To the Editor,
Aortobronchial fistula (ABF) is a rare, late, and usually catastrophic complication that should be suspected in any patient who has undergone a surgical procedure involving descending thoracic aorta. It usually presents as atypical chest pain that is followed by massive hemoptysis and death due to blood loss if emergency surgery is not performed.
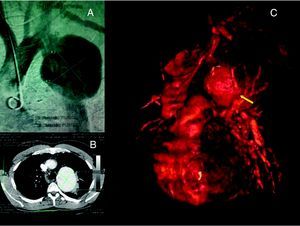
Our patient was a 39-year-old man, whose only notable medical event had been surgical repair of aortic coarctation with patch enlargement 27years earlier and who, after several days of intense atypical chest pain, came to our center because his condition had deteriorated and he had developed hemoptysis, with a loss of over 600mL of blood. Given his history of previous aortic surgery with no other risk factors, emergency contrast-enhanced computed tomographic angiography (CTA) was requested. This study revealed a true aneurysm measuring 71mm×71mm in diameter, located 11mm distal to the orifice of left subclavian artery, confirmed by aortography (Figure 1); thus, the decision was made to perform an emergency endovascular surgical intervention.
Figure 1. Preoperative images. A: aortography indicating 71-mm aneurysm. B: computed tomographic angiography of descending aorta. C: 3-dimensional reconstruction; the arrow indicates the site of the aortobronchial fistula, with a bronchiole eroded by the aneurysm and alveolar hemorrhage.
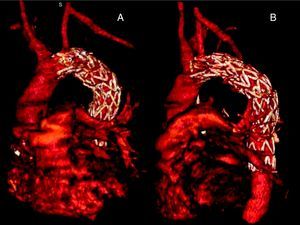
After dissection of left common femoral artery, a Medtronic Valiant thoracic aortic endograft (Medtronic, Santa Monica, California, United States) measuring 26mm×26mm×150mm was implanted distal to the orifice of left subclavian artery, excluding the aneurysm. On the third day after the operation, the patient underwent a follow-up CTA, which revealed a proximal type IA endoleak. The decision was made to reintervene to perform a left carotid-subclavian bypass to occlude the ostium of the left subclavian artery and improve the seal and, in addition, to implant a new 28mm×28mm×100mm Medtronic Valiant endograft; the absence of endoleaks was confirmed by follow-up CTA 72h later (Figure 2). To complete the treatment, maintenance antibiotic therapy with levofloxacin was administered for 6 months. One year later, the patient is asymptomatic.
Figure 2. Postoperative images. Note the left carotid-subclavian bypass. A: frontal view. B: lateral view.
Postoperative ABF is a rare and serious late complication of surgical interventions involving the thoracic aorta. It is potentially fatal and can occur as early as 3weeks and as late as 25years after the primary surgery.1 The existence of a certain index of suspicion is fundamental for diagnosis, given the lack of specificity of the standard diagnostic tests.2, 3 The chest X-ray is generally normal or provides inconclusive images. High-resolution CTA and aortography usually identify the aneurysm or pseudoaneurysm, but they commonly fail to discover the fistula. Fiberoptic bronchoscopy should be carried out to attempt to identify the site of the communication.4
At the present time, the majority of the cases of ABF are related to penetrating ulcers or complications of interventions to treat congenital aortic disease.3, 4 One of every 6 patients will have a pseudoaneurysm or aneurysmal degeneration as a complication of surgery of this type.4 In addition to hemoptysis, chest pain and dyspnea usually appear in up to 45% of the cases.3, 5
The treatment is always surgical, even when the diagnosis remains unconfirmed; at present, the technique of choice involves the endovascular approach.4, 5, 6 However, the indication for long-term antibiotic therapy remains a subject of controversy.6 The use of these endovascular techniques has enabled surgeons to achieve a success rate of over 90%, with excellent medium-term results, considerably reducing the rates of morbidity and mortality associated with conventional surgery (from 15-41% to 6.6%6).
In short, endovascular treatment is a safe therapeutic alternative for the repair of an ABF, although long-term follow-up is necessary.
Without treatment, this condition is associated with a mortality rate of 100% and, thus, clinical suspicion is essential for immediate action to be undertaken. In our case, the time elapsed between surgery and the development of the ABF was 27years, making this the case with the latest onset reported in the literature.
Corresponding author: erodriguezcaulo@hotmail.com