There is continued debate about the routine use of aspiration thrombectomy in patients with ST-segment elevation myocardial infarction. Our aim was to evaluate clinical and procedural outcomes of aspiration thrombectomy-assisted primary percutaneous coronary intervention compared with conventional primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction.
MethodsWe performed a meta-analysis of 26 randomized controlled trials with a total of 11 943 patients. Clinical outcomes were extracted up to maximum follow-up and random effect models were used to assess differences in outcomes.
ResultsWe observed no difference in the risk of all-cause death (pooled risk ratio = 0.88; 95% confidence interval, 0.74-1.04; P = .124), reinfarction (pooled risk ratio = 0.85; 95% confidence interval, 0.67-1.08; P = .176), target vessel revascularization (pooled risk ratio = 0.86; 95% confidence interval, 0.73-1.00; P = .052), or definite stent thrombosis (pooled risk ratio = 0.76; 95% confidence interval, 0.49-1.16; P = .202) between the 2 groups at a mean weighted follow-up time of 10.4 months. There were significant reductions in failure to reach Thrombolysis In Myocardial Infarction 3 flow (pooled risk ratio = 0.70; 95% confidence interval, 0.60-0.81; P < .001) or myocardial blush grade 3 (pooled risk ratio = 0.76; 95% confidence interval, 0.65-0.89; P = .001), incomplete ST-segment resolution (pooled risk ratio = 0.72; 95% confidence interval, 0.62-0.84; P < .001), and evidence of distal embolization (pooled risk ratio = 0.61; 95% confidence interval, 0.46-0.81; P = .001) with aspiration thrombectomy but estimates were heterogeneous between trials.
ConclusionsAmong unselected patients with ST-segment elevation myocardial infarction, aspiration thrombectomy-assisted primary percutaneous coronary intervention does not improve clinical outcomes, despite improved epicardial and myocardial parameters of reperfusion.
Full English text available from:www.revespcardiol.org/en
Keywords
Primary percutaneous coronary intervention (PPCI) is the standard of care for patients with ST-segment elevation myocardial infarction (STEMI).1,2 Compared with fibrinolysis, PPCI is associated with improved patency of the infarct-related artery, a lower risk of reocclusion and reinfarction, faster and more complete resolution of ST-segment elevation, and improved epicardial (Thrombolysis In Myocardial Infarction [TIMI] flow 3) and myocardial reperfusion myocardial blush grade [MBG] 3).3 In aggregate, these benefits translate into reduced infarct size and improved survival.4
Nevertheless, up to one-fourth of reperfused coronary arteries show evidence of impaired flow at the myocardial level (MBG < 2) after PPCI,5 commonly referred to as no-reflow phenomenon and associated with increased infarct size and reduced survival.6 Among several causes, embolization of thrombotic material and plaque debris into the microcirculation during stent implantation is an important putative mechanism of reperfusion injury,7 which has led to the development of dedicated devices to further improve on results.8
Although distal protection devices failed to improve epicardial and myocardial reperfusion or infarct size, aspiration thrombectomy (AT) has yielded some positive results.9 The procedure is technically simple, not time demanding, and can be easily performed in nearly all anatomies.10 Several studies and systematic reviews have reported improved parameters of reperfusion following AT.10–14 However, a survival benefit has not been consistently observed.8,15–17 In view of the recently reported 1-year outcomes of the large-scale Thrombus Aspiration in ST-Elevation myocardial infarction in Scandinavia (TASTE) trial, we performed a meta-analysis to assess the clinical value of AT in the management of STEMI.
METHODSSearch StrategyWe searched MEDLINE and EMBASE through OvidSp, PubMed, and the Cochrane Central Register of Controlled Trials (CENTRAL) with a combination of words and keywords related to “thrombectomy,” “thrombus,” and “myocardial infarction,” with no restrictions for language. Published meta-analyses and reference lists of the finally eligible trials were reviewed. We provided our list of identified randomized clinical trials to experts in the field with a request to provide us citations to randomized clinical trials not yet identified. The searches were performed on September 5, 2014 (Tables 1 and 2 of the supplementary material).
Eligibility CriteriaIncluded trials met the following criteria: a) investigated AT-assisted PPCI in the setting of STEMI, and b) patients were randomly allocated to PPCI with or without AT within 24hours of symptom onset. Aspiration thrombectomy included all manual thrombectomy devices and vacuum aspiration devices. Trials that randomized rescue PCI patients were included, but not those that tested facilitated PCI with fibrinolysis. We excluded studies not providing any prespecified outcome, studies using mechanical thrombectomy devices, studies of thrombectomy in saphenous vein grafts, those comparing different thrombectomy devices with each other, and combined strategies (ie, with additional antithrombotic therapy or protection devices). Two investigators (Ernest Spitzer and Stefan Stortecky) independently performed the screening, reviewed articles, and determined their eligibility through the web-based software EROS (Early Review Organizing Software). Discrepancies were resolved by consensus.
Data Extraction and Pre-specified OutcomesWe extracted characteristics of trials, patients and interventions, including study design, length of follow-up, details on methodological quality, source of funding, time of randomization, age, sex, diabetes, ischemic time (Table 3 of the supplementary material), use of enteral and parenteral antithrombotic agents, multivessel disease, myocardial infarction involving the left anterior descending artery territory, and visualization of thrombus as a prerequisite prior to randomization.
Procedural outcomes extracted included a surrogate marker of epicardial reperfusion, namely failure to reach TIMI flow grade 318; 2 surrogate markers of myocardial reperfusion, namely failure to reach MBG grade 3,19 and incomplete ST-segment elevation resolution (iSTR, resolution of < 70% of the sum of the initial ST-segment elevation)20; as well as absence of direct stenting,21 and evidence of distal embolization.7
Prespecified clinical endpoints included all-cause death, reinfarction, target vessel revascularization, definite stent thrombosis, and stroke. Data on all-cause death was not available in 8 trials; in 5 of these trials cardiac death was used as a proxy measure. Reinfarction included Q-wave and nonQ-wave myocardial infarction as defined in each study. Target vessel revascularization was defined as repeat percutaneous intervention or coronary artery bypass grafting of the target vessel or its branches. If target vessel revascularization was not reported, target lesion revascularization was used as a proxy measure. Definite stent thrombosis was defined as a thrombosis within the stented segment, confirmed by angiography or pathology in accordance with the criteria of the Academic Research Consortium.22 The number of patients experiencing an adverse event and the overall number of patients at risk were recorded separately. For all trials, 1-month and longest available follow-up results were used. Data were extracted independently by 2 authors (Ernest Spitzer and Giulio G. Stefanini), and discrepancies were resolved by consensus.
Quality AssessmentMethodological quality was assessed by extracting information on concealment of allocation, blinding of investigators adjudicating clinical events, the independence of investigators assessing angiographic and electrocardiographic endpoints, and the inclusion of all randomized individuals into the analysis according to the intention-to-treat principle.23 Concealment of allocation was considered adequate if the investigators responsible for patient selection did not know before allocation which treatment was next in line. The analysis was considered to be according to the intention-to-treat principle if all randomized patients were analyzed in the group they were originally allocated to, regardless of the treatment actually received.
Statistical AnalysisWe calculated risk ratios from the number of patients per arm with adverse events (and in the denominator the number of patients randomized per arm for clinical outcomes and number of patients analyzed per arm for procedural outcomes) as measures of treatment effect and used a DerSimonian and Laird random effects models to combine estimates across trials. We performed overall meta-analyses for all clinical outcomes using the maximum follow-up duration available for each trial. We also analyzed the procedural outcomes reported, but excluded EXPORT and Lelek et al from the STR analysis, because both reported STR > 50% as complete and was not comparable to the other trials. We excluded the Thrombus Aspiration during Percutaneous Coronary Intervention in Acute Myocardial Infarction Study (TAPAS) and the Polish-Italian-Hungarian Randomized ThrombEctomy Trial (PIHRATE) from the direct stenting analysis, because control groups were randomized to balloon predilatation. We determined heterogeneity across trials using the I2 statistic, constructed funnel plots to assess asymmetry, and used Egger's test for small study effects. We performed stratified analyses for all outcomes by the following trial characteristics: adequate concealment of allocation, blind adjudication of clinical outcomes, or independent assessment of procedural outcomes, adequacy of analyses in accordance with the intention-to-treat principle, trial size, single-center vs multicenter study, industry-dependent funding, and year of publication (2010-2014 vs earlier). Interaction was tested for clinical outcomes at ≤ 30 days and ≥ 1 year follow-up when available. Sensitivity analyses according to the following criteria were executed: excluding trials that used vacuum aspiration devices, excluding TASTE, and excluding TASTE and TAPAS trials. An intention-to-treat analysis was used for all clinical outcomes.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was followed for this meta-analysis. All P-values were 2-tailed, with statistical significance set at .05, and 95% confidence intervals (95%CI) were calculated. All analyses were performed using Stata 13 (Stata Corporation; College Station, Texas, United States).
RESULTSWe identified 831references and considered 87 to be potentially eligible (Figure 1 of the supplementary material). Thirty-eight reports describing 26 trials met our inclusion criteria and were included in the meta-analysis, 13 abstracts and 25 full-text articles (Table 3 of the supplementary material). The trials had randomly allocated 11 943 patients undergoing PPCI in the setting of STEMI to adjunctive treatment with AT (n = 5969) or PPCI alone (n = 5974). Twenty trials allocated patients to manual AT devices including Diver (Invatec; Brescia, Italy) (4 with 531 patients), Pronto (Vascular Solutions; Minneapolis, Minnesota, United States) (1 with 148 patients), Export (Medtronic; Minneapolis, Minnesota, United States) (11 with 2557 patients), Eliminate (Terumo Clinical Supply; Gifu, Japan) (2 with 269 patients), and Thrombuster II (Kaneka Medical Products; Osaka, Japan) (1 with 86 patients). One trial did not report the manual catheter used (71 patients). Four trials allocated patients to vacuum-pump assisted AT including TVAC (Nipro; Osaka, Japan) (1 with 355 patients) and Rescue (BSC; Maple Grove, Minnesota, United States) (3 with 545 patients). Two trials combined catheters, 1 used Diver and Rescue in 137 patients, and another Eliminate, Export and Pronto in 7244 patients. Seven trials with 691 patients required thrombus evidence for randomization.
Baseline clinical, angiographic, and procedural characteristics are summarized in the Table 3 of the supplementary material. Methodological characteristics of included randomized clinical trials are summarized in the Table 4 of the supplementary material. Concealment of allocation was adequate in seven trials and not reported in 19 trials. Blind adjudication of clinical events by an independent clinical events committee was described in 2 trials, independent assessment of angiographic outcomes in 6 trials, and independent assessment of electrocardiographic endpoints in 4 trials. Seventeen trials had analyzed data according to the intention-to-treat principle. The maximum length of follow-up ranged from in-hospital to 2 years with a follow-up duration of more than 1 month in 15 trials. Eight trials reported the funding received to be independent from industry.
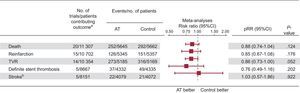
Clinical OutcomesPooled risk ratios (pRR) of random effects meta-analyses are shown in Figure 1. At a weighted maximum follow-up duration of 10.4 months, there was no significant difference in the risk of all-cause death (pRR = 0.88; 95%CI, 0.74-1.04; P = .124), reinfarction (pRR = 0.85; 95%CI 0.67-1.08; P = .176), target vessel revascularization (pRR = 0.86, 95%CI, 0.73-1.00; P = .052) or definite ST (pRR = 0.76; 95%CI, 0.49-1.16; P = .202) between groups. The risk of stroke was similar for both groups, but confidence intervals were wide (pRR = 1.03; 95%CI, 0.57-1.86; P = .922).
Meta-analysis of clinical outcomes at maximum follow-up. 95%CI, 95% confidence interval; AT, aspiration thrombectomy; pRR, pooled risk ratios of random effects meta-analysis; TVR, target-vessel revascularization. I2 = 0 in each of the 5 meta-analyses. aNote that trials with zero events in both arms were excluded from meta-analyses. bAll strokes were reported within the first 30 days of follow-up.
We observed no evidence of heterogeneity across trials for any of the analyzed endpoints (I2 = 0% for all endpoints) (Figure 2 of the supplementary material). Funnel plots did not suggest small study effects and stratified analyses showed no evidence for interactions for treatment effects with trial characteristics on any of the clinical outcomes, except for statistical trends suggesting beneficial effects of AT assisted PPCI in single-centre trials for all-cause death and reinfarction. A similar trend suggesting beneficial effects for all-cause death was observed in early trials (Figure 3 and Table 5 of the supplementary material). Stratified analyses comparing short-term vs long-term outcomes showed no significant interactions (Figure 2). Results of sensitivity analyses are summarized in Table 6 of the supplementary material and indicate that findings were consistent after exclusion of trials using vacuum aspiration devices.
Meta-analysis of clinical outcomes stratified for follow-up time. 95%CI, 95% confidence interval; AT, aspiration thrombectomy; pRR, pooled risk ratios of random effects meta-analysis; TVR, target-vessel revascularization. All strokes were reported within the first 30 days of follow-up, so no stratification was performed. *Excludes trials with zero events in both arms.
Pooled risk ratios of random effects meta-analyses for procedural outcomes are shown in Figure 3. The use of AT was associated with a significant reduction of postprocedural TIMI flow < 3 (pRR = 0.70; 95%CI, 0.60-0.81; P < .001), MBG < 3 (pRR = 0.76; 95%CI, 0.65-0.89; P = .001), and iSTR (pRR = 0.72; 95%CI, 0.62-0.84; P < .001). Aspiration thrombectomy was also associated with a lower frequency of absence of direct stenting (0.42, 95%CI, 0.30-0.57, P < .001) and distal embolization (pRR = 0.61; 95%CI, 0.46-0.81; P = .001) compared with PPCI alone (Figure 4 of the supplementary material).
Meta-analysis of procedural outcomes. 95%CI, 95% confidence interval; AT, aspiration thrombectomy; MBG, myocardial blush grade; pRR, pooled risk ratios of random effects meta-analysis; STR, ST-segment elevation resolution; TIMI, Thrombolysis In Myocardial Infarction. Note that trials with zero events in both arms were excluded from meta-analyses. *See “Methods” for description of trials excluded from incomplete ST-segment elevation resolution and no direct stenting analyses.
Heterogeneity between trials was low for postprocedural TIMI flow < 3 (I2 = 0%) and distal embolization (I2 = 12.3%). However, there was evidence of high heterogeneity for MBG < 3 (I2 = 73.3%), iSTR (I2 = 74.4%), and absence of direct stenting (I2 = 92%). Funnel plots revealed higher benefits of AT in smaller trials for iSTR and absence of direct stenting, with positive Egger's test for asymmetry (Figure 5 of the supplementary material). In stratified analyses we generally found trials with adequate concealment of allocation to show smaller benefits on procedural outcomes, with formally positive interactions for iSTR, and absence of direct stenting (both P < .003); and a statistical trend for TIMI < 3 (P = .07). There were also positive interactions with independent assessment of outcomes for iSTR (P < .001); with sample size for iSTR and absence of direct stenting (both P < .01); with single vs multicentre design for iSTR, and absence of direct stenting (both P < .002); and with year of publication for iSTR (P < .001). In general, trials showed less benefit on procedural outcomes if they were more recent, of higher quality and with larger sample size (Table 7 of the supplementary material). Stratification according to the selective use of AT based on thrombus evidence at baseline did not reveal a significant interaction. Notably, less than 6% of patients were treated selectively and with nonuniform criteria (Table 8 and Figure 6 of the supplementary material).
DISCUSSIONThe findings of this meta-analysis of 26 randomized trials in 11 943 patients and a weighted maximum follow-up duration of 10.4 months in the setting of PPCI for STEMI with or without adjunctive AT can be summarized as follows:
- •
The use of adjunctive AT in unselected STEMI patients in the setting of PPCI does not significantly reduce all-cause mortality, reinfarction, target-vessel revascularization, or definite stent thrombosis.
- •
Although AT results in improved parameters of epicardial and myocardial reperfusion, there is evidence of bias and more recent trials, those of higher quality, and larger sample size show smaller improvements than the remainder.
- •
The risk of stroke is not affected by the use of AT.
Direct aspiration of thrombotic material in the setting of STEMI by means of AT devices is a simple procedure which attempts to reduce thrombus burden with the aim of improving procedural and clinical outcomes in STEMI patients. On the basis of encouraging findings from relatively small trials, the use of AT has been rapidly implemented in clinical practice. Nevertheless, a beneficial effect of AT on ischemic clinical outcomes has not been shown by adequately powered randomized clinical trials. Recently the TASTE trial failed to show the superiority of AT compared with conventional PPCI with respect to the primary endpoint of all-cause death at 30 days and 1-year in unselected STEMI patients.24,25 In the present meta-analysis we summarized all the available randomized evidence providing the largest collective evidence base on AT so far.
Contrary to several previous meta-analyses, our results indicate no benefit in clinical outcomes at the time of longest follow-up.11,13,15,16,26 It has recently been suggested that even though a benefit was not observed at short-term follow-up, late mortality may be reduced by AT.26 This prompted the question of whether the equipoise in early mortality was related to a lack of statistical precision or whether there was an actual mechanistic explanation for a potential reduction in late mortality. In a stratified analysis we found no formal interactions for the time point of evaluation of outcomes (30 days or 1 year). These results were largely influenced by the TASTE trial, since after its exclusion the results were consistent with previous meta-analyses in the sensitivity analysis. Nevertheless, we explored pooled estimates after exclusion of the TASTE and TAPAS trials, and again no benefit was observed in favour of AT.
Several reports suggest that the unrestrictive use of thrombectomy may not offer a benefit to all STEMI patients.27–30 Even in the case of effective thrombectomy, other determinants of prognosis including ischemic time, extent of the area at risk, presence of collateral flow before the procedure, and quality of reperfusion at the end of the procedure, as well as stent type, need to be considered.31–33 The interplay between these factors may importantly diminish the impact of AT on overall mortality in unselected STEMI patients. Of note, at least 35% of patients included in the TASTE trial did not present with an angiographically-evident thrombus (TIMI thrombus grade > 1) camouflaging potential benefits among patients with large thrombus burden.
Kumbhani et al26 showed a significant reduction of reinfarction and stent thrombosis during a weighted mean duration of follow-up of 2.7 months. Our results at 10.4 months showed no difference in the 2 endpoints between groups; however, after stratifying the extracted outcomes according to short- (30 days) or long-term (1 year) follow-up, we observed significantly lower rates of reinfarction at 30 days, a benefit that subsequently disappeared at 1 year. This finding was due to a numerically lower incidence of reinfarction at 1 month observed in patients randomized to AT in the TAPAS and TASTE trials.24,25,34 Nevertheless, TASTE results at 1 year showed virtually no difference among arms (2.7% vs 2.7%, hazard ratio [HR] 0.97; 95%CI, 0.73-1.28; P = .81).
Immediate effects of AT on reperfusion have been consistently demonstrated in randomized trials and previous meta-analyses, revealing improved postprocedural TIMI flow and MBG. Our results confirm a significant improvement with respect to both epicardial and myocardial perfusion among patients treated with AT. However, asymmetrical funnel plots and stratified analyses suggest that previous meta-analyses may have overestimated the benefit if they disregarded methodological quality and sample size as potential explanations of heterogeneity between trials. Stratifying by year of publication also revealed a significant interaction for a marker of myocardial reperfusion (ie, iSTR), which could be a consequence of patient selection, improved periprocedural treatments (ie, antithrombotic regimens) or, again, methodological quality. Nevertheless, in view of the low extent of heterogeneity and negative interaction tests, overall estimates appear valid for TIMI flow < 3, MBG < 3, and distal embolization. Conversely, absence of direct stenting, and iSTR should be interpreted cautiously.
In a recent meta-analysis of AT in STEMI patients,14 a trend has been reported toward a higher risk of stroke at the expense of AT. However, the analysis was limited at least in part by the inconsistent reporting of stroke across included trials, as well as by the low number of patients included for the calculation of estimates. In the present meta-analysis, no differences in the risk of stroke were observed between patients treated with or without AT, suggesting the absence of safety concerns related to AT and the risk of cerebrovascular events.
LimitationsThe findings of the present meta-analysis should be interpreted in view of the following limitations. First, in the absence of individual patient data, findings should be viewed as average effects, and differential effect size in specific subgroups cannot be excluded. Second, we were unable to analyze data on the impact of AT on infarct size due to its inconsistent reporting in included trials. Third, procedural outcomes suffered from heterogeneity, small study effects, and stratified analysis showed evidence for less benefit of higher methodological quality. However, pRR for clinical endpoints showed no heterogeneity across trials and were not associated with trial size or quality, supporting the robustness of our findings for clinical outcomes. Fourth, our analysis is limited to a weighted mean follow-up time of 10.4 months, and longer-term benefits cannot be excluded. Finally, the upcoming results of A Randomized Trial of Routine Aspiration ThrOmbecTomy With PCI Versus PCI ALone in Patients With STEMI Undergoing Primary PCI (TOTAL) (NCT01149044) will shed more light on the effects of AT among STEMI patients undergoing PPCI, along with a planned patient-level meta-analysis combining TASTE and TOTAL data.
CONCLUSIONSAmong unselected patients with STEMI, AT-assisted PPCI does not improve clinical outcomes, despite improved epicardial and myocardial parameters of reperfusion.
FUNDINGFunding for the current analysis was provided in part by a grant of the Swiss National Science Foundation to Prof. S. Windecker and Prof. P. Jüni (grant 33CM30-140336). Dr. E. Spitzer is the recipient of a research fellowship of the EAPCI (European Association of Percutaneous Cardiovascular Interventions) of the European Society of Cardiology and a Research Grant of the Spanish Society of Cardiology. Dr. G. G. Stefanini is the recipient of a research fellowship (SPUM [Special Programme University Medicine]) of the Swiss National Science Foundation.
CONFLICTS OF INTERESTProf. P. Jüni an unpaid steering committee or statistical executive committee member of trials funded by Abbott Vascular, Biosensors, Medtronic and Johnson & Johnson. The CTU (Clinical Trials Unit) Bern, from the University of Bern, has a staff policy of not accepting honoraria or consultancy fees. However, CTU Bern is involved in design, conduct, or analysis of clinical studies funded by Abbott Vascular, Ablynx, Amgen, AstraZeneca, Biosensors, Biotronik, Boehringer Ingelheim, Eisai, Eli Lilly, Exelixis, Geron, Gilead Sciences, Nestlé, Novartis, Novo Nordisk, Padma, Roche, Schering-Plough, St. Jude Medical, and Swiss Cardio Technologies. Prof. S. Windecker has received research contracts to the institution from Biotronik and St Jude. All other authors have reported that they have no relationships to disclose.
We would like to thank Jingying Wang, a PhD student at the Institute of Social and Preventive Medicine, Bern, for her help in translating the Chinese manuscript into English.