of the WOEST (What is the Optimal antiplatElet and anticoagulant therapy in patients with OAC and coronary StenTing) trial, one option being considered is to prescribe treatment with oral vitamin K antagonist anticoagulants and clopidogrel to patients with high bleeding risk and low risk of thrombosis of the chosen stent. For patients with atrial fibrillation who are not at high risk for thromboembolism (CHA2DS2-VASc 1 [men] or 2 [women]), dual antiplatelet therapy is recommended as an alternative to triple therapy.
With respect to coronary artery surgery in anticoagulated patients, if the intervention is urgent, prothrombin complex concentrate should be administered, as well as vitamin K for those being anticoagulated with vitamin K antagonists. In the case of elective surgery, the usual recommendation is to interrupt the anticoagulant therapy 48hours before and reinitiate it as soon as possible after the intervention.
Management of Acute Bleeding ComplicationsAnother new feature is a table outlining proposed strategies to reduce the bleeding risk in patients who undergo PCI, such as adjusting anticoagulant doses to body weight and renal function, or performing PCI without interrupting oral anticoagulation, and avoiding dual anticoagulation prior to coronary angiography in chronically anticoagulated patients. The guidelines also include an excellent online Appendix with practical recommendations for treating bleeding associated with antiplatelet agents, vitamin K antagonists or the new oral anticoagulants, although many of them are not based on controlled trials.
For bleeding in patients treated with vitamin K antagonists, the administration of vitamin K reverses the effect, but it takes several hours and has not been shown to offer any benefit in emergency situations. Prothrombin complex concentrate is recommended, as it is more efficient than fresh frozen plasma and recombinant activated factor VII. In bleeding associated with the new oral anticoagulants, vitamin K or fresh frozen plasma have no demonstrated effect, and for patients with hemodynamic deterioration or life-threatening bleeding, prothrombin complex concentrate is the best option.
The characteristics, predictors, and treatment of bleeding not related to the access site, and of that related to PCI or coronary revascularization, are described. There is a section on transfusion, which mentions the higher mortality rate among transfused acute coronary syndrome patients. Despite the conflicting results of some studies, the guidelines recommend a policy of restrictive transfusion (hematocrit < 25% or hemoglobin < 7 g/dL) for anemic patients.
INVASIVE CORONARY ANGIOGRAPHY AND REVASCULARIZATIONMajor New FeaturesThe guidelines emphasize the superiority of the invasive approach in the management of NSTEACS and point out that the benefit of this strategy, shown in trials carried out in the past, is being underestimated, since the generalized use of radial access and the new-generation drug-eluting stents and antiplatelet agents enable even better outcomes. The accepted criteria for very high, high, intermediate, and low risk are clearly specified in a Table. In contrast to the latest European guidelines for myocardial revascularization,7 diabetes mellitus, renal failure, postinfarction angina, and previous revascularization are considered criteria for intermediate risk, rather than secondary criteria for high risk. Coinciding with the previous guidelines, there are detailed recommendations for the invasive approach in NSTEACS, with 4 possible alternatives, depending on the patient's risk factors: immediate < 2 hours), early (< 24 hours), delayed (< 72 hours), and elective (according to the results of noninvasive tests).
In accordance with existing studies, the guidelines recommend radial access, depending on the operator's experience, although they indicate that proficiency in femoral access should be maintained. A section is devoted to the identification of the culprit lesion on the basis of 4 angiographic criteria (thrombus, plaque ulceration, plaque irregularity, and dissection), at least 2 of which should be present. This definition might be useful, but has not been validated, and it may be too restricted.
The new-generation drug-eluting stents can be considered an alternative to bare-metal stents in those patients with high bleeding risk scheduled to receive dual antiplatelet therapy for no longer than 1 month.
There are detailed indications for antiplatelet therapy before and after coronary artery surgery, and the guidelines state that the recommendation of dual antiplatelet therapy for 12 months in the absence of contraindications depends on the revascularization strategy. The level of priority and technical aspects of surgical revascularization are presented as online supplementary material.
Controversial AspectsWhen the criteria for very high risk are met, angiography should probably be immediate. However, the established 24-hour limit for patients considered high-risk should be a subject of debate, as the studies cited in support of this recommendation found no clear benefit from a generalized early strategy. Moreover, any elevation in the troponin level is indicative of high risk, but minimum increases do not have the same prognostic implications as greater increases, and may not even be due to acute coronary syndrome. Changes in T waves, also considered to indicate high risk, do not have the same value as changes in the ST segment for the prediction of the existence of serious coronary lesions or the incidence of complications.5 On the other hand, for a large proportion of patients with NSTEACS, scheduling of coronary angiography within less than 24hours can create considerable logistical problems, such as the need for urgent interhospital transfers, and can interfere with other more serious cases and favor the referral of patients without adequate assessment.
Little is said about the utility of intracoronary imaging studies in the detection of the mechanisms leading to plaque instability and the prognostic implications.8 The limited reliability of the pressure wire in the assessment of culprit lesions is stressed, but mention should be made of its potential utility for assessing nonculprit lesions of uncertain significance or even potential culprit lesions of uncomplicated morphology and uncertain significance.9,10
In multivessel disease, the decision on the revascularization mode should be individualized and reached by consensus among the heart team, taking into account patient preferences. Another responsibility of the heart team is to estimate the risk of bleeding and ischemia and guide the assigning of priority to revascularization surgery, while managing antiplatelet therapy. The lack of a definition of the concept of heart team and its composition in the guidelines is quite noticeable.
It is established (class I-B recommendation) that CABG be performed without delay in patients with hemodynamic instability, ongoing myocardial ischemia, or very high-risk coronary anatomy, regardless of the antiplatelet therapy received. However, the extension of this emergent recommendation to patients with a very high-risk anatomy even if they are stable, and regardless of the antiplatelet therapy received, is debatable. Very high-risk coronary anatomy is not defined. The supplementary material mentions the concept of critical anatomy, which is not defined either. The recommended surgery in patients with critical anatomy is urgent (during the hospital stay) but not emergency surgery, all of which creates confusion. In our patient population, up to 50% of the surgical myocardial revascularization procedures are performed (during the hospital stay) as urgent interventions. The lack of randomized studies to define the optimal priority criteria for surgery in patients who have been stabilized after NSTEACS renders it impossible to make evidence-based recommendations. The usual approach is to delay surgery for a few days, even if the patient has left main coronary artery disease; in fact, that is what is indicated in the supplementary material of these guidelines. There is a need for uniform definitions of the terms immediate, emergent, and urgent relative to the planning of surgery, to be used consistently in documents issued by the scientific societies.
DIFFERENCES RELATED TO SEX AND TO SPECIAL POPULATIONSThe new guidelines have eliminated specific recommendations for management according to sex and acknowledge that there is no scientific evidence to justify different strategies for the treatment of men and woman. This is one of the major changes and most positive outcomes of these guidelines. The risk of in-hospital death in women is twice that of men, which has been attributed to the underuse of evidence-based treatments in women. It will be essential to implement strategies aimed at promoting the application of the guidelines and increasing the awareness of gender equality in terms of cardiovascular risk.
Among patients with NSTEACS, those of advanced age (≥ 75 years) represent a growing segment but have a lower probability than younger patients of being treated in accordance with guideline recommendations, which may, in part, explain their poorer prognosis. There is a section devoted to elderly and frail patients, although the approach to the particular features of this subgroup focuses almost exclusively on the chronological point of view. The only issue addressed is the need to consider cognitive or functional impairment, dependence on others and frailty, which is recognized as a powerful independent predictor of mortality. However, there is a need to adopt an approach to the systematic evaluation of frailty, the tools that should be used, and how to incorporate them into the decision-making process. Thus, this should be an area of research in this field.13,14
With respect to patients with diabetes mellitus, the threshold for initiating glucose-lowering therapy is more precisely defined, although specific treatment regimens are not described in detail. Less strict glycemic control is recommended for patients of advanced age, and the recommendation concerning the control of renal function in diabetic patients following coronary angiography has been modified.
Patients with chronic kidney disease constitute another group at higher risk for complications. There are no changes in the recommendations regarding antiplatelet therapy, which should be the same as for patients without renal failure, although with dose adjustment when necessary, or with respect to anticoagulant therapy, in which it will be necessary to indicate unfractionated heparin or adjust the doses of other anticoagulants. The fear of renal function deterioration secondary to coronary angiography is one of the reasons why the percentage of patients who undergo this invasive strategy is inversely proportional to the severity of the renal failure. The SWEDEHEART registry provided a very precise analysis of the relationship between early revascularization and 1-year mortality in the different stages of renal dysfunction, and a reduction in the mortality rate of 36% was observed, although the significance of this benefit disappeared in the more advanced stages. These data indicate that the treatment strategy for these patients should be individualized, as recommended by the guidelines.
The new guidelines have included a section on the treatment of acute heart failure. With respect to ventricular assist devices, the guidelines maintain the option of using intra-aortic balloon counterpulsation in selected patients, as well as other short-term devices, and advise against the systematic use of counterpulsation in cardiogenic shock. Importantly, there is a change in the recommendation for implantable cardioverter defibrillators and cardiac resynchronization therapy, as the document stresses the importance of waiting at least 40 days before implantation in patients who are symptomatic despite optimal therapy and have no additional options for revascularization. This recommendation is based on the available evidence, although the ESC guidelines for the prevention of sudden death allow earlier implantation under certain circumstances. In patients with residual ischemia, revascularization should be performed first, followed by a wait of up to 6 months before assessment of the indication for device implantation. Atrial fibrillation during hospital stay is associated with a higher risk of recurrent ischemia, heart failure, and thromboembolic complications, as well as a longer hospital stay and a higher rate of long-term mortality. The guidelines stress the difficulty of establishing a differential diagnosis between atrial fibrillation with elevated troponin and type 1 AMI. Thus, if there is significant troponin elevation, the performance of tests for ischemia may be justified. The recommendations are based on the latest guidelines for atrial fibrillation and heart failure.
Anemia is common in patients with NSTEACS and is associated with an increase in the risk of death, AMI, and major bleeding. It is uncertain whether anemia is a marker associated with an elevated comorbidity burden or is an independent determinant of prognosis. Given that the optimal threshold for the justification of packed red blood cell transfusion is unknown, the recommendation in this respect has gone from I-B to IIb-C. There is a section on the management of thrombocytopenia with no significant changes.
LONG-TERM MANAGEMENTAntithrombotic therapy has been mentioned above. With respect to lipid-lowering therapy, the guidelines maintain the recommendation to initiate high-intensity statin therapy as early as possible or to increase the intensity of statin therapy in those receiving low- or moderate-intensity regimens. Although there are no explicit recommendations on specific therapeutic goals, a new aspect is that the addition of a second lipid-lowering agent can be considered in patients with low-density lipoprotein cholesterol (LDL-C) ≥ 70 mg/dL (≥ 1.8 mmol/L), despite receiving the maximum tolerated dose of statins. However, for now, this recommendation applies only to ezetimibe, given that it is based on the IMPROVE-IT (IMProved Reduction of Outcomes: Vytorin Efficacy International Trial) study.
Angiotensin-converting enzyme (ACE) inhibitors are recommended for patients with left ventricular ejection fraction (LVEF) ≤ 40%, heart failure, hypertension, or diabetes mellitus, and the recommendation on renal failure has been omitted. The recommended target blood pressure is < 140/90mmHg, in accordance with the ESC guidelines for hypertension. In patients with intolerance to ACE inhibitors, angiotensin II receptor blockers are an alternative, although they are only superior to the ACE inhibitors in the presence of cough. The indication suggesting ACE inhibitors for all other patients, which in previous guidelines was a class I-B recommendation, has disappeared.
Long-term beta-blockers are indicated only for patients with LVEF ≤ 40, and the guidelines mention that their efficacy has not been evaluated recently in patients with NSTEACS without ventricular dysfunction or heart failure. Observational studies indicate that their long-term indiscriminate administration may not be useful,15 although, according to other studies, they could be beneficial after discharge, in the absence of ventricular dysfunction.16
The indication for mineralocorticoid receptor antagonists has not changed, and they are recommended for patients with LVEF ≤ 35% and heart disease or diabetes mellitus, without renal dysfunction or hyperkalemia, although, in the text, LVEF ≤ 40% is mentioned as the threshold for treatment.
The recommendation on glycemic control is generic, but clear: the older the patients, the greater their comorbidities, or the longer their history of diabetes mellitus, the less strict their glycemic control.
The recommendations on lifestyle and rehabilitation do not differ from those of earlier guidelines, although the inclusion of these patients in structured cardiac rehabilitation programs is considered a class IIa-A recommendation, without specifying the duration. The importance of the advice on aerobic exercise and smoking cessation is discussed, and diet and weight control are mentioned. However, the document misses the opportunity to indicate clearly the type of diet that is adequate, specifically, that which is rich in virgin olive oil, nuts and other dried fruits, whose effectiveness in primary cardiovascular prevention has been demonstrated.17
CONCLUSIONSThe guidelines provide an excellent review and clear recommendations on the management of patients with NSTEACS. Because NSTEACS is by far the most common presentation of acute coronary syndrome in Spain, the impact of these clinical practice guidelines in Spain is important. Notable aspects are the refinement of the diagnostic algorithms in emergency cases, the adjustment of the recommendations for antithrombotic therapies and for secondary prevention to the latest available evidence, and the firm commitment to an early invasive strategy for most patients. The effort made by the authors to provide useful recommendations on aspects not previously dealt with, such as the practical management of bleeding or the treatment of patients requiring chronic anticoagulation, is very much appreciated.
CONFLICTS OF INTERESTNone declared.
Referencias no citadasSEC Working Group for the 2015 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-segment Elevation: José A. Barrabés (coordinator*), Ángel Cequier (coordinator), Héctor Bueno, Ángel L. Fernández González, Antonio Fernández-Ortiz, Rosa M. Lidón, Francisco Marín, Juan Sanchis, Alessandro Sionis and José M. de la Torre Hernández.
Expert Reviewers for the 2015 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-segment Elevation: Jaime Aboal Viñas, Emad Abu-Assi, Albert Ariza Solé, Oscar Díaz Castro, José Luis Ferreiro Gutiérrez, Alberto García Lledó, Iván Núñez Gil, Sergio Raposeiras Roubín, José F. Rodríguez-Palomares, Ana Viana Tejedor and David Vivas Balcones.
SEC Guidelines Committee: Manuel Anguita (president), Ángel Cequier, Fernando Alfonso, Lina Badimón, José A. Barrabés, Ignacio Fernández Lozano, José Juan Gómez de Diego, Luis Rodríguez Padial, José Alberto San Román, Pedro-Luis Sánchez, Juan Sanchis and Alessandro Sionis.
SEC Working Group for the 2015 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-segment Elevation, Expert Reviewers for the 2015 ESC Guidelines for the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-segment Elevation and the SEC Guidelines Committee.