Heart failure is a major public health concern. The aim of this review was to estimate the burden of heart failure in Latin America.
MethodsSystematic review and meta-analysis following a search in MEDLINE, EMBASE, LILACS, and CENTRAL for articles published between January 1994 and June 2014, with no language restrictions. We included experimental and observational studies with at least 50 participants aged ≥ 18 years.
ResultsIn total, 143 of the 4792 references retrieved were included in the study. Most studies had been conducted in South America (92%), and mainly in Brazil (64%). The mean age of the patients was 60 ± 9 years, and mean ejection fraction was 36% ± 9%. The incidence of heart failure in the single population study providing this information was 199 cases per 100000 person-years. The prevalence of heart failure was 1% (95% confidence interval [95%CI], 0.1%-2.7%); hospital readmission rates were 33%, 28%, 31%, and 35% at 3, 6, 12, and 24 to 60 months of follow-up, respectively; and the median duration of hospitalization was 7.0 days. The 1-year mortality rate was 24.5% (95%CI, 19.4%-30.0%). In-hospital mortality was 11.7% (95%CI, 10.4%-13.0%), and the rate was higher in patients with a reduced ejection fraction, ischemic heart disease, or Chagas disease.
ConclusionsFew studies have evaluated the incidence and prevalence of heart failure in Latin America. High mortality and hospitalization rates were found, and the main limitation was heterogeneity between studies. The results presented provide useful epidemiologic information for decision-making related to this disease. Further studies with standardized methods and representative populations are needed in this line.
Keywords
Heart failure (HF) is a common clinical syndrome that represents the end stage of several heart diseases and is a considerable public health concern. In the United States, 1% to 2% of the adult population and up to 10% of persons aged 75 to 80 years develop HF.1,2 An acute presentation of this condition is a common reason for emergency room consultations and hospitalization in intensive care units.
Heart failure, a clinical syndrome involving changes in ventricular filling or cardiac output, can be classified as HF in which the ejection fraction (EF) is reduced (REF) or HF with a preserved EF, which includes more than 50% of all HF patients.1,3
The disease burden resulting from HF has not been precisely characterized, as there are no reliable population calculations of the prevalence, incidence, or prognosis of this condition, particularly for regions such as Latin America and the Caribbean (LAC).4,5 The problem resides partly in the variations between studies regarding the definitions for HF and the diagnostic methods used.6 As the evidence related to the epidemiology of HF in LAC is scarce and difficult to access, a systematic approach is needed to obtain all the available data in this line, with the aim of summarizing the current knowledge to serve as a guide for future research. To this end, a systematic review of the related literature and a meta-analysis were conducted to determine the burden of HF in the LAC region.
METHODSA systematic review of the published literature was carried out according to the parameters for reporting proposed in the guidelines for meta-analyses of observational studies7 and the PRISMA declaration8,9 (Table 1 and Table 2 of the supplementary material).
Information Sources and Search StrategyA literature search was conducted of articles published between January 1994 and June 2014 in the main regional and international databases—MEDLINE, EMBASE, LILACS (Latin American and Caribbean Literature in Health Sciences [Literatura Latinoamericana y del Caribe en Ciencias de la Salud]) and CENTRAL (Cochrane Library)—with no language restrictions. We also reviewed the reference lists to identify additional studies. Abstracts were included only if they contained complete information enabling their evaluation. The details of the search strategy are provided in Table 3 of the supplementary material.
Eligibility Criteria, Participants, and Measures of the ResultsThe analysis included randomized or quasi-randomized controlled studies, cohort studies, case-control studies, cross-sectional studies, and case series. Only studies containing a population > 18 years of age and at least 50 patients were included. When data were found to be duplicated in more than 1 publication, the article with the larger sample was selected. The measures calculated were the incidence and prevalence of HF, the HF hospitalization rates at 30, 60 and 90 days, 6 months, and 1 year, the duration of hospitalization by department (emergency hospitalization, hospital ward, intensive care unit), and the fatality rate (FR) at 30, 60 and 90 days, 6 months, and 1 year.
Data Collection Process, Article Selection, and Data ExtractionAll the selection and processing phases of the study were carried out using EROS.10 Pairs of reviewers independently selected the articles by evaluating the titles and abstracts according to pre-established criteria, and then extracted the relevant data. Discrepancies were resolved by consensus with the remainder of the research team. When deemed necessary, the authors of some articles were contacted to obtain supplementary information.
Evaluation of the Risk of BiasThe risk of bias was determined using the STROBE11 checklist and taking into account the information provided by articles on research methodology.12–14 The following items were evaluated: selection of the participants, control of confounding factors, measurement and reporting of the results, and conflicts of interest (Table 4 and Table 5 of the supplementary material). Independent pairs of reviewers evaluated the quality of the methods used, and discrepancies were resolved by consensus with the remainder of the team.
Statistical AnalysisA meta-analysis of proportions was carried out. Arcsine transformation was applied to stabilize the variance of the proportions.15 When heterogeneity between studies was encountered, we used the DerSimonian-Laird random effects model, which considers the variability between studies.16,17 The I2 was calculated as a measure of the combined proportion attributable to this heterogeneity.18 All analyses were performed with Stats-Direct and STATA 13.0 software.
Incidence is expressed as the incidence density; that is, the number of cases per 100000 person-years.19 If the person-years were not reported, this value was calculated by multiplying the sample size by the mean follow-up time.
Several analyses by pre-established subgroups were performed: according to the HF classification of REF (≤ 35%) or preserved EF, according to blood pressure (low/normal vs high), by HF etiology, according to whether the patient had been hospitalized for the first time or readmitted for HF, and by age (stratified into 4 groups: 18 to 39, 40 to 64, 65 to 79, and ≥ 80 years). In addition, a sensitivity analysis was conducted according to the risk of bias in the studies, and a post-hoc analysis according to the definition of HF used in the studies
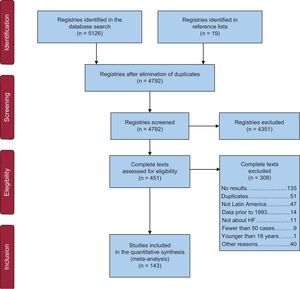
RESULTSThe search identified 4792 references, and 143 studies were ultimately included in the analysis (Figure 1). The characteristics of the studies included and their risk of bias are described in Table 5 and Table 6 of the supplementary material.
Most of the studies had been carried out in South America (92%), mainly in Brazil (64%) and Argentina (22%), and the majority had been published between 2005 and 2013. The studies included a median of 257 (range, 56 to 1 14391282) patients, with a mean age of 60.34 ± 8.98 years. The mean percentage of men was 61.07% ± 11.48%. Most of the studies (80%) included participants from specific populations, such as hospitalized patients (64%), those with REF (63%), or those in New York Heart Association functional class III-IV (59.42% ± 35.49%). As to the HF definition, the studies used clinical definitions and diagnostic methods (49%), the patients’ medical records (24%), and validated scales (15%), or this factor was not defined (6%).
The mean EF was 35.93% ± 8.58%. Most studies included more than 1 etiology (79%), but the single etiology most often evaluated was Chagas disease (ChD) (13%). The reported comorbidities included diabetes mellitus (32%), hypertension (62%), atrial fibrillation (22%), renal disease (25%), and anemia (40%).
The study designs were most commonly cohort studies (32%) and registries or surveillance studies (20.27%). A low-risk evaluation was given to 31% of the studies for selection bias, 49% for control of confounding factors, 79% for measuring and reporting the results, and 94% for possible conflicts of interest.
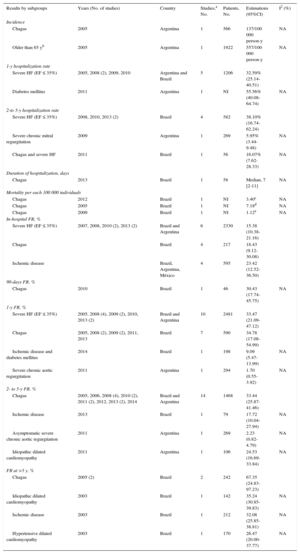
The main findings in the overall population are summarized in Table 1, and the data for specific populations, defined according to severity (EF ≤ 35%), age >65 years, and etiology (ChD, diabetes mellitus, ischemic disease, severe aortic regurgitation, idiopathic dilated cardiomyopathy, and hypertensive cardiomyopathy), are shown in Table 2. The complete reference list according to the results presented can be consulted in Table 7 of the supplementary material.
Summary of the Main Findings in the General Population
| Results | Years (No. of studies) | Country | Studies included, No. | Patients, No. | Estimations (95%CI) | I2 (%) |
|---|---|---|---|---|---|---|
| Incidence of HF | 2003 | Brazil | 1 | 1091 | 199/100 000 person-y | NA |
| Prevalence of HF, % | 1999-2009 | Antigua and Barbuda, and Cuba | 2 | 87 204 | 1.01 (0.13-2.74) | NA |
| 90-day hospitalization rate, % | 2005-2007-2009 (2)-2011-2012 | Argentina and Brazil | 6 | 2180 | 33.44 (19.50-49.05) | 97.9 |
| 6-month hospitalization rate, % | 2009-2013 | Brazil | 2 | 199 | 28.16 (9.74-51.60) | NA |
| 1-y hospitalization rate, % | 1998-2003-2005 (2)-2008 (3)-2009 (3)-2010 (2) | Argentina and Brazil | 12 | 2720 | 30.69 (25.39-36.25) | 88 |
| 2- to 5-y hospitalization rate, % | 2006-2007-2008-2009-2010 (2)-2013 (2) | Argentina, Brazil and Uruguay | 8 | 2483 | 35.24 (24.00-47.37) | 97.2 |
| Duration hospitalization (without determining the department), days | 2004 (3)-2005-2006 (3)-2007 (2)-2008 (1)-2009 (2)-2010-2011 (2)-2012 (2)-2014 | Argentina, Brazil, Chile, and Colombia | 18 | 200 378 | 7.00 [5.20-11.00] | NA |
| Hospitalization in intensive care units, days | 2006-2007-2012 | Argentina and Brazil | 3 | 833 | 6.90 [3.03-8.23] | NA |
| Emergency hospitalization, days | 2008 | Brazil | 1 | 100 | 8.45±12.90 | NA |
| Hospitalization in general wards, days | 1999-2005-2006-2007-2009-2010 (2) | Brazil, Chile, Peru and Antigua and Barbuda | 7 | 66 321 | 11.50 [10.00-19.02] | NA |
| Mortality | 2003 | Brazil | 1 | 1091 | 168.00 (83.90-300.50)/100 000 person-y | NA |
| In-hospital FR | 1998-1999 (2)-2004 (3)-2005 (2)-2006 (6)-2007 (4)-2008 (2)-2009 (3)-2010 (6)-2011-2012 (3)-2013 (3)-2014 | Antigua and Barbuda, Argentina, Brazil, Chile, Colombia and Mexico | 37 | 759 636 | 11.67% (10.39-13.02) | 99.5 |
| 60-day FR | 2011 | Brazil | 1 | 89 | 11.24% (5.52-19.69) | NA |
| 90-day FR | 2005-2006-2009 (2)-2010-2012 | Argentina and Brazil | 6 | 1856 | 17.26% (11.72-23.62) | 88.4 |
| 6-month FR | 2006-2008-2009 | Argentina and Brazil | 3 | 3128 | 24.00% (7.78-45.59) | 92.1 |
| 1-y FR | 1998-2003 (2)- 2005 (2)-2007-2008 (4)-2009 (5)-2010 (4)-2011-2012 (2)-2013 (2) | Argentina, Brazil, Chile and Jamaica | 25 | 7714 | 24.52% (19.42-30.02) | 96.6 |
| 2- to 5-y FR | 2006 (2)- 2007 (4)- 2008 (3)- 2009 (5)- 2010 (3)- 2011 (4)-2012 (4)-2013 (3)-2014 (3)-2015 | Argentina, Brazil, Chile, Mexico, Cuba and Uruguay | 32 | 11 425 | 27.22% (22.51-32.18) | 97 |
| FR at > 5 y | 2005-2009-2010 (2)-2011 | Argentina, Brazil and Chile | 5 | 4745 | 47.43% (36.55-58.43) | 98.2 |
95%CI, 95% confidence interval; FR, fatality rate; HF, heart failure; NA, not applicable.
The bibliographic references for the studies are summarized in Table 7 of the supplementary material, which shows the complete references according to the results presented in this table.
Unless otherwise indicated, data are expressed as mean ± standard deviation or median [interquartile range].
Summary of the Main Findings in Specific Populations
| Results by subgroups | Years (No. of studies) | Country | Studies,a No. | Patients, No. | Estimations (95%CI) | I2 (%) |
|---|---|---|---|---|---|---|
| Incidence | ||||||
| Chagas | 2005 | Argentina | 1 | 566 | 137/100 000 person-y | NA |
| Older than 65 yb | 2005 | Argentina | 1 | 1922 | 557/100 000 person-y | NA |
| 1-y hospitalization rate | ||||||
| Severe HF (EF ≤ 35%) | 2005, 2008 (2), 2009, 2010 | Argentina and Brazil | 5 | 1206 | 32.59% (25.14-40.51) | |
| Diabetes mellitus | 2011 | Argentina | 1 | NI | 55.56% (40.08-64.74) | NA |
| 2-to 5-y hospitalization rate | ||||||
| Severe HF (EF ≤ 35%) | 2008, 2010, 2013 (2) | Brazil | 4 | 582 | 38.10% (16.74-62.24) | |
| Severe chronic mitral regurgitation | 2009 | Argentina | 1 | 269 | 5.95% (3.44-9.48) | NA |
| Chagas and severe HF | 2011 | Brazil | 1 | 56 | 16.07% (7.62-28.33) | NA |
| Duration of hospitalization, days | ||||||
| Chagas | 2013 | Brazil | 1 | 58 | Median, 7 [2-11] | NA |
| Mortality per each 100 000 individuals | ||||||
| Chagas | 2012 | Brazil | 1 | NI | 3.40c | NA |
| Chagas | 2005 | Brazil | 1 | NI | 7.18d | NA |
| Chagas | 2009 | Brazil | 1 | NI | 1.12e | NA |
| In-hospital FR, % | ||||||
| Severe HF (EF ≤ 35%) | 2007, 2008, 2010 (2), 2013 (2) | Brazil and Argentina | 6 | 2330 | 15.38 (10.38-21.16) | |
| Chagas | Brazil | 4 | 217 | 18.43 (9.12-30.08) | ||
| Ischemic disease | Brazil, Argentina, México | 4 | 595 | 23.42 (12.52-36.50) | ||
| 90-days FR, % | ||||||
| Chagas | 2010 | Brazil | 1 | 46 | 30.43 (17.74-45.75) | NA |
| 1-y FR, % | ||||||
| Severe HF (EF ≤ 35%) | 2005, 2008 (4), 2009 (2), 2010, 2013 (2) | Brazil and Argentina | 10 | 2481 | 33.47 (21.09-47.12) | |
| Chagas | 2005, 2008 (2), 2009 (2), 2011, 2013 | Brazil | 7 | 590 | 34.78 (17.08-54.99) | |
| Ischemic disease and diabetes mellitus | 2014 | Brazil | 1 | 198 | 9.09 (5.47-13.99) | NA |
| Severe chronic aortic regurgitation | 2011 | Argentina | 1 | 294 | 1.70 (0.55-3.92) | NA |
| 2- to 5-y FR, % | ||||||
| Chagas | 2005, 2006, 2008 (4), 2010 (2), 2011 (2), 2012, 2013 (2), 2014 | Brazil and Argentina | 14 | 1468 | 33.44 (25.87-41.46) | |
| Ischemic disease | 2013 | Brazil | 1 | 79 | 17.72 (10.04-27.94) | NA |
| Asymptomatic severe chronic aortic regurgitation | 2011 | Argentina | 1 | 269 | 2.23 (0.82-4.79) | NA |
| Idiopathic dilated cardiomyopathy | 2011 | Argentina | 1 | 106 | 24.53 (16.69-33.84) | NA |
| FR at >5 y, % | ||||||
| Chagas | 2005 (2) | Brazil | 2 | 242 | 67.35 (24.83-97.23) | |
| Idiopathic dilated cardiomyopathy | 2003 | Brazil | 1 | 142 | 35.24 (30.85-39.83) | NA |
| Ischemic disease | 2003 | Brazil | 1 | 212 | 32.08 (25.85-38.81) | NA |
| Hypertensive dilated cardiomyopathy | 2003 | Brazil | 1 | 170 | 26.47 (20.00-37.77) | NA |
95%CI, 95% confidence interval; EF, ejection fraction; FR, fatality rate; HF, heart failure; NA, not applicable; NI, not indicated.
The complete bibliographic references for the studies are shown in Table 7 of the supplementary material.
A population study of Brazilian cohorts reported an HF incidence of 199 cases per 100000 person-years. Two cohort studies in Argentina (1 in patients with ChD and another in patients older than 65 years) described an HF incidence of 137 and 557 per 100 000 person-years, respectively. Because of the heterogeneity of the study populations, their results were not combined (Table 7 of the supplementary material1–3).
PrevalenceThree population studies (2 from Cuba and 1 from Antigua and Barbuda) have reported the prevalence of HF. One of the Cuban studies described a high prevalence of 10.8% (95% confidence interval [95%CI], 9.75%-13.16%), but it was not included in the final meta-analysis because it did not apply probability sampling. The meta-analysis of the remaining studies showed a combined prevalence of 1.01% (95%CI, 0.13%-2.74%) (Table 7 of the supplementary material4–6). Furthermore, 2 studies reported the prevalence of HF in patients with an acute coronary syndrome, which showed a combined value of 7.88% (95%CI, 7.16%-8.62%) (Table 7 of the supplementary material7,8).
HospitalizationThe meta-analysis of hospitalization rates at 90 days, 6 months, 1 year, and 2 to 5 years yielded combined values of 33.44% (95%CI, 19.50%-49.05%), 28.16% (95%CI, 9.74%-51.60%), 30.69% (95%CI, 25.39%-36.25%), and 35.24% (95%CI, 24.00%-47.37%), respectively. In addition, some studies reported these values in patients with severe HF, severe chronic mitral regurgitation, and ChD with severe HF (Table 2).
Four studies that used validated scales to define HF reported a 1-year hospitalization rate of 31.94% (95%CI, 17.08%-48.97%; I2, 91.7%), and 5 studies that had a low risk of participant selection bias showed a rate of 25.73% (95%CI, 19.10%-32.97%; I2, 95.6%) (Table 7 of the supplementary material9–48).
Duration of HospitalizationIn studies reporting intensive care unit admittance for HF, the median duration of hospitalization was 6.9 days, with 11.50 days in general wards, and 8.45 days in emergency hospitalization. Eighteen studies in which the hospitalization area was not reported cited a median duration of 7.0 days (Table 7 of the supplementary material49–77).
MortalityOne population study conducted in Brazil and including multistage probability sampling reported a mortality rate of 168.00 (95%CI, 83.90-300.50) per 100000 person-years.
Five registries and surveillance studies performed in Brazil and 1 in Argentina provided data on yearly mortality due to HF per each 100 000 inhabitants. A nationwide registry from Argentina, with data collection from 1995 to 2005 showed a 22.95% reduction in mortality in the population older than 35 years. One Brazilian study described a 71% decrease in mortality from 1992 to 2008 in São Paulo and another showed a decrease occurring from 1992 to 1995 in Salvador de Bahia. Finally, a study carried out in Rio de Janeiro, São Paulo, and Rio Grande do Sul reported higher mortality in men older than 50 years (Table 7 of the supplementary material78–87).
In-hospital fatality ratesThe combined in-hospital mortality in 37 studies was 11.67% (95%CI, 10.39%-13.02%).
Eight studies that used validated scales to define HF showed a 1-year FR of 12.78% (95%CI, 10.43%-15.33%; I2, 56.4%), and 13 with a low risk of participant selection bias reported an FR value of 14.13% (95%CI, 9.22%-19.88%; I2, 97.6%).
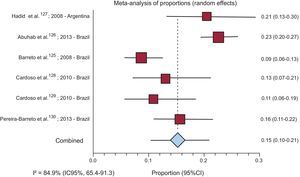
Four studies reporting the in-hospital FR in patients with ChD yielded a combined rate of 18.43% (95%CI, 9.12%-30.08%), and 6 studies reporting the FR in patients with REF described a value of 15.38% (95%CI, 10.38%-21.16%) (Figure 2 and in Table 7 of the supplementary material 88–138).
In-hospital mortality in patients with heart failure and ejection fraction ≤ 35% (random effects). The references are listed in Table 7 of the supplementary material. 95%CI, 95% confidence interval.
Only a single study from Brazil described mortality at 60 days, with a value of 11.24% (95%CI, 5.52%-19.69%). Mortality at 90 days, 6 months, 1 year, 2 to 5 years, and >5 years yielded combined rates of 17.26% (95%CI, 11.72%-23.62%), 24.00% (95%CI, 7.78%-45.59%), 24.52% (95%CI, 19.42%-30,02%), 27.22% (95%CI, 22.51%-32.18%), and 47.43% (95%CI, 36.55%-58.43%), respectively.
Four studies that used validated scales to define HF showed a 1-year FR of 20.06% (95%CI, 12.05%-29.51%; I2, 80%), and 6 studies reported a 2- to 5-year FR of 24.96% (95%CI, 15.20%-36.21%; I2, 92.9%).
The 9 studies having a low risk of participant selection bias yielded a 1-year FR of 21.74% (95%CI, 14.64%-29.80%; I2, 96.8%), and 9 studies reported a 2- to 5-year FR of 30.59% (95%CI, 19.91%-42.44%; I2, 97.6%).
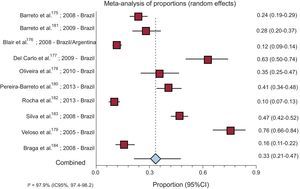
Nine studies performed in Brazil and 1 carried out in both Brazil and Argentina described a 1-year FR rate in patients with REF of 33.47% (95%CI, 21.09%-47.12%) (Figure 3).
One-year fatality rate in patients with heart failure and ejection fraction ≤ 35%. The references are listed in Table 7 of the supplementary material. 95%CI, 95% confidence interval.
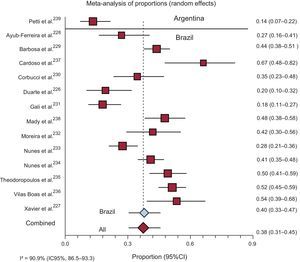
Fourteen studies provided information on the 2- to 5-year FR in patients with ChD. The combined FR in the 13 studies from Brazil was 39.92% (95%CI, 33.22%-46.82%), whereas in the single study from Argentina, the FR was 13.68% (95%CI, 6.19%-21.08%). Overall mortality was 37.83% (95%CI, 30.60%-45.34%) (Figure 4).
Two- to 5-year fatality rate in patients with heart failure and Chagas disease, by country. The references are listed in Table 7 of the supplementary material. 95%CI, 95% confidence interval.
Six studies reported the 1-year FR in ChD patients. Two studies evaluating patients with severe HF (EF ≤ 35%) reported a combined 1-year FR of 62.76% (95%CI, 51.88%-73.03%), and 4 studies in patients with EF > 35% yielded a 1-year FR of 33.30% (95%CI, 20.23%-47.84%) (Table 7 of the supplementary material139–250).
DISCUSSIONThis study provides a summary of the available evidence on the HF burden in LAC. The single population study including data on the incidence of HF was from Brazil, and it reported values similar to those seen in studies from the Unites States, a rate of 310 cases per 100 000 person-years20 (564 men and 327 women per 100 000 person-years21). As would be expected, our review found a higher incidence of HF in elderly populations, in agreement with the findings from other studies.22–24
Our prevalence estimate was 1.01%, a value similar to that of the REACH study25 (0.4-1.4%) and in line with the American Heart Association statistics26 (2%). Nonetheless, other reports from the United States and Europe have cited higher values (1%-14%).22,24,27 The reliability of the prevalence estimates is limited by differences in the approaches used to diagnose HF and the age of the populations included. For example, some studies applied validated scales to classify HF, others used clinical definitions and patient reporting, and some relied on hospital discharge records.22 It is known that the number of HF cases will rise in the coming years, although the incidence will decrease because of the growing elderly population28 and the epidemics of HF risk factors in LAC, reflected in studies by the Centro de Excelencia en Salud Cardiovascular para América del Sur (South American Center for Excellence in Cardiovascular Health, CESCAS),29 the Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA),30 and the Latin American Consortium of Studies in Obesity (LASO).31,32
Hospital readmissions imply a huge burden on health care systems and society in general, and they are partly the result of poor adherence to the guidelines for HF, especially in LAC.33,34 The hospitalization rates and duration of hospital stay found in our review are similar to the values reported in studies from the United States and Europe.25,35–38
One nationwide study carried out in Argentina and including data from 1999 to 2005 reported a decrease in HF mortality (Table 7 of the supplementary material79). In Brazil, a population cohort study performed in the 1990s described a crude HF mortality rate of 168 per 100 000 person-years, whereas in the United States the age-standardized total death rate in 2009 was 82.3 per 100 000 person-years.26 These disparities may be related to differences in the adherence to treatment, hospitalization rates, and the multifactorial etiology of HF in elderly patients. In Brazil a drop in mortality due to ChD-related cardiomyopathy was observed between 1985 and 2006.39 Coordinated campaigns to control transmission through vectors and blood transfusions have contributed to this reduction.40
In the present study, in-hospital mortality was estimated at 11.67% and was higher in patients with REF (15.38%). Patients with ischemic disease and Chagas-related disease also showed a poorer prognosis (23.42% and 18.43% mortality, respectively). These rates are higher than those observed in other studies, which have reported a decrease in in-hospital mortality.37,38,41
Based on the data from 6 studies conducted in Argentina and Brazil, the combined 90-day HF mortality rate was 17.26%, and was higher (30.40%) in patients with ChD. Although these rates are higher than those reported in other countries in the-short term, they appear similar in the long term, which likely reflects not only the differences inherent to patients with HF but also differences in the health systems involved. Furthermore, the FR was comparable to the reported rates in other publications.22,42
The epidemiology of myocardial infarction has changed considerably over the last 2 decades due to the increase in non—ST-segment elevation myocardial infarction, improved treatment methods, and decreases in mortality rates in the short-term.43 The substantial drop in mortality has led to an increasing percentage of HF survivors. It has been calculated that 7.9% of patients with an acute coronary syndrome experience HF. However, we found no studies reporting the incidence of HF in patients with ischemic heart disease.
Reliable data are lacking on the etiology of HF in the LAC region, as the cause is not determined in around one-third of cases. The etiologies most commonly cited are ChD (36%) and ischemic heart disease (35%), although these values should be interpreted with caution, as they are not based on population studies (Table 6 of the supplementary material). The prevalence of coronary disease has been described at 68% in some randomized controlled trials in the United States,44 and a population-based study performed in 1999 in Britain reported that coronary disease led to HF in 36% of cases.45 These differences in the etiology of HF are not surprising considering the high prevalence of ChD in South America.
Data on the epidemiology of HF in patients with PEF are scarce, both worldwide and in the LAC region. However, the prevalence of preserved EF in HF patients from LAC was found to be 69% in the I PREFER46 study.
Limitations and StrengthsOur study has several limitations. Although we sought published evidence and unpublished data indexed in electronic databases, certain “grey” literature such as HF registries may have been omitted. Furthermore, we encountered high heterogeneity, even in the analyses by pre-established subgroups. This clinical heterogeneity may partly be explained by variations in the definitions of HF and selection of participants, as well as considerable variability in the prevalence of risk factors in the LAC region.34 Nonetheless, the sensitivity analysis exclusively including studies using validated scales and those with a low risk of selection bias showed no significant differences compared with the primary analysis. Although a random effects model was used to minimize this typical problem in epidemiologic reviews, the main estimates should be taken with caution and the confidence intervals considered the best approximation to the true situation. This approach takes advantage of the strength of the meta-analytic technique, in which statistical precision is increased through weighting of the individual studies, thus yielding more informative results than a mere description of the dispersion parameters or the values obtained in each primary study. Perhaps the main limitation is the scarcity of studies with adequate methodological quality performed in the region, as most of the information has been extracted from nonrepresentative samples and from a small number of countries. This paucity of information should be emphasized: most of the studies identified were conducted in Brazil or Argentina, countries with relatively high per capita incomes for the region. Although HF is a common disease, there is very little related information on the epidemiology of this condition from population studies. Furthermore, most of the studies enrolled hospitalized patients; hence, the available evidence is mainly related to patients with more severe symptoms and a poorer EF.
Despite these limitations, our study has several strengths. One of them is the strict methodology used,7–9 including a highly sensitive search strategy. Consequently, our systematic review exceeds the scope of previous narrative reviews by including a much larger number of references.34 Furthermore, whenever possible, we performed an analysis by subgroups with pre-established sensitivity, and a meta-analysis of the most highly comparable studies.
CONCLUSIONSHeart failure is a common syndrome in the LAC region, but there is a paucity of related data from high-quality population studies, especially regarding the incidence and prevalence of this condition. The causes of HF reported in the studies identified (mainly hospital-based), were mainly ChD and ischemic heart disease, but the heterogeneity found indicates that the results should be interpreted with caution.
Hospitalization rates are high in patients with HF. A trend toward a decrease in mortality was seen, although the values are still high, particularly in patients with poorer EF values, ischemic heart disease, and ChD.
The results of our study focusing on HF in Latin America may be of help for designing effective preventive strategies and therapies to address the growing health concern generated by this condition.
Latin America and the Caribbean require additional studies in this line that have adequate methodological quality, include representational samples, use valid diagnostic criteria for HF, and report data separately by sex, age, etiology, EF status, and other relevant prognostic factors.
FUNDINGIndependent grant from Novartis Argentina, S.A., and Instituto de Efectividad Clínica y Sanitaria, Buenos Aires, Argentina.
CONFLICTS OF INTERESTNone declared.
- –
Few population studies have focused on the epidemiology of HF in Latin America. The main causes of this condition are ischemia and idiopathic dilated cardiomyopathy, valvular disease, hypertension, and Chagas cardiomyopathy. Chagas is involved in 41% of HF cases in endemic areas and is associated with the poorest prognosis.
- –
The region studied has to face not only the risk factors and epidemiology of HF seen in developed countries, but also that of Chagas-related disease.
- –
Heart failure causes 6.3% of deaths and the majority of hospitalizations in affected patients.
- –
Following a comprehensive systematic literature search, a single population study was found reporting the incidence of HF (199 cases per 100 000 person-years) and 2 studies describing the population prevalence (around 1%). Few population studies performed with high-quality methods have focused on these epidemiologic aspects.
- –
Among the studies identified (mainly conducted in hospitalized patients), HF mainly results from ChD and ischemia. The hospitalization and mortality rates of patients with HF are markedly high, particularly HF caused by the above-mentioned etiologies and HF in patients with systolic dysfunction.
- –
Our study provides data that may be of help in decision-making in Latin America, aimed toward designing preventive strategies and therapeutic approaches to cope with the growing health concern associated with HF.