To the Editor:
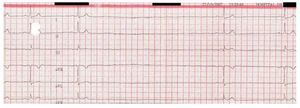
We present the case of a 72-year-old male patient examined because of repeated syncopal events. The patient had already been studied for syncope 3 years previously; in that moment, a 24-hour Holter recording and the echocardiogram were normal. He was re-examined for losses of consciousness occurring equally in active and resting moments, without a clear orthostatic or neuromediated profile, at times accompanied by abnormal movements of the mouth. He was on no medications whatsoever. The physical examination and the baseline electrocardiogram were normal and the echocardiogram did not uncover structural heart disease. Massage of the right carotid sinus was performed, which produced a cardioinhibitory response with an asystole of 5 s (Figure 1).
Figure 1. Electrocardiogram reading during the right carotid sinus massage. Note the 5-second pause.
An electroencephalogram gave a normal reading.
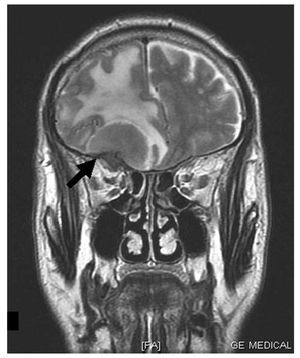
Finally, using cerebral MRI, a tumour was found in the right extraaxial frontobasal area, 34´18´35 mm, compatible with meningioma of the greater sphenoid wing, accompanied by a significant vasogenic oedema and a midline shift (Figure 2). The patient was operated and resection was performed. The definitive anatomopathologic diagnosis was of meningioma. Since then, the patient has been asymptomatic and has recovered completely. Carotid sinus massage was repeated 4 months later with negative results.
Figure 2. Cerebral MRI. T2-weighted coronal view showing the meningioma (arrow) and the significant accompanying oedema that caused the disappearance of the ipsilateral sulci and subfalcial herniation.
Carotid sinus syndrome results from hyperexcitability of the carotid sinus reflex. Its exact pathophysiology is unknown, and the 2 most widely-accepted theories attribute it to either a lesion in the nucleus of the solitary tract or to a peripheral lesion in the area of the carotid sinus baroreceptor.1,2 A third theory suggests a central lesion that interferes with ipsilateral circulation.3 Three types of response to sinus stimulation4 are identified: cardioinhibitory, with pauses of more than 3 s, mediated by vagus nerve afference; vasodepressant, with a drop in systolic arterial pressure of more than 50 mm Hg without changes in the heart rate; and cerebral, which can provoke convulsions and convulsive crises. As in our case, 2 or more mechanisms may be present in the same patient, which is known as a "mixed response."
Carotid sinus syndrome is a rare manifestation in cases of head and neck tumours.5,6 In an series of 4500 patients, only 17 presented this syndrome.7 It has been described in association with tumours, whether benign or malignant, whose location is related to reflex arc structures; in most cases, this coincides with extensive affections of the high or low area of the jugular chain. However, no human cases related with intracranial meningiomas are reported in the literature, and the few references that do exist describe cases in animals.8 Additionally, in our patient the frontal position of the mass was different from that of the nerve bundles and nuclei that make up the carotid sinus reflex arc. There is no doubt that the underlying mechanism in our case is related with the intracranial hypertension induced by the mass and its oedema. Indeed, the bradycardia associated with intracraneal hypertension (Cushing's effect) due to secondary medullary ischemia in severe cases, is well-known.
A permanent pacemaker is prescribed for patients with primary carotid sinus hypersensitivity.9 In patients with malignant head and neck tumours, it is of limited use, because the syncopal mechanism frequently includes a vasodepressor effect. For persistent cases, alternative techniques have been explored, such as surgical denervation. Our patient experienced surgical resolution, and has not needed cardiac stimulation. This case demonstrates that, in patients with syncopal events and carotid sinus system, any symptom potentially neurological in origin, even one as slight as abnormal mouth movements during syncope, requires meticulous neurological evaluation.