To the Editor,
A 26-year-old man came to our hospital for paroxysmal palpitations accompanied by profuse sweating, dry heaves, and considerable psychomotor agitation unrelated to effort (sudden onset during physiological sleep). He was transferred to the recovery unit for assessment and symptom management.
During the patient's stay in the unit, his overall condition deteriorated unexpectedly, ventricular tachycardia caused by torsade de pointes appeared simultaneously on the electrocardiographic monitor (lead II), and he experienced cardiopulmonary arrest. He recovered following cardiac electric defibrillation (3 shocks of 200, 200, and 360 J of energy, respectively) and pharmacological treatment (2 g of sulfate magnesium in a bolus over 2 min, followed by prescribed intravenous perfusion of 500 mL of saline solution with 2 mg of sulfate magnesium, together with 1.5 µg of isoproterenol/min). He recovered completely, and there were no changes compared to the baseline QTc value. The patient had experienced another ventricular fibrillation episode 3 years earlier, from which he recovered by electric defibrillation in another hospital.
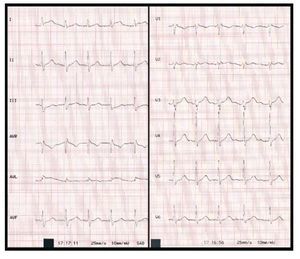
The ECG prior to the ventricular tachycardia presented electrical abnormalities with a short PR interval and long QT interval. This ECG pattern remained stable throughout the patient's follow-up, and was not a finding on admission (Figure 1).
Figure 1. Baseline 12-lead surface electrocardiogram for the patient.
Once the event stabilized, the patient was transferred from the emergency room to the cardiology department, where he underwent an electrocardiographic study and a series of protocol-based tests for similar lesions: laboratory workup (basic, ions, electrolytes, thyroid, cardiac), Holter monitoring, stress test, echocardiography, tilt test, and single photon emission computed tomography. None of these examinations showed significant cardiac alterations. Genetic and electrophysiologic studies were also carried out. The genetic studies showed no abnormalities in genes currently considered to cause short PR interval1 (PRKAG2) or in specific genes known to cause long QT interval2 (LQT1 [KCNQ1], LQT2 [HERG + MiRP1], LQT3 [SCN5A], and LQT4 [anchor protein Ankyrin B]).
In the electrophysiologic study, after autonomic blockade with esmolol and subsequent pacing with adenosine, no specific cardiac arrhythmia (including ventricular fibrillation) was induced, and the mean intervals were AH 40 ms, His 25 ms, HV 25 ms, and normal AV conduction with 1:1 AV conduction up to 714 ms and absence of VA conduction.
The patient's family history included 2 sudden deaths—father and paternal uncle at 47 and 34 years of age, respectively—classified as of uncertain origin because no cardiac or noncardiac organic abnormalities (structurally normal heart) were observed in the autopsies; neither person had ever reported symptoms that might have suggested a heart condition.
The patient's current close and immediate family consisted of his mother, age 48, a 25-year-old sister (Figure 2), and 2 nephews, aged 2 and 3 years.
Figure 2. Baseline 12-lead surface electrocardiogram for the patient's sister.
The mother's baseline surface electrocardiogram presented an image of right incomplete bundle-branch block, with no other abnormalities of interest; she reported no unusual cardiac symptoms to date. The sister had a baseline electrocardiogram that resembled the patient's (short PR interval, averaging 0.09 s and long QT interval, averaging 0.475 s) and also reported no unusual cardiac symptoms to date. The baseline electrocardiograms for the nephews were within normal for their age and sex.
In the patient's ECG, the mean PR interval was 0.096 s, the mean QT interval was 0.52 s, and the mean QTc was 0.555 s (Bazett), 0.543 s (Fridericia), and 0.584 s (Framingham). These values revealed the presence of electrocardiographic abnormalities unknown to date (Figures 1 and 2): short PR interval1 along with long QT interval2 in an individual who had experienced 2 cardiopulmonary arrests from which he recovered (one in our hospital).
The combination of a short PR interval and a long QT interval in this patient may be incidental. Nevertheless, the extremely short PR interval and the fact that his sister shows the same electrocardiographic findings suggest that, unless future publications report similar findings or genotyping, this combination may be genetically conditioned and may represent a new variant of long QT syndrome.