To the Editor:
A paraganglioma is a neuroendocrine tumour that originates from the neural crest cells,1 on generating the parasympathetic ganglia. The tumours (paragangliomas) from the chromaffin tissue (phaeochromocytomas) are the most common and at the same time as the catecholamines; their most common location is the adrenal medulla, although they can also be found on the carotid bodies2 or in the chest.3 Derivatives of the chemoreceptors (chemodectomas) are more infrequent and are usually located in the carotid glomus and the middle ear.4
A 58-year-old female was referred to us diagnosed with periaortic paraganglioma. After the incidental x-ray finding of a mediastinal mass, thoracoscopy was performed at another centre. As it was not conclusive, a transsternal thoracotomy was performed for biopsy. This tumour, very haemorrhagic given its great vascularisation, was a paraganglioma.
The endocrine study displayed no secretion whatsoever of catecholamines.
The magnetic resonance imaging confirmed that the tumour had grown 3 cm in 3 months and displayed a necrotic centre, sign of rapid growth, with a highly vascularised perimeter. The mass compressed the superior vena cava, right pulmonary artery, the roof of the left atrium, displacing it towards the ascending aorta.
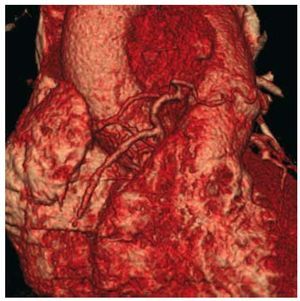
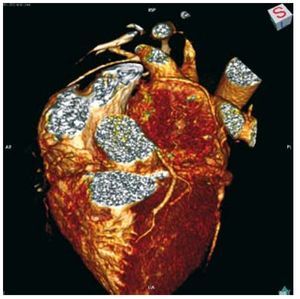
A computerised tomography (CT) was taken, which confirmed the description; clearly demonstrating how it displaced the common trunk from the left coronary artery, to which it was intimately attached. The reconstruction of the coronary tree was of even greater interest, from which 2 nourishing branches stemmed. The first, coming from the right coronary artery at 1 cm from the right ostium, evolved towards the tumour with an identical diameter to that of the right coronary artery (Figure 1). The second, originating in a marginal branch, progressed through the roof of the left atrium to irrigate the tumour (Figure 2). An exhaustive study of the tumour showed neovascularisation coming from the left bronchial artery and small branches from the aortic arch.
Figure 1. Computerised tomography with reconstruction of the right coronary tree and the Vieussens artery that irrigates the tumour.
Figure 2. Computerised tomography with reconstruction of the left coronary tree and the circumflex artery that irrigates the tumour on its posterior surface.
Given the history of haemorrhaging and in accordance with previous publications,5 we decided on prior embolisation of the tumour; 24 hours before the intervention the tumour was embolised with polyvinyl-alcohol microparticles measuring 355-500 µm. The 4 branches were catheterised: the tumoral branch of the right coronary artery, the branch coming from the circumflex coronary artery, the left bronchial artery, and the small branches originating in the aortic arch which also irrigated the tumour. A few hours after the procedure, the patient presented a sensation of nausea and discomfort, both self-limited and with no other symptoms.
On the following day, she was intervened via median re-sternotomy. Through cannulation of the aortic arch and bicaval drainage, the extracorporeal circulation was entered. The tumoral mass that displaced the superior cava vein was dissected and showed no infiltration (a perioperative biopsy was performed, results negative). More closely attached was the mass in the anterior surface of the common pulmonary artery and its right branch and the descending aorta on its back side. A subadventitial dissection allowed for total resection of the tumour, with respect to the sinus of Valsalva, the roof of the left atrium and roof of the common trunk. The previously embolised nourishing branches remained bloodless. The portion of the tumour related to the pulmonary artery was so closely attached that resection of the common pulmonary artery and right pulmonary branch for its extraction with the tumour was opted for.
To replace the pulmonary artery, it was resected at supravalvular level and at the height of both branches, and was replaced by a cryopreserved homograft. The ascending aorta was replaced above the sinotubular junction with a 28 mm Hemashield graft.
Pathological anatomy confirmed the cytology as compatible with paraganglioma.
Cardiac surgery is rarely confronted with cardiovascular tumours, outside of myxomas, valvular fibroelastomas, and some kidney tumours with venous invasion.
The paraganglioma, secretor (pheochromocytoma) or not, is very rare, it is usually not metastasised and its location makes resection complex.2,6 However, an exhaustive study of the tumour, with CT and reconstruction of its vascularisation, was crucial in the diagnosis and treatment of the case. In the diagnosis, given that it serves to differentiate it from other mediastinal tumours (lymphomas and sarcomas), on the other hand more common, and also the need for biopsies, in our opinion, contraindicated due to their high risk of haemorrhaging.7 With respect to its therapeutic importance, it would be crucial to locate all of the possible nourishing vessels for their embolisation,3 even if, as in this case, it involves the embolisation of coronary branches. Embolisation is not spurious, given the great tendency to bleeding of these tumours, as shown in this patient in the biopsy performed and as confirmed by other groups that did not opt for embolisation.8
The periaortic paraganglioma is a rare, highly vascularised tumour; its diagnosis should include an endocrine and vascularisation study. It is fundamental that its treatment includes embolisation of all nourishing arteries and a well planned aggressive surgical approach.