To the Editor,
Penetrating aortic ulcers (PAU), aortic dissection (AD), and intramural hematomas (IH) constitute what is currently known as acute aortic syndrome. This condition carries a high rate of morbidity, meaning that an early diagnosis is necessary to start treatment quickly.1 After reading the interesting article by Gutierrez-Martín et al,2 we present the case of a penetrating aortic ulcer which fistulizes to the oesophagus. We did not have time to insert a vascular endoprosthesis as the patient died due to massive haematemesis. We would therefore like to point out the importance of recognizing this fatal complication.
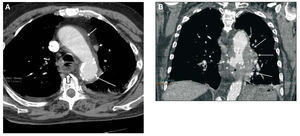
An 83-year-old male with a background of arterial hypertension, dyslipidemia, and a permanent pacemaker implanted 3 years earlier for symptoms of panconductional defect, had been diagnosed 1 year earlier with prostate carcinoma, which was stage IV with bone metastases at the time of consultation. The patient sought attention for retrosternal chest pain that radiated to the back over 4 days, and a recent episode of hematemesis. Physical examination showed blood pressure of 160/90 mm Hg, heart rate of 110 bpm, and normal pulse in both legs. Electrocardiogram showed abnormalities only in relation to the pacemaker, and cardiac enzymes (creatine kinase, troponin) were normal. Suspecting acute aortic syndrome, we performed a computerized tomography (CT) of the chest (Figure), in which an aortic intramural hematoma was observed that extended from the aortic arch (Figure, A), associated with PAU with anfractuous borders, hemomediastinum, and air bubbles related to an aortoesophageal fistula (Figure, B). We performed an endoscopy, in which a 4 cm ulcerated lesion, covered with normal mucosa and broad coagulation, without active bleeding, and compatible with an aortoesophageal fistula, was observed. The treatment plan involved placing an endovascular prosthesis but the patient died due to massive hematemesis before we could proceed.
Figure. Chest computerized tomography. A: axial: aortic intramural haematoma (short arrow) identified by the intimal calcification (long arrow), persistent in the upper left vena cava (arrow point), and submucosal haematoma in the posterior wall of the oesophagus (hollow arrow). B: coronal reconstruction: hyperdense saccular image projecting from the right margin of the aortic wall corresponding to a penetrating aortic ulcer, extravasation of the contrast due to perforation (short arrow), increased paraaortic density in relation to the haemomediastinum (long arrows), and small hypodensities inside the haemomediastinum caused by air bubbles (arrow points).
Originally described by Stanson in 1986,3 is currently considered to be a condition different from aortic dissection. It is defined as the ulceration of an aortic atheromatous plaque that penetrates the internal elastic layer up to the medial layer, causing it to weaken and aneurysms to form, or even rupture, which occurs in as many as 40% of untreated cases. It is frequently accompanied by a haematoma inside the aortic wall. This condition affects hypertensive patients over 65 years of age with severe atherosclerosis. The ulceration is most frequently located in the thoracic descending aorta. The clinical presentation includes intense chest pain, and a differential diagnosis is required to distinguish this condition from acute coronary syndrome, AD, and IH. Diagnosis is performed using a multidetector CT, which shows that iodinated contrast media accumulated in the aortic wall in the shape of a "bag, shirt button, or crater," on a wall which is normally thickened due to the associated IH. Intimal calcification provides a means for differentiating between intramural haematoma (extraluminal) and aortic thrombi (intraluminal).4
Fistulization towards the stomach has been reported in other studies.5 In our case, the anfractuous border of the ulcer, the presence of air in the haemomediastinum, and submucosal haematoma of the posterior esophageal wall all pointed towards this diagnosis. Treatment is based on placing a vascular endoprosthesis to isolate the ulcer in the bloodstream and to reinforce the aortic wall.6,7