The available information regarding blood pressure control in women is scarce. This study was aimed at assessing blood pressure control and predictors of a lack of blood pressure control in the primary care setting in a large sample of hypertensive women.
MethodsWomen aged 65 years or older with an established diagnosis of hypertension (≥6 months of evolution) were included in a cross-sectional, multicenter study. Blood pressure readings were taken following the current guidelines, and the value for each visit was the average of two separate measurements. Adequate blood pressure control was defined as <140/90mmHg (<130/80mmHg for diabetics).
ResultsA total of 4274 hypertensive women (mean age: 73.6 years [6.1 years]) were included in the study; blood pressure was controlled in 29.8% (95% confidence interval: 28.4%-31.1%) of the study population. Combined therapy was administered in 67.6% of patients (46.3% with 2 drugs and 21.7% with 3 or more drugs). The most common organ damage was left ventricular hypertrophy (33.8%) and the most common associated condition was heart failure (19%). Poor blood pressure control was more frequent in patients with more cardiovascular risk factors, organ damage, and associated clinical conditions (P<.01). A more recent hypertension diagnosis, LDL-cholesterol >115mg/dl, monotherapy, obesity, and hemoglobin A1c ≥7% were associated with a lack of blood pressure control (P<.0001).
ConclusionsOnly 3 in 10 hypertensive women aged ≥65 years monitored daily in the primary care setting achieved their blood pressure goals. A recent diagnosis of hypertension was the main predictor of poor blood pressure control.
Keywords
.
INTRODUCTIONArterial hypertension (AHT) is an important cardiovascular risk factor (CVRF) and a powerful indicator of survival risk. The prevalence of this condition in the general population in Spain is approximately 35% in people older than 18 years, and reaches a rate of 68% in people older than 60 years.1 The age distribution of AHT has a growing tendency, with important variations between sexes. The highest prevalences are observed in women older than 55 years of age.2 Arterial hypertension is the foremost cause of strokes and is one of the primary causes of ischemic heart disease and heart failure.3 Additionally, cardiovascular disease (CVD) is the primary cause of death in women in Spain.4
In spite of the fact that vascular diseases, and coronary diseases in particular, are still considered to be a characteristically male phenomenon, the role of these diseases varies between the sexes.5 For example, the risk of heart failure related to AHT is greater in women than in men,6 and women currently suffer a higher mortality rate from this disease than men.7 The fact that many doctors continue to consider CVD as a primarily male disease could be due to the fact that men commonly have more coronary risk factors and that women are less frequently included in clinical trials.8 Recently, the European Society of Cardiology (ESC) promoted the “Women at Heart” program, with the objective of increasing education and research on CVD.9 In this sense, an analysis of registries from the AHT section (Sección de Hipertensión Arterial) of the Spanish Society of Cardiology (Sociedad Española de Cardiología) including 50 000 hypertensive patients (45% female) concluded that women from the various studies had a worse risk profile than men. There were also differences in the diagnostic and therapeutic approaches that could at least partly justify the worse prognosis for CVD observed in women.10
These data, along with the poor AHT control evidenced by surveys carried out in Spain in the primary care (PC) setting involving both men and women,11, 12 justify the actions taken towards improving the overall understanding of CVRF in women and, more specifically, the treatment and control of AHT.
The primary objective of the MERICAP study is to research the prevalence of hidden or unrecognized heart failure using the Framingham clinical criteria in hypertensive women older than 65 years who sought treatment in the PC setting.13 One of the secondary objectives of the study is to quantify the level of control for blood pressure (BP) in the study population and to determine the associated factors.
METHODSWe designed a cross-sectional, multicenter study involving patients diagnosed with AHT who were treated in normal clinical practice in the PC setting in the Spanish health system. We calculated the sample size according to the primary objective of the study (to assess the prevalence of hidden or unrecognized heart failure according to the Framingham clinical criteria in hypertensive women aged ≥65 years).
A study sample of 4235 patients would obtain a precision of ±1.5% for the proportion of hypertensive women aged ≥65 years with hidden heart failure with a 95% confidence interval (CI). Assuming that 15% of patients are not viable study subjects, the total number of patients needed rose to approximately 4982.
We carried out the fieldwork between June and December 2007, with the participation of 1066 family doctors proportioned according to the population of each province. Each doctor selected a maximum of 5 consecutive patients.
The inclusion criteria used were women aged ≥65 years with a diagnosis of AHT who signed the informed consent form to participate in the study. We excluded patients with recently diagnosed AHT (within the last 6 months). The study protocol was approved by the ethics committee in the Hospital Clínico de Barcelona.
Information for the following variables was collected by each doctor using the patients’ clinical histories:
PatientsSociodemographic variables,14 CVRF, target organ damage, and associated CVD were all recorded as per the directives of the European Societies of Hypertension and Cardiology (ESH/ESC).15 We considered target organ damage to be the presence of left ventricular hypertrophy as evaluated by ECG (Sokolow-Lyon >38mm, Cornell >2440 mmxms) and/or echocardiogram (left ventricular mass index ≥110g/m2); kidney function deterioration (serum creatinine levels between 1.2mg/dl and 1.4mg/dl); microalbuminuria (30-299mg/24h, >20-199mg/l); albumin/creatinine ratio >30-299mg/g); and glomerular filtration rate (simplified MDRD [Modification of Diet in Renal Disease]<60ml/min/1.73 m2). Obesity was diagnosed when the body mass index was ≥30, abdominal obesity when the abdominal circumference was >88cm,15 and dyslipidemia when total cholesterol was >190mg/dl or low-density lipoproteins (LDL) >115mg/dl or high-density lipoproteins (HDL)<46mg/dl or triglycerides >150mg/dl.15 Diabetes mellitus was recorded when this condition was registered in the patient clinical history. Metabolic syndrome was diagnosed using the criteria established by the Adult Treatment Panel III (ATP-III) of the National Cholesterol Education Program.16 Patients were considered tobacco smokers if they had smoked at least 1 cigarette per day within the preceding month,17 and “nonsedentary” was defined as the patient who was actively walking for at least half an hour per day or practiced sports at least 3 times per week.18 Serum biochemical analyses were obtained from the clinical histories; a new laboratory test was performed under standard clinical protocols if the previous results were more than 6 months old.
Blood PressureBlood pressure was measured according to the recommendations of the Spanish Hypertension Society-Spanish League for the Fight Against Arterial Hypertension (Sociedad Española de Hipertensión-Liga Española para la Lucha contra la Hipertensión Arterial).19 After the patient spent 5min at rest, 2 sitting measurements were taken 2min apart, and the arithmetic mean of the 2 BP values was calculated. In the case of differences ≥5mmHg between measurements, a third was taken. A recently calibrated mercury-based or aneroid sphygmomanometer was used for the measurements, or an automated electronic device. Good AHT control (optimal control) was considered when the mean values for systolic BP (SBP) and diastolic BP (DBP) were <140mmHg and <90mmHg, respectively (<130/80mmHg for diabetic patients).
Antihypertensive TreatmentThe class and number of each antihypertensive drug subgroup used in the treatment of AHT were registered, as well as treatments for other conditions (diabetes mellitus, dyslipidemia, and associated CVD).
Data QualityThe data were recorded by the researcher in the data notebook. The database included ranges and guidelines for internal coherence to guarantee data quality control.
Statistical AnalysisWe performed all statistical analyses on a single sample of patients including all those that fell within the selection criteria. The analyses related to the primary study variable (level of AHT control) considered only those patients with a value for this variable.
Results were expressed as frequencies and percentages for qualitative variables and as a mean±standard deviation for quantitative variables. We also calculated 95% CI for the following variables: BP control, SBP control, DBP control, and the odds ratio (OR) value for the regression model, assuming normality and using an exact method for small samples.20 We compared quantitative variables between patient subgroups using parametric tests (Student's t-test or ANOVA) and nonparametric tests (Mann-Whitney or Kruskal-Wallis) according to the characteristics of each study variable. We used χ2 tests for qualitative variables.
A P-value <.05 was considered significant. In order to assess which variables were associated with poor control of AHT (BP≥140 and/or ≥90mmHg), we used a nonconditional logistic regression (Enter method). The study variables were age (younger than 75 years/75 years or older), obesity, CVRF (tobacco smoking, sedentary lifestyle, abdominal obesity, diabetes mellitus, dyslipidemia, family history of CVD, damage to target organs, associated clinical diseases, age of AHT), laboratory parameters (hemoglobin A1c [HbA1c], total cholesterol, LDL, creatinine, glomerular filtration rate), and antihypertensive treatment (monotherapy/combined therapy). The selection criteria for each variable was based on the statistical significance of the bivariate analysis with respect to BP control and the statistical significance of this relationship as expressed by authors from previous studies (tobacco use, CVD, and family history of CVD).21, 22 We performed all statistical analyses using SAS statistical software (version 9.1.3).
RESULTS Description of the SampleWe evaluated a total of 5047 surveys, of which 773 (15.3%) were rejected due to noncompliance with study protocol or due to incoherent/incomplete data, resulting in a final sample size of 4274 patients. Patient ages were distributed in the following manner: 61.1% were younger than 75 years, 33.1% were aged 75 to 84 years, and 5.8% were 85 years or older. In 69.4% of patients, AHT had been diagnosed more than 5 years earlier. Table 1 shows the most relevant clinical characteristics of the study patients. The most prevalent CVRF were sedentary lifestyle (67.3%), dyslipidemia (62.4%), abdominal obesity (54.9%), and diabetes mellitus (38.6%). The most frequently observed target organ damage was left ventricular hypertrophy (33.8%), and the most prevalent associated clinical disease was heart failure (19%).
Table 1. Clinical Characteristics of the Study Patients.
| Main characteristics | |
| Age (years) | 73.6±6.1 |
| Body mass index | 29.6±4.8 |
| Abdominal circumference (cm) | 96.3±14 |
| Clinical SBP (mmHg) | 143.3±15.9 |
| Clinical DBP (mmHg) | 82.7±10 |
| Cardiovascular risk factors | |
| Family history of early CVD | 743 (17%) |
| Diabetes mellitus | 1665 (38.6%) |
| Tobacco use | 415 (9.6%) |
| Dyslipidemia | 2688 (62.4%) |
| Abdominal obesity | 1944 (54.9%) |
| Sedentary lifestyle | 2904 (67.3%) |
| Metabolic syndrome | 1718 (40.2%) |
| Target organ damage | |
| Left ventricular hypertrophy | 1456 (33.8%) |
| Deteriorated kidney function (creatinine, 1.2-1.4 mg/dl) | 689 (16%) |
| Microalbuminuria | 717 (16.6%) |
| Associated clinical disease | |
| Ischemic heart disease | 770 (17.9%) |
| Cerebrovascular disease | 550 (12.8%) |
| Heart failure | 812 (19%) |
| Kidney disease (creatinine >1.4 mg/dl) | 346 (8%) |
| Peripheral arterial disease | 578 (13.4%) |
| Advanced retinopathy (grade III/IV) | 174 (4%) |
| Antihypertensive treatment | |
| Monotherapy | 1388 (32.4%) |
| Combination of 2 or more drugs | 2886 (67.6%) |
| Laboratory parameters | |
| Glucose (mg/dl) | 116.5±35.6 |
| HbA1c (%) in diabetes mellitus | 7±1.2 |
| Total cholesterol (mg/dl) | 216.3±38.5 |
| LDLc (mg/dl) | 131.5±33.9 |
| HDLc (mg/dl) | 53.5±14.2 |
| Creatinine (mg/dl) | 1±0.3 |
| Glomerular filtration rate (MDRD) | 62.3±20.2 |
CVD, cardiovascular disease; DBP, diastolic blood pressure;HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; MDRD, Modification of Diet in Renal Disease; SBP, systolic blood pressure.
Data are expressed as mean±standard deviation or no (%).
Antihypertensive treatment was administered in monotherapy to 32.4% of patients, and the most commonly used drug types were diuretics (52.8%), angiotensin II type 1 receptor blockers (ARB-II) (51.4%), and angiotensin-converting enzyme (ACE) inhibitors (33.6%). Combinations of different drugs were being taken by 46.3% of patients, and the most frequently used were diuretics with ARB-II (40%) and diuretics with ACE inhibitors (35.2%). Finally, 38% of women were taking antiplatelet treatment, and 57.9% statins.
Blood Pressure ValuesMean SBP was 143.3±15.9 mmHg and mean DBP was 82.7±10 mmHg. We observed significant differences (P<.0001) between the different age groups, with 144/84.2mmHg (<75 years), 142.4/80.9mmHg (75 years to 84 years), and 140.5/77.6mmHg (85 years or older) for SBP/DBP, respectively.
Arterial Hypertension ControlWe observed a good level of control of both SBP and DBP in 29.8% of study patients (95% CI: 28.4%-31.1%), and good control of only SBP in 32.8% (95% CI: 31.3%-34.2%), and only DBP in 56.8% (95% CI: 55.3%-58.3%). Only 11.9% of diabetic patients had controlled BP (95% CI: 10.3%-13.4%).
Table 2 shows the clinical characteristics of controlled and uncontrolled patients. Patients without controlled BP had higher percentages of CVRF, target organ damage, and associated clinical diseases than controlled patients, with significant differences for all of them (P<.001), except for ischemic heart disease. Women with poor BP control also had higher glucose levels, total cholesterol, LDL, and creatinine, as well as lower HDL levels (P<.001). We observed no differences between these 2 subgroups with regard to antihypertensive drug treatments (monotherapy or combined therapy) or antiplatelet or lipid-lowering drugs.
Table 2. Clinical Characteristics of Patients With Good and Bad Control of Arterial Hypertension.
| Good control (no=1272) | Bad control (no=3002) | P | |
| Age (years) | 74.1±6.4 | 73.2±5.9 | <.001 |
| BMI | 29.2±4.6 | 29.8±4.9 | <.0001 |
| Obesity (BMI≥30) | 452±35.5 | 1307±43.5 | <.0001 |
| Abdominal circumference (cm) | 95.3±13.7 | 97±14.1 | <.001 |
| Clinical SBP (mmHg) | 129±7.7 | 152.7±12.5 | <.0001 |
| Clinical DBP (mmHg) | 76.3±7.4 | 87±9.1 | <.0001 |
| Glucose (mg/dl) | 102.9 (25.6) | 123.6 (39.7) | <.0001 |
| HbA1c (%) in diabetes mellitus | 6.9±1.2 | 7.1±1.2 | <.01 |
| Total cholesterol (mg/dl) | 210.1±38.7 | 220.8±39.6 | <.0001 |
| LDLc (mg/dl) | 126.8±32.9 | 135±34.4 | <.0001 |
| HDLc (mg/dl) | 54.8±14.6 | 52.8±14.1 | .0001 |
| Creatinine (mg/dl) | 1±0.3 | 1.1±0.3 | <.0001 |
| Presence of hypertension (<5 years) | 323 (25.4%) | 829 (27.6%) | NS |
| Family history of early CVD | 205 (16.1%) | 538 (17.9%) | .001 |
| Diabetes mellitus | 198 (15.6%) | 1467 (48.9%) | <.0001 |
| Tobacco use | 127 (7.5%) | 284 (11%) | <.0001 |
| Dyslipidemia | 728 (57.2%) | 1960 (65.3%) | .0001 |
| Abdominal obesity | 621 (48.8%) | 1799 (59.9%) | <.0001 |
| Sedentary lifestyle | 1096 (64.4%) | 1808 (70.3%) | <.0001 |
| Metabolic syndrome | 219 (17.2%) | 1600 (53.3%) | <.0001 |
| Left ventricular hypertrophy | 498 (29.2%) | 948 (36.9%) | <.0001 |
| Glomerular filtration rate <60 ml/min/1.73m2 | 533 (41.9%) | 1463 (48.7%) | <.0001 |
| Microalbuminuria | 238 (14%) | 474 (18.4%) | .0001 |
| Coronary disease | 320 (18.8%) | 440 (17.1%) | NS |
| Cerebrovascular disease | 190 (11.2%) | 356 (13.8%) | .0003 |
| Heart failure | 351 (20.6%) | 450 (17.5%) | .0108 |
| Kidney disease (creatinine>1.4 mg/dl) | 118 (6.9%) | 226 (8.8%) | .0285 |
| Peripheral arterial disease | 159 (9.3%) | 411 (16%) | <.0001 |
| Advanced retinopathy (grade III/IV) | 50 (2.9%) | 123 (4.8%) | .0027 |
| Monotherapy treatment | 547 (32.1%) | 841 (32.7%) | NS |
| Treatment with a combination of two antihypertensive drugs | 746 (43.8%) | 1151 (44.8%) | NS |
| Treatment with a combination of three or more antihypertensive drugs | 385 (24.1%) | 538 (22.5%) | NS |
BMI, body mass index; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDLc, high-density lipoprotein cholesterol; LDLc, low-density lipoprotein cholesterol; NS, nonsignificant difference; SBP, systolic blood pressure.
Data are expressed as mean±standard deviation or no (%).
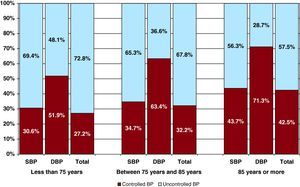
We observed significant differences in the percentages of controlled patients based on patient age (Figure 1), and that this had a favourable influence on BP control (P<.001). Upon analyzing these two variables separately (Figure 1), we observed that the percentage of patients with controlled SBP or DBP increased with age after 75 years (P<.001).
Figure 1. Percentage of patients with controlled total blood pressure, controlled systolic pressure, and controlled diastolic pressure by age groups. Good BP control: SBP <140mmHg and diastolic blood pressure <90mmHg (SBP <130mmHg and diastolic blood pressure <80mmHg in diabetic patients). BP, blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Table 3 shows the primary clinical characteristics of each age group: the oldest patients had higher percentages of target organ damage, associated clinical diseases, and combined antihypertensive drugs (P<.01).
Table 3. Main Clinical Characteristics of Patients by Age Group.
| <75 years (no=2610) | 75-84 years (no=1408) | ≥85 years (no=256) | P | |
| Left ventricular hypertrophy | 835 (32) | 519 (36.9) | 90 (36.4) | <.01 |
| Microalbuminuria | 398 (15.2) | 267 (19) | 46 (18.6) | <.01 |
| Coronary disease | 432 (16.6) | 275 (19.5) | 52 (21.1) | .02 |
| Cerebrovascular disease | 258 (9.9) | 238 (16.9) | 49 (19.8) | <.0001 |
| Heart failure | 469 (17.3) | 268 (19.1) | 51 (21) | <.0001 |
| Kidney disease (creatinine>1.4mg/dl) | 154 (5.9) | 155 (11) | 35 (14.2) | <.0001 |
| Peripheral arterial disease | 358 (13.2) | 186 (13.7) | 26 (10.5) | NS |
| Advanced retinopathy (grade III/IV) | 90 (3.4) | 71 (5) | 11 (4.5) | .04 |
| Monotherapy treatment | 953 (36.5) | 362 (25.7) | 68 (27.5) | <.0001 |
| Combined treatment with 2 antihypertensive drugs | 1113 (42.6) | 663 (47.1) | 119 (48.2) | <.01 |
| Combined treatment with 3 or more antihypertensive drugs | 500 (19.2) | 362 (25.7) | 59 (23.9) | <.0001 |
NS: nonsignificant.
Data are expressed as the total number of individuals that met criteria for each variable and a percentage for each qualitative variable.
We performed a simultaneous adjustment of the variables included in the study that were associated with poorly controlled BP using a binary logistic regression model, with a bilateral level of significance of .05 for all statistical tests. Table 4 shows the resulting variables from the final model. The most closely associated variables with poorly controlled AHT were age of AHT<5 years (OR=1.8), LDLc >115mg/dl (OR=1.5), HbA1c ≥7% (OR=1.5), family history of CVD (OR=1.4), monotherapy (OR=1.4), and abdominal obesity (OR=1.3).
Table 4. Variables Associated With Poor Control of Arterial Hypertension in The Total Population. a
| OR (95% CI) | P b | |
| AHT of <5 years duration | 1.823 (1.435-2.317) | <.0001 |
| LDLc>115 | 1.577 (1.28-1.944) | <.0001 |
| HbA1c ≥7% | 1.573 (1.274-1.943) | <.0001 |
| Family history of CVD | 1.469 (1.126-1.915) | .0046 |
| Monotherapy | 1.448 (1.147-1.829) | .0019 |
| Abdominal obesity | 1.337 (1.087-1.645) | .006 |
AHT, arterial hypertension; CI, confidence interval; CVD, cardiovascular disease; LDLc, low-density lipoprotein cholesterol; OR, odds ratio.
a Multivariate logistic regression, Enter-method (control of arterial hypertension): systolic and diastolic blood pressure ≥140mmHg and/or ≥90mmHg.
b Wald χ2 test.
We also calculated the area under the curve for poorly controlled BP, resulting in a value of 0.635. We used the Hosmer-Lemeshow goodness-of-fit statistic to analyze the calibration level for the logistic regression model, observing a nonsignificant value (χ2=3.9062; P=.8655). As a result, the model was considered to have a good fit.
We analyzed the interactions between values observed for abdominal obesity and monotherapy, less than 5 years duration of AHT and family history, and monotherapy and family history. The Akaike information criterion was the same for the model with no interactions, with minimal correlation values, and the estimates for each parameter showed no changes. Therefore, these interactions were not included in the final model.
DISCUSSIONThe results from the MERICAP study, performed using a large sample of hypertensive Spanish women aged 65 years or older and receiving drug treatment, show that an optimal control of AHT is achieved in 29.8% of patients treated in the PC setting. As in other studies,23, 24 the rate of controlled DBP (56.8%) was far greater than for SBP (32.8%).
This study was performed in a homogeneous sample, with similar sociodemographic and clinical characteristics to other studies,25, 26 which presumably reflects the characteristics of the hypertensive population aged 65 years and older that seeks attention in health centers.
To our knowledge, no previous study has focused on the level of control of AHT in the female population treated in the PC setting in Spain. This could be particularly relevant, due to the differences between men and women with regard to the presence of CVD, and its clinical characteristics, prevalence of CVRF, diagnostic testing, and drug treatment in particular.10 On the other hand, as the editors for biomedical journals have requested,27 we present here specific data for the female population in an attempt to understand the magnitude of this issue in women older than 64 years, especially in the very elderly, as we have very little information available regarding the control and management of AHT in these patients.
Although we recognize the methodological differences that exist between studies performed in patients of both sexes, our results confirm the lack of AHT control observed in previous surveys taken in PC clinical settings in Spain.23, 24, 28 Specifically, in the population aged >64 years from the PRESCAP studies,24, 25 only 3 in 10 hypertensive patients had adequately controlled BP. These results coincide with our own and are slightly more severe than those found in population surveys from Spain29 and other countries,30, 31 although we must point out that these studies were for the general population, and many patients had unknown and untreated AHT.
Various studies have provided insight into the differences in clinical characteristics and level of control of AHT based on patient sex. In general, hypertensive women included in these studies have a less favorable cardiovascular risk profile than men, with worse control of pressure values, in spite of receiving more hypertensive treatment.10 In the PRESCAP study,21 which included 10 358 patients (53.7% women), there were appreciable differences between women and men in BP control (39.7% vs 42.6%; P=.001), coexisting CVRF (sedentary lifestyle, obesity, abdominal obesity, and metabolic syndrome), and the antihypertensive treatment being administered. The VIIDA study,32 which involved 3962 high-risk patients (47.6% women), showed that more women (42% vs 48.9%; P=.001) formed part of the subgroup of patients with poorly controlled AHT (77.6%), and that the strongest predictors of poorly controlled AHT were female sex, diabetes mellitus, and obesity. Along this same line were the results from the CINTHIA study,33 including 2024 patients with a background of coronary disease, in which the rate of controlled AHT was lower in women (30.5%) than in men (44.9%). Women also had a worse lipid profile and a greater incidence of diabetes mellitus.
As expected, DBP decreased with age, whereas, contrary to other studies that included patients of both sexes,25, 26, 34, 35 SBP also decreased with age, which indicates different levels of AHT control in different age groups. The level of control increased with age after 75 years, which implies a greater level of AHT control in older patients. These findings may have been influenced by the greater prevalence of target organ damage and associated CVD in the study population, especially heart failure and coronary disease, which are clinical conditions that require more intense treatment. In the case of heart failure, the type of ventricular dysfunction (systolic or diastolic), which was not analyzed in this study, could have had an impact on the differences in BP between groups. Also, older patients had been treated for a longer period of time with combined treatment of antihypertensive drugs.
The level of AHT control among diabetic women continues to be low, and similar to rates described in other studies12, 23 that have considered “good control” in this population to be BP levels <130/80mmHg. Although our study design did not allow for establishing which variables are associated with poor control, we did observe that the most strongly related factors were more recent AHT, poor lipid control, poor HbA1c control, background of CVD, monotherapy treatment, and abdominal obesity, which are well-known factors for poor control.15, 19, 21, 22
The majority of patients received combined drug treatments (67.6%), a similar percentage to that observed in other studies with elderly patients,25, 26, 34, 35 with no significant differences in the use of 2 or more antihypertensive drugs between controlled and uncontrolled patients. This finding has been described previously,32 and could be due to the difficulty in controlling AHT in advanced stages of the disease or due to poor compliance with treatment schedules, which is a very common factor in chronic and asymptomatic diseases such as AHT.
Upon analyzing the treatment subgroups of women included in the MERICAP study, the most commonly used drugs were diuretics, followed by ARB-II and ACE inhibitors, which also are in concordance with other studies28, 34, 36 and the recommendations from some guidelines37 that advise the use of thiazide diuretics as the first step of treatment, whether as monotherapy or in combined treatment. On the other hand, the high prevalence of heart failure may have had an impact on the recommended treatment schedule.
LimitationsThe limitations of this study are the same as for any observational study; it does not allow for the randomization of patients and doctors and thus cannot establish a cause-effect relationship between the correlations observed. Furthermore, we measured some variables only once (weight, height, abdominal circumference) or several times but on the same visit (BP), using the available techniques (not validated for all researchers). The laboratory analyses were not all carried out at the same place, and we did not evaluate noncompliance with treatment schedules as a cause of poor control. The high prevalence of HF, which was higher than that for ischemic heart disease, could have been due to a selection bias based on the primary objective of the study (the detection of hidden heart failure in hypertensive patients). Although these limitations do not allow for general conclusions based strictly on the results from the female population in Spain aged 65 years or older, we do believe that the large sample size, the consecutive selection of a maximum of 5 patients per doctor, and the methods of analysis used all provide robustness to the study, and that our results could be reasonably considered as representative of hypertensive women being treated in the PC setting.
CONCLUSIONSThe results from the MERICAP study, involving only female patients, showed that only 3 in 10 hypertensive patients ≥65 years old and treated in the PC setting have optimally controlled AHT. Patients with uncontrolled BP had greater percentages of CVRF, target organ damage, and associated CVD than patients with good BP control. A younger age of the AHT condition, LDL >115mg/dl, and HbA1c ≥7% were the most highly correlated variables for poor control.
CONFLICTS OF INTERESTThis study was carried out using an unconditional research grant from Laboratorios Almirall S.A.
Acknowledgements
We would like to thank all PC doctors that participated in the MERICAP study for their collaboration and for providing the data necessary for this project.
Received 24 November 2010
Accepted 29 April 2011
Corresponding author: Tallafoc del Ferro 11, 46012 Valencia, Spain. jllisterric@gmail.com