The Spanish health system has undergone spectacular development in recent decades. It now provides universal access, almost without direct costs for patients, and achieves high levels of quality and excellence. However, in parallel with other Western countries’ health systems, the Spanish system is showing signs of strain as it faces ever-greater costs as a result of the increased resources needed to meet the health care demands of an aging population, diseases converting to chronic conditions, and new treatments and technologies becoming available to a growing number of patients. These factors, together with today's budgetary constraints, make health systems extremely vulnerable, especially in the case of Spain.
THE ECONOMIC CRISIS AND THE HEALTH SYSTEMIn this scenario, health care practitioners, on the one hand, find it challenging to balance ever-increasing demand with ever-dwindling economic resources in their daily clinical practice and decision-making. Health care managers, on the other hand, have to deal with the high cost of new, technological interventions and innovations– some with limited effectiveness–, increased demand, and the major knock-on effect of longer waiting lists. Halfway along this continuum are health care practitioners with management responsibilities, who have the challenge of making the system more effective and efficient. Their aim is to make their organizations more involved and committed, optimizing benefits for patients.1
To date, the economic crisis has led to a series of short-term measures being applied solely to contain expenditure, by reducing operational and human resources, limiting service portfolios, lowering the prices or tariffs agreed with material and service providers, etc. However, if these measures remain in place in the medium- to long-term, they may have irreversible consequences, and lead to lower quality services in some cases. In recent years, health care policymakers (politicians, administrators, and managers) have focused solely on spending containment and cost efficiency, without setting strategic planning objectives. This focus means that health care practitioners work defensively, based on economic criteria. As a result, they feel uncertain and demotivated; they distrust the system. The divergence between the stakeholders’ approaches is patent. The Institute of Medicine recently proposed a new definition of health care quality, understood as a reduction in the overuse, misuse, or underuse of services. This definition can be interpreted and then translated into the stakeholders’ language, creating a shared vision to work toward the goal of common quality.2
To date, policymakers have chosen a certain model (generally involving a combination of health care settings and practitioners, new processes, and new technologies) and have promised to achieve global improvements in quality and costs. However, the successful implementation of a new model depends on 2 local factors: effective and involved care teams and good management of care operations (known as ‘clinical microsystems’).3 Both factors require strong physician leadership, but consensus is lacking on the nature of such leadership, with regard to what needs to be done and how this can be achieved.4
CLINICAL MANAGEMENT UNITSIn addition to structural measures to increase efficiency, productivity, and quality, it appears that a set of predominantly clinical changes is essential to achieve system sustainability.5 Improved organization of clinical processes will clearly enhance health outcomes, and this improvement depends on clinical leadership. Health care professionals continually make clinical decisions that have significant economic implications. This is a vital point. It is the physicians who decide, control, and influence almost all health care expenditure. Changes in hospital organization that aim to achieve true decentralization and autonomy, and stronger clinical leadership powers (so that practitioners hold shared responsibility for resource management) should lead to an improved health care outcome in quantitative and qualitative terms.6
Traditionally, physicians have been trained with a focus on developing high professional standards to respond to patients’ needs–regardless of the costs involved–and to make personalized decisions. In parallel, there has been an explosion of knowledge that is a key determinant of increased costs, due to the introduction of new drugs, novel devices, innovative diagnostic tests, and new indications. Focusing on patients’ needs, developing high professional standards, and keeping up to date in medical advances are the first steps toward responsibility in a medical service. However, even in a hospital setting, these 3 pillars are insufficient to ensure quality of care. Integrating information and teamwork across different medical services, bodies, or health care levels is a vital cornerstone in clinical management today. This cornerstone can be strengthened and health care system sustainability can be enhanced through performance improvement in care processes, stronger physician leadership and implementation of clinical management.7 For this reason, the concept of clinical management has been revisited in recent years to study its role as an essential instrument for increasing efficiency. There is consensus that organizational care units need to be process-centered, patient-centered, evidence-based, and coordinated among the difference care levels.5 One way to achieve these objectives is to strengthen and devolve care management to clinical management units (CMUs). The ultimate goal of a CMU is to integrate decision-making in certain care processes, manage resources, and increase hospital service quality control.
CLINICAL MANAGEMENT LEVELSMany health care professionals have an incomplete understanding of the concept of CMUs, their objectives, implementation, and applicability. The concept of clinical management is often used across a wide range of clinical scenarios, hindering proper understanding and masking the potential for implementation.
Cardiac CMUs should centralize related disciplines and activities that are essential in cardiology and heart surgery, sharing organization and budgets at a functional level. There are several reasons why cardiac care is a perfect candidate for a CMU: a) it has clinically-related categories, which share well-defined care processes; b) these categories are closely related at a functional level, thus facilitating operations, communication and a common strategy; c) heart procedures, despite being complex, are largely independent of central hospital services; d) cost/quality analysis measurements are simple and easily traceable, and e) in tertiary teaching hospitals, cardiac care has a major impact on the hospital activity and budget.
This favorable context explains why reports have already been published on CMU experiences in heart clinics and hospitals in Spain and abroad.8–10 However, although CMUs are feasible from a theoretical point of view, many of these experiences have only been short-lived. There are many determinant factors, including legal obstacles, inflexible budget and compensation models, resistance to change, limited information systems, and a lack of political commitment.1
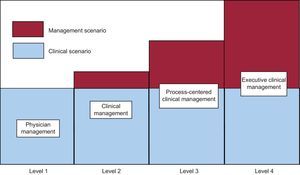
The Figure and Table show a simple classification of the progressive levels that can be implemented in clinical management, defining objectives, and the scope of applicability and responsibilities at each level. The levels reflect incremental management autonomy in an on-going, shared clinical or care activity scenario. A management action may be confined to the most basic level (level 1: physician management), in which the physician's goal is to solve a number of care needs that do not have economic implications. A management action that extends to a more complex scenario (level 4: executive clinical management) includes comprehensive budget management, and an all-inclusive human resources policy. It entails financial risk. Level 4 involves management and administration of all the human, material and economic resources in the units and services belonging to a specific care activity area.
Classification of the possible progressive levels in clinical management, objectives, and scope of applicability at each level. Level 1: The objective is focused on patients’ and physicians’ needs, and knowledge updates. It applies only to physicians. Level 2: The objective is to assess performance, and clinical and economic outcomes. Economic management is limited. It applies to physicians and nursing staff. Level 3: The objective is multi-specialty, interdisciplinary, and process-based. It involves budget management. It applies to all staff (physicians, nurses, ancillary staff, etc.). Level 4: The objective is management of the entire clinical unit. Budget management entails financial risk. This level has its own, complete human resources policy. It applies to all staff.
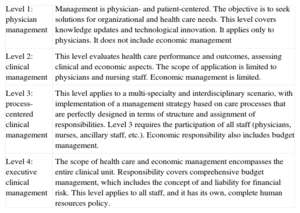
Clinical Management Classification
| Level 1: physician management | Management is physician- and patient-centered. The objective is to seek solutions for organizational and health care needs. This level covers knowledge updates and technological innovation. It applies only to physicians. It does not include economic management |
| Level 2: clinical management | This level evaluates health care performance and outcomes, assessing clinical and economic aspects. The scope of application is limited to physicians and nursing staff. Economic management is limited. |
| Level 3: process-centered clinical management | This level applies to a multi-specialty and interdisciplinary scenario, with implementation of a management strategy based on care processes that are perfectly designed in terms of structure and assignment of responsibilities. Level 3 requires the participation of all staff (physicians, nurses, ancillary staff, etc.). Economic responsibility also includes budget management. |
| Level 4: executive clinical management | The scope of health care and economic management encompasses the entire clinical unit. Responsibility covers comprehensive budget management, which includes the concept of and liability for financial risk. This level applies to all staff, and it has its own, complete human resources policy. |
Regardless of the target clinical management level, a number of factors are essential for a successful outcome,11 some of which have already been mentioned (leadership, team work, patient-centered care, integrated care processes, etc.). Other key factors for CMUs are an outcome-centered approach, analysis of professional skills, and continuous development models, together with a capacity for self- and external assessments. The ultimate success of these projects depends on managers and practitioners having common objectives that are formally drawn up in a management agreement. Hospital managers should encourage health care process improvement and support CMU operations. Practitioners, for their part, should shoulder the responsibility of decision-making in clinical and administrative processes, and in the use of allocated resources.
CLINICAL MANAGEMENT UNITS, PROPOSED CHANGES, AND SYSTEM SUSTAINABILITYTo increase the efficiency, productivity, and quality of the health care system, a number of changes have been proposed that are essential if sustainability is to be achieved in the medium-term.12 The common denominator of these changes is improved efficiency and a more rational distribution of resources to match capacity, activity, and quality. One change that has been put forward to increase efficiency is to devolve management to CMUs. This change breaks with the current situation, and is a central component for sustaining and facilitating subsequent implementation of other proposed changes. Management autonomy means that professionals will have to switch from simply measuring their care activity to analyzing and rethinking care and management outcomes as a team, identifying thriving areas and processes and those that need improvement. To achieve this change in attitude, it is essential to involve health care professionals in the analysis and discussion process by identifying best practices and ineffective or inefficient practices, assigning resources to specific interventions that achieve the best outcomes, and implementing innovative organizational strategies in the multidisciplinary team itself.13 These key factors will position CMUs clearly at the center of this proposed change to increase health care system quality and improve transparency, thus providing a benchmarking system for clinical and nonclinical outcomes. It has been shown that drawing direct comparisons between health care institutions and transparent feedback on outcomes contributes not just to health care quality improvement, but also to significant resource optimization, because procedures can be adapted accordingly.14
Another proposed change involves centralizing services and integrating health care levels to reduce or eliminate duplication and improve complex care processes. Health care agencies now have access to more information, which can facilitate the introduction of structural and logistic changes, and health planning based on objective data. In this context, CMUs could be used as a tool for final decisions on activity centralization by sector. With clearly defined criteria for the organization, design, infrastructure, and management of health care units in their various dimensions,15 it will be easy to base new measures on efficiency and outcome criteria.
In conclusion, CMUs can act as a cornerstone for introducing changes that are deemed essential for increasing health care efficiency and quality, which in turn are key factors in health care system sustainability. However, it should be stressed that a CMU project needs to be designed with a specific clinical management level in mind, thus defining the initial objectives, stakeholders, and strategies involved.
CONFLICTS OF INTERESTNone declared.