In accordance with the policy on clinical practice guidelines of the Spanish Society of Cardiology (SEC),1 this article presents the novel, pertinent, and conflicting aspects of the 2017 focused update on the use of dual antiplatelet therapy (DAPT) in coronary artery disease of the European Society of Cardiology (ESC) together with the European Association for Cardio-Thoracic Surgery.2
The preamble once again emphasizes that, although these recommendations are designed to support health care professionals in decision-making, the ultimate responsibility in each case lies with the professional and the patient. The authors use the opportunity to insist on the need for registries that verify the clinical reality to address these recommendations and to analyze the differences between them and the standard clinical practice.
This year marked the 21st anniversary of the publication of the first clinical trial that established the superiority of DAPT over anticoagulation after percutaneous coronary intervention (PCI); the number of patients treated with DAPT is high and ever growing. The challenges facing DAPT have included the shift from a local target vessel strategy to a comprehensive protection strategy (fewer ischemic coronary artery complications and those of other territories), doubts about the optimal duration of treatment in different settings (whether the procedure was invasive or not and according to revascularization type), bleeding complications, influence of clinical variables, and comorbidities (eg, advanced age, diabetes mellitus, renal failure, need for anticoagulation). Because these variables mean that patients in clinical practice are often different from those selected in clinical trials, this guideline-update on the use of DAPT is both interesting and necessary.
The guidelines uses the standard levels of evidence (A, B, C) and classes of recommendation (classes I, IIa, IIb, and III) and ends with a summary of the key messages and a succinct table showing the recommendations. One notable aspect of these guidelines, in contrast to others, is the high percentage of class I and III recommendations (27 of 64, 42%). Another interesting aspect is the additional on-line material, which briefly describes 18 clinical cases that clearly and specifically illustrate the practical application of the guidelines’ recommendations.
METHODSAt the suggestion of the SEC Guidelines Committee and the coordinators assigned to these guidelines, a group of expert cardiologists was selected to review the ESC guidelines published at the end of August. The objective was to comment on the nature and timeliness of this document, analyze the methodology, and highlight the novelties and positive, questionable, or omitted aspects (Table 1). These evaluations were used to develop a joint document, which was further assessed by cardiologists appointed by the Catheterization, Ischemic Heart Disease and Acute Cardiovascular Care, and Clinical Cardiology sections of the SEC.
Comments on Important, Debatable, and Novel Aspect
| Relevant/novel Aspect | Comment |
|---|---|
| Strategies and tools | |
| Incorporation of the risk scores (DAPT and PRECISE-DAPT) to guide DAPT duration | Lack of prospective validation of their usefulness in clinical trials |
| Early administration of ticagrelor or clopidogrel in NSTEACS | More proactive guidelines regarding pretreatment with P2Y12 inhibitors, although there have been no relevant changes in the pertinent evidence |
| Ticagrelor or prasugrel instead of clopidogrel for patients with stable ischemic heart disease undergoing complex PCI | Prasugrel or ticagrelor can again be used in this scenario according to ischemic risk (high SYNTAX, previous stent thrombosis, location and number of stents) and bleeding risk |
| Use of PPI in combination with DAPT to reduce the risk of gastrointestinal bleeding | This recommendation is generalized to all patients |
| Switching of oral P2Y12 inhibitors | Algorithms based on pharmacodynamic studies are incorporated, one for the acute phase and another for the chronic phase. There is little relevant clinical evidence |
| The metallic stent is the device of choice, regardless of the planned DAPT period | The planned DAPT period should not affect the choice of the metallic stent used in percutaneous revascularization, but the reason why is not stated in the text |
| Duration | |
| The decision on the duration of DAPT must be dynamic and must be re-evaluated during the course of the recommended regimen by assessing risks/benefits at all times | New recommendation |
| DAPT duration based on the underlying clinical profile rather than the type of stent | Different approaches of longer or shorter DAPT duration |
| For patients with stable disease after PCI, 6 mo of DAPT are recommended regardless of the type of metallic stent implanted | Omitted for the first time are specific recommendations for the dual antiplatelet period after metallic stent implantation in patients with stable disease |
| If a bioabsorbable drug-eluting stent has been implanted, prolonged (at least 12 m) and potent DAPT is recommended, whenever possible | This recommendation implicitly recognizes an excessive ischemic/thrombotic risk associated with these devices |
| Duration of DAPT in patients with ACS and cardiac surgery | • 6 mo for patients with high risk of bleeding and receiving an aspirin plus clopidogrel or aspirin plus ticagrelor (IIa C) regimen• Prolong DAPT beyond 12 mo (up to 36) in patients without high risk of bleeding and with previous infarction (IIb B) |
| DAPT duration in patients with ACS and conservative treatment | Prolong DAPT for up to 36 months in patients with previous infarction, high ischemic risk, and good tolerance to antiplatelet therapy (ticagrelor 60 mg/12 h plus aspirin or clopidogrel plus aspirin) (IIb C) |
| Special groups | |
| Interruption of DAPT before surgery in patients with ACS | 3 d for ticagrelor5 d for clopidogrel7 d for prasugrel |
| Anticoagulated patients with hemorrhagic risk higher than ischemic risk | Chronic oral anticoagulation with clopidogrel may be considered for 12 months (IIa A) |
| Chronic treatment (> 12 mo) for anticoagulated patients undergoing angioplasty | Chronic oral anticoagulation is exclusively recommended (without added antiplatelet) (IIa B) |
| DAPT duration should be similar regardless of sex or the presence of diabetes mellitus | Waiting for new evidence on diabetes |
| DAPT if history of thrombosis (of the stent), peripheral vascular disease, and complex PCI | There are favorable scenarios for the use of prolonged DAPT |
| Need for ad hoc-designed tests that establish the minimum duration of DAPT necessary after implantation of latest-generation drug-eluting stents and bioresorbable drug-eluting stents and after angioplasty with drug-coated balloons | Moving toward an approach that is more centered around the type of stent |
| Prospective validation is recommended in contemporary cohorts of tools that allow the precise identification of patients who could benefit more from prolonged DAPT, beyond the first year and before 30 mo | Nonetheless, the guidelines are oriented toward prolonging the DAPT |
ACS, acute coronary syndrome; DAPT, dual antiplatelet therapy; PCI, percutaneous coronary intervention; PPI, proton pump inhibitor.
This section begins by recalling the effectiveness of DAPT in terms of the continuous prevention of stent thrombosis (from the acute to the very late phases) and reiterates that its main benefit, when it lasts longer than 1 year, is the reduced incidence of spontaneous myocardial infarction. The possible benefit on mortality is highly dependent on the patients’ cardiovascular history (thus, patients with a history of acute coronary syndrome [ACS] may benefit more than those with stable coronary artery disease). In addition, it is restated that continuous DAPT increases the bleeding risk proportionally to its duration. Thus, when the duration of DAPT is being decided, the guidelines insists on an individualized approach that is based on the balance between ischemic and bleeding risks. Importantly, the decision on the duration of DAPT should be dynamic and should be re-evaluated during the course of the initially recommended regimen.
One of the main novelties of these guidelines is the recommendation to use risk scales to guide DAPT duration (IIb A). It is clearly specified that the scales that must be used (in preference to others designed and evaluated for the prediction of hospital events or in a short follow-up) are those specifically designed to guide and aid decision-making on the duration of DAPT. Only 2 meet these characteristics: DAPT score (a value ≥ 2 indicates the benefit of prolonged DAPT) and PRECISE-DAPT (a value ≥ 25 indicates the benefit of shortened DAPT). It should be remembered that the DAPT score should be used after 12 event-free months of DAPT and that the PRECISE-DAPT should be used at the time of stent implantation, as noted in Table 3 of the document. Despite the possible usefulness of these models, although they indicate that a more stringent validation is needed, it could be the case that, in a given patient, the values obtained in one score recommend shortening DAPT and those of the other, prolonging it. Thus, it is important to remember that their function is to aid decision-making and never to replace clinical judgment. Regardless, the general class IIb recommendation for the use of these scales is probably reasonable because, as recognized in the guidelines, there is a lack of prospective validation with randomized studies demonstrating the possible clinical benefit of these scores.
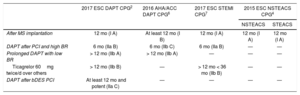
Recommendations on DAPT Duration in Patients With Acute Coronary Syndrome Treated With PCI
| 2017 ESC DAPT CPG2 | 2016 AHA/ACC DAPT CPG6 | 2017 ESC STEMI CPG7 | 2015 ESC NSTEACS CPG4 | ||
|---|---|---|---|---|---|
| NSTEACS | STEACS | ||||
| After MS implantation | 12 mo (I A) | At least 12 mo (I B) | 12 mo (I A) | 12 mo (I A) | 12 mo (I A) |
| DAPT after PCI and high BR | 6 mo (IIa B) | 6 mo (IIb C) | 6 mo (IIa B) | — | — |
| Prolonged DAPT with low BR | > 12 mo (IIb A) | > 12 mo (IIb A) | — | — | — |
| Ticagrelor 60mg twice/d over others | > 12 mo (IIb B) | — | > 12 mo < 36 mo (IIb B) | — | — |
| DAPT after bDES PCI | At least 12 mo and potent (IIa C) | — | — | — | — |
bDES, bioresorbable drug-eluting stent; BR, bleeding risk; CPG: clinical practice guidelines; DAPT, dual antiplatelet therapy; MS, metallic stent; NSTEACS, non—ST-segment elevation acute coronary syndrome; PCI, percutaneous coronary intervention; STEACS, ST-segment elevation acute coronary syndrome; STEMI, ST-segment elevation myocardial infarction.
Regarding the choice of P2Y12 inhibitor, the guidelines stress the possibility of using ticagrelor or prasugrel (IIb C recommendation) for patients with stable ischemic heart disease who undergo PCI, taking into account the patients’ ischemic risks (high SYNTAX score, previous stent thrombosis, and stent location and number) and bleeding risks.
As regards the always complicated and controversial issue of pretreatment with P2Y12 inhibitors, these guidelines are more proactive than the previous ones. The guideline recommends (I A recommendation) the general pretreatment of patients with known coronary anatomy who have decided to undergo PCI, as well as those with ST-segment elevation ACS or ST-segment elevation myocardial infarction. The authors also recommend that ticagrelor administration be considered, or clopidogrel if ticagrelor is not an option, as soon as the diagnosis is made (IIa C recommendation). This represents a change from the previous guidelines for non—ST-segment elevation ACS (NSTEACS),3 which specified that no recommendation could be made for pretreatment with these drugs because they had not been studied properly.
These guidelines also incorporate recommendations to implement measures reducing the bleeding risk associated with DAPT. In addition to the usual methods, namely, radial access in preference to femoral and an aspirin dose not exceeding 75 to 100mg, the general recommendation is to use a proton pump inhibitor in all patients receiving DAPT to minimize the risk of gastrointestinal bleeding. This represents another change from the previous guidelines,4 which restricted this drug to patients with an increased risk of gastrointestinal bleeding.
There are no changes regarding the recommendation to not systematically perform platelet function tests to guide DAPT, although they can be considered for certain patients.
Another novelty of the document is the appearance of a section dedicated exclusively to “switching” between P2Y12 inhibitors, because the guidelines admit that it may be necessary for clinical reasons and that clinical registries have shown that these changes are not uncommon in clinical practice. Indeed, patients with ACS who have received clopidogrel are specifically recommended to switch to ticagrelor (unless there are contraindications to its use) during their hospital admission, independently of the dose and time of administration (I B). The applicability of this recommendation to all patients might be debatable because, as the document notes, although this change was permitted in the pivotal trial of ticagrelor, it was not allowed in that of prasugrel. The latter study was not designed to evaluate the efficacy and safety of this change and, in addition, the patients with NSTEACS included had to have moderate or high risk. The second recommendation that has been introduced in this regard is to make changes when necessary for a clinical reason (side effects or drug intolerance) in accordance with 2 algorithms based mostly on pharmacodynamic studies, one for the acute phase (during hospitalization) and the other for the chronic phase (Figure 2 of the guidelines).
The document advises against a change in treatment in the chronic phase, given the absence of randomized studies evaluating long-term efficacy or safety. However, in the immediate future, doubts may arise about this concept with further research in the field. Indeed, in the recently published clinical trial TOPIC,5 a strategy of switching to clopidogrel after 1 month of treatment with prasugrel or ticagrelor showed safety benefits by reducing bleeding, without diminishing efficacy, vs no changes in DAPT with prasugrel or ticagrelor in patients with ACS who underwent PCI.
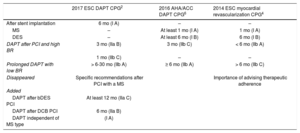
DAPT After Percutaneous Coronary InterventionThe 2 main aspects to consider when the DAPT period after PCI is being determined must be the clinical context in which it occurs–stable or unstable–and the patient's bleeding risk, except for patients who have received a bioabsorbable drug-eluting stent (DES). For these patients, prolonged (at least 12 months) and potent DAPT is recommended whenever possible. This approach assumes that the thrombotic risk associated with these devices exceeds other considerations, despite the absence of ad hoc evidence to support this strategy (IIa C). The main changes from previous recommendations and those of other scientific societies are collected in Table 22,4,6 and Table 3.2,4,6,7
Recommendations on DAPT Duration and Aspects Related to the Choice of Stent for Patients With Stable Coronary Disease Undergoing PCI
| 2017 ESC DAPT CPG2 | 2016 AHA/ACC DAPT CPG6 | 2014 ESC myocardial revascularization CPG4 | |
|---|---|---|---|
| After stent implantation | 6 mo (I A) | – | – |
| MS | – | At least 1 mo (I A) | 1 mo (I A) |
| DES | – | At least 6 mo (I B) | 6 mo (I B) |
| DAPT after PCI and high BR | 3 mo (IIa B) | 3 mo (IIb C) | < 6 mo (IIb A) |
| 1 mo (IIb C) | – | – | |
| Prolonged DAPT with low BR | > 6-30 mo (IIb A) | ≥ 6 mo (IIb A) | > 6 mo (IIb C) |
| Disappeared | Specific recommendations after PCI with a MS | Importance of advising therapeutic adherence | |
| Added | |||
| DAPT after bDES PCI | At least 12 mo (IIa C) | ||
| DAPT after DCB PCI | 6 mo (IIa B) | ||
| DAPT independent of MS type | (I A) | ||
bDES, bioresorbable drug-eluting stent; BR, bleeding risk; CPG: clinical practice guidelines; DAPT, dual antiplatelet therapy; DCBs, drug-coated balloons; DES, drug-eluting stent; MS, metallic stent; PCI, percutaneous coronary intervention.
For patients with stable disease after PCI, a DAPT period of 6 months is recommended, which can be shortened depending on the patient's bleeding risk or for safety reasons. The duration of this period should not be determined by the type of metallic stent implanted. The guidelines go beyond specific scope and favors the use of metallic stents as a default treatment option, even in patients who are recommended to have an antiplatelet period of only 1 month for safety reasons.8,9 In addition, it should be specified that the only DES shown to be safe after DAPT suspension at 1 month is the biolimus-coated stent. For patients treated with angioplasty with a drug-coated balloon, DAPT should also be maintained for 6 months. This recommendation reflects the empirical antiplatelet strategies used in different clinical trials. However, in our opinion, it could be questioned, because many studies with drug-coated balloons recommend a shorter duration.
Patients with Acute Coronary SyndromeFor patients with ACS treated with coronary stenting, the default DAPT duration should be 12 months, although it may be reasonable to shorten the period to 6 months in patients with high bleeding risk or prolong it to more than 12 months in selected patients. These decisions should be based on an evaluation of patients’ bleeding and ischemic risks. Although some characteristics can help to select the patients who would benefit most, the need to validate operative tools in clinical practice is recognized. This is especially important in the case of DAPT prolongation beyond 1 year. For patients with this indication who have tolerated this period of DAPT without bleeding complications, a longer dual antiplatelet period may be considered. In this regard, ticagrelor 60mg twice daily is specifically indicated for patients with infarction history and high ischemic risk.
Finally, although some reviews published around the same time as these guidelines have considered the potential impact of strategies that reduce the antithrombotic potency of DAPT beyond the first month after an ACS, this evidence has not been incorporated into the guidelines’ recommendations.10
DAPT and Coronary SurgeryIn this interesting section, which involves the interaction between cardiologists and cardiac surgeons, the document is very clear, particularly in the case of patients with stable coronary artery disease. In these patients, DAPT has not shown benefits on survival or reduction of thrombotic complications. There is little evidence of a potential benefit of dual therapy with clopidogrel on the permeability of venous (nonarterial) grafts and in patients who underwent surgery without extracorporeal circulation. In contrast, in patients with ACS, DAPT has been proven to effectively reduce ischemic risk irrespective of the revascularization strategy.
Preoperative DAPTGiven that continuation of DAPT until surgery increases the risk of perioperative bleeding, treatment with P2Y12 inhibitors should be interrupted whenever possible before elective surgery or the surgery should be postponed until the DAPT period is completed. When the therapy is interrupted, the guidelines provide a novel aspect based on recent studies by indicating different safety periods for the different drugs: 3 days for ticagrelor, 5 days for clopidogrel, and 7 days for prasugrel (IIa B). In urgent cases, the risk of thrombotic event recurrence and the risk of perioperative bleeding must be weighed and bridge therapy with cangrelor or a glycoprotein IIb/IIIa inhibitor should be considered in patients with very high thrombotic risk. It must be recognized that, although it appears to be one of the future indications of cangrelor, this recommendation is based on a phase II pharmacodynamic clinical trial and this indication is also not included in the technical data sheet.
In addition, the document indicates the importance of maintaining the continuity of aspirin therapy in patients with ACS and surgical revascularization, both preoperatively and postoperatively, given the risk of thrombotic complications and perioperative infarction (I C), and notes that, in the case of bleeding, the effects could be counteracted by platelet transfusion.
Postoperative DAPTAlthough DAPT reintroduction after surgery can increase the risk of bleeding complications, it should be restarted as soon as it is considered safe, except for anticoagulated patients, because there is no scientific evidence for triple therapy in this setting. The optimal restart time is not clear, but between 24 and 96hours seems reasonable for patients without recent stent implantation. The risk of atrial fibrillation (AF) in the first days of the postoperative period (30%) should be taken into account and anticoagulation may be required.
When addressing the duration of DAPT, the guidelines make distinctions according to the risk of bleeding:
- A.
Patients with a high risk of bleeding: 6 months with ticagrelor or clopidogrel plus aspirin (IIa C). This recommendation could be criticized because, given the high risk of bleeding, it seems prudent to reduce DAPT duration, but perhaps clopidogrel should be recommended.
- B.
Patients without a high risk of bleeding: 12 months with prasugrel or ticagrelor (or clopidogrel if the patient is not a candidate for the previous ones) plus aspirin (I C), with the possibility of prolonged therapy of up to 36 months in patients with previous infarction (IIb B). The document does not mention in this section the doses used for prolonged dual therapy, but it does in the group of patients undergoing conservative treatment.
The authors mention the possible usefulness of platelet function tests if the time from the treatment interruption is unconfirmed (eg, in unconscious or nonadherent patients) and to help in choosing the optimal time of suspension prior to surgery instead of an arbitrary time interval (IIb B). In addition, we are reminded that the different tests and their values are not interchangeable.
DAPT in Patients with ACS and Conservative TreatmentThe guidelines assign a class I A indication for a DAPT period of 12 months and a class IIa C indication for DAPT of at least 1 month for those with high bleeding risk (PRECISE-DAPT score ≥ 25). For patients with high ischemic risk and previous infarction who they have not experienced bleeding, the therapy can be prolonged up to 36 months using ticagrelor 60mg/12h plus aspirin (IIb B). Another option for patients with previous infarction not treated with a stent who are not candidates for ticagrelor would be aspirin plus clopidogrel (IIb C). Ticagrelor is recommended over clopidogrel if there is no bleeding risk (I B).
The guidelines highlight 2 points of interest. The first is that, in usual practice, patients with ACS and conservative treatment are less frequently treated with DAPT than those undergoing angioplasty; in this regard, the authors point out that DAPT should not be prescribed based on the revascularization or the type of stent used, but the clinical presentation. The second point refers to the treatment of patients with NSTEACS who do not have coronary lesions; there are no specific studies in this setting, although a high prevalence of plaque rupture is observed in intravascular imaging tests. In these patients, the document point out the potential usefulness of DAPT if allowed by the risk of bleeding.
In the case of patients with ST-segment elevation ACS undergoing medical treatment or with previous fibrinolysis, a DAPT duration of 1 year is recommended. However, considering that most of these patients will subsequently have invasive treatment and that DAPT has to be shown to be beneficial regardless of whether or not revascularization is performed, the therapy can be prolonged according to the risk of bleeding.
DAPT for Patients With Indication for Oral AnticoagulationThis section of the guidelines is one of the most novel, with relevant information that complements the ESC 2016 guidelines on AF,11 which provided very limited information on antithrombotic treatment in this complex group of patients. Although anticoagulated patients undergoing PCI continue to comprise just 6% to 8% of all stent-revascularized patients, it should be taken into account that the total population increases each year. Moreover, the addition of DAPT to oral anticoagulation increases bleeding complications by between 2 and 3 times.
One important aspect of the new guidelines is a series of general strategies aimed at reducing or avoiding bleeding complications.
Duration of Triple Antiplatelet TherapyThis is the aspect most discussed by the guidelines and, for the first time, the use of triple therapy (anticoagulant, aspirin, and clopidogrel) and dual therapy (anticoagulant and clopidogrel) are assigned the same level, although reserved for patients with high bleeding risk.
Ischemic and bleeding risk should determine the best antithrombotic regimen and its duration. Thus, triple therapy should be considered for up to 6 months for patients with high ischemic risk (ACS, anatomical features, or complex PCI) (IIa B recommendation). On the other hand, some patients whose bleeding risk is higher than the ischemic risk could opt for oral anticoagulation and clopidogrel (IIa A recommendation). This strategy had been assigned a class IIb C recommendation in the last AF guidelines.8 This change of indication must be prudently assessed because it is based on a single clinical trial that has some recognized selection biases (stable patients, triple therapy recommended for 12 months). In our opinion, this strategy may be an option for certain patients with very high bleeding risk but should not be generalized
Cessation of Antiplatelet AgentsThe guidelines insist on the need to discontinue aspirin or clopidogrel from 1 year in patients who have remained stable and symptom-free (IIa B recommendation). This indication is based on the evidence that in this population, oral anticoagulation plus aspirin does not increase the protective effect versus oral anticoagulation alone, but is associated with increased bleeding. This is another of the novel aspects of the document, which revises the previous indication and changes it from a IIb to IIa recommendation. However, we believe that oral anticoagulation in monotherapy might offer insufficient protection to patients who have had a coronary thrombotic event in stable anticoagulation or in patients with a high thrombotic risk. The guidelines only consider prolonging the antiplatelet therapy added to oral anticoagulation beyond 1 year for patients with very high ischemic risk or those with a mechanical prosthesis and significant atherosclerotic disease.
Anticoagulant TypeAt the time of the presentation of the guidelines, the RE-DUAL PCI study had not yet been published, although it was presented at the same Barcelona congress.12 Therefore, the document cites the PIONEER-AF-PCI13 as the only clinical trial thus far to compare vitamin K antagonists with direct oral anticoagulants (DOACs) in patients with AF subjected to PCI. The 2 anticoagulation regimens with rivaroxaban proposed in the study are criticized by the guidelines because they involve doses of rivaroxaban not approved for AF. The document proposes a IIb B indication for the use of rivaroxaban 15mg/d and clopidogrel. However, based on the fundamental studies of DOACs, the guidelines note the benefit of these agents over vitamin K antagonists in patients with AF and coronary disease and mentions the absence of evidence for the indication of one DOAC over others. Certainly, one DOAC cannot be recommended over another, although, there may be differences between them according to the results of the latest trials. The guidelines also recommend considering the lowest dosage of DOACs that has been studied for the prevention of stroke in their fundamental studies (IIa C), although these doses have been evaluated in patients with a series of specific characteristics and, for example, there is no information on the benefit of these low doses in the reduction of stroke in patients with normal renal function.
Stent TypeThe guidelines are clear in positioning the new-generation DESs as the approach of choice for patients with a high risk of bleeding, such as patients on oral anticoagulation.
Elective Noncardiac Surgery in Patients on DAPTThis section is a novelty, given that the previous recommendations did not refer to this specific problem. The guidelines address a clinical scenario of increasing importance in routine clinical practice because, as noted by the authors, an estimated 5% to 25% of patients who have undergone stent implantation will require noncardiac surgery within 5 years after the procedure. The approach, which must be multidisciplinary, is determined by 3 aspects: the risk of stent thrombosis (particularly in the suspension of DAPT), the consequences of a delay in the intervention, and, finally, the risk of bleeding and its consequences.
We must highlight some novel points that these guidelines add to the few recommendations that can be found in other previous documents. First, the authors refer to the generational differences in the DESs. As pointed out, all of the previous recommendations were made at the time of first-generation DES implantation, which had a higher risk of adverse events. These safety profiles differ considerably from those of second-generation DESs, which are associated with a lower risk of adverse events (including stent thrombosis), raising the possibility of shorter treatment durations and allowing early suspension. In addition, the document summarizes the results of registries of stent-implanted patients who require an intervention and the results of the PARIS registry14 are briefly mentioned. These registries showed that, in patients with stable coronary disease, the intervention should be delayed at least 1 month after implantation, at which time suspension of DAPT (of the P2Y12 inhibitor) seems to be safe, regardless of stent type. However, for patients with high thrombotic risk due to previous ACS, the recommendations remain for P2Y12 inhibitor cessation at 6 months. Third, the guidelines clearly establish that when the risk of bleeding exceeds the thrombotic risk, the P2Y12 inhibitor must be suspended early enough so that there is no residual platelet inhibition. Finally, the P2Y12 inhibitor should be reintroduced as soon as possible, with 48hours as the upper limit, because the thrombotic risk in these patients is increased mainly in the early moments after the surgical intervention. This decision must be made in a multidisciplinary environment.
From the pharmacological point of view, the document continues to recommend interruption of prasugrel 7 days prior to an operation and 5 days for clopidogrel and again highlights the possibility of a 3-day suspension in the case of ticagrelor. Reference is finally made to bridge therapy with intravenous agents, adding the possible use of cangrelor as an alternative to glycoprotein IIb/IIIa inhibitors. In this section, the recommendation is to avoid the use of anticoagulants to minimize bleeding.
The authors emphasize that the evidence serving as the basis for these recommendations is still very scarce because there is no specific clinical trial dedicated to this aspect, probably due to the heterogeneity and complexity of the situations and the resultant challenges facing clinical trial design in this context. However, in recent years, several national registries examining the strategy in these patients have emerged that will help to direct future recommendations.
Special PopulationsThe final section of the guidelines is dedicated to the DAPT strategy in very specific situations. The authors recommend that the type and duration of DAPT not depend on sex or the presence of diabetes mellitus. On the other hand, they advise prolonging DAPT in 3 situations: a) stent thrombosis, particularly if there are no obvious correctable causes (> 12 months, IIa B), such as lack of adherence to medical treatment or the presence of correctable mechanical factors related to stent implantation; b) concomitant peripheral vascular disease (> 12 months, IIb B), and c) complex PCI (> 6 months, IIb B).
As a novelty in these guidelines, and despite the absence of data from randomized trials, practical recommendations are presented for the treatment of bleeding in patients with DAPT and anticoagulation. In the presence of patient bleeding, the type, dose, and duration of the DAPT should be re-evaluated. In this context, the decision to suspend the 2 antiplatelet agents, particularly if the stent implantation is very recent, should be taken only if the bleeding compromises the life of the patient and cannot be treated. In this case, the patients should be transferred to a center with on-site PCI capability.
In conclusion, we consider these guidelines to be essential, particularly for daily clinical practice, and that it will contribute to a systematic approach to the management of antiplatelet agents in a group of patients whose duration of antiplatelet therapy will always be a critical issue.15
CONFLICTS OF INTERESTNone declared.
SEC Working Group for the 2017 ESC Focused Update on Dual Antiplatelet Therapy in Coronary Artery Disease, Expert Reviewers for the 2017 ESC Focused Update on Dual Antiplatelet Therapy in Coronary Artery Disease, and the SEC Guidelines Committee.
The names of all authors of this article are listed in the Appendix.