Keywords
INTRODUCTION
Coronary heart disease (CHD) is the leading cause of mortality in most industrialized countries.1 In Spain, it was the cause of 11.2% of deaths in males and 9.6% in females in 2004,2 although these rates vary considerably between countries.3,4 In southern European countries, mortality due to CHD and its incidence is between three to five times less than in northern countries, Spain having the second-lowest rates in Europe.3-6
In Spain, as in most western countries, mortality due to CHD has been decreasing since 1976,2,7,8 probably due to the effect of primary prevention regarding improvements in controlling cardiovascular risk factors. This decrease can also be attributed to secondary prevention in the patients who have already presented a coronary event, which includes optimizing the risk factor profile and treatments and therapeutic interventions that can modify the natural history of the disease. Improvements in the treatment of the patients in the acute phase of a coronary event, such as the increase in the use of drugs with proven efficacy, have also helped to maintain this trend.9-12 Primary prevention reduces the incidence of new coronary events, and secondary prevention, the number of recurrent events. In addition, improvements in treatment in the acute phase after a coronary event, such as acute myocardial infarction (AMI), would be associated with a decrease in the percentage of deaths among such patients. In order to study the influence of primary and secondary prevention on the evolution of case-fatality over time, and AMI incidence and mortality rates, the number of cases (fatal or not) of this disease in the population has to be calculated on an annual basis.13
The REGICOR project (Girona Heart Registry) has recorded all the patients with fatal and non-fatal AMI in the population of six counties in Girona since 1990.
The aim of this study was to analyze trends in AMI mortality, incidence, attack, and 28-day case-fatality rates between 1990 and 1999 in the population aged 35-74 years in Girona, and to analize trends in the use of therapies with proven efficacy in the acute phase of the patients hospitalized for myocardial infarction in the same period.
METHODS
The methodology used to identify and classify the cases has already been published.3,6 In short, a population of 227 598 inhabitants aged 35-74 years was monitored in six counties in Girona (1996 census). All AMI episodes in residents from the area were included in the registry: this was done prospectively, regarding those admitted to the only referral hospital in the area, and retrospectively regarding the nine regional hospitals. Furthermore, patients transferred to hospital centers from outside the area were identified. Patients who died without managing to contact the hospital system were identified by reviewing the mortality register, and all suspected cases of death due to CHD were investigated by interviewing the certifying physician and, if necessary, the family.14
Diagnostic and Selection Criteria
In order to be eligible, the subjects had to be clinically diagnosed with AMI or angina. Once identified, the patients were classified according to the MONICA (MONItoring of trends and determinants in CArdiovascular diseases) project algorithm,14 which takes into account the type of symptoms, electrocardiographic findings, enzymes and, for fatal cases only detected through the registry of mortality register, a previous history of CHD and the autopsy results, if carried out. According to this information, each case investigated was classified as: ischemic cardiac arrest successfully resuscitated, noncoronary death, definite AMI (fatal or non-fatal), possible AMI (fatal), and fatal case with insufficient data to classify it in one of the previous categories. The last four constitute definition 1 in the MONICA study, and are used to present the data in our study.14
Statistical Analysis
The following annual rates have been calculated: a) attack (or cumulative incidence): number of cases of AMI (first or recurrent) per 100 000 population; b) incidence: number of first AMI per 100 000 population; c) recurrence: number of cases of recurrent AMI per 100 000 population; d) hospitalization: number of AMI patients admitted to hospital alive per 100 000 population; e) mortality: fatal cases per 100 000 population; this mortality rate was also calculated depending on whether death occurred in or outside the hospital; f) case-fatality in the population: percentage of fatal cases in the first 28 days among all the patients with AMI in the region studied; and g) in-hospital case-fatality: percentage of fatal cases among the patients with AMI arriving at the hospitals alive. All the indicators were calculated separately for every year for the period studied.
The annual inter-census estimations -- calculated on the basis of the electoral censuses of 1991 and 1996 -- were used as denominators to calculate the annual rates. The rates, which were standardized using the direct method, are presented using the world population as the reference: 12, 11, 8, and 5 for the age groups 35-44, 45-54, 55-64, and 65-74 years, respectively.15 Case-fatality was standardized by calculating weights based on the standard distribution by patient age-group: 7, 16, 26, and 50 for the age groups 35-44, 45-54, 55-64, and 65-74, respectively.6,14
To analyze trends, log-linear models were used assuming a Poisson distribution.16,17 Aggregate data were analyzed and adjusted using the following general linear model:
ln(E[Me,t])=α0+αee+β1t+β2t2+γete+ηet2+ln(Pe,t)e,t
where t is the period, Me,t is the number of cases in age group e and period t, E[Me,t] is the number of cases expected in age group e and period t, α0 is the model constant, αe are coefficients of the age groups (e)m, β1 is the coefficient of the period (t), β2 is the coefficient of the quadratic term for the period, γe is the interaction between the age groups and the period, eηe is the interaction between the age groups and the quadratic term of the period, and ln(Pe,t)e,t is the natural logarithm of the risk population in age group e and period t. This term is equivalent to standardization by age.
The annual percentage change (APC) was estimated using the expression APC=(eβ1+γe1)x100. For the indicators where there is significant interaction between age groups and period, PCA was estimated using the expression APC=(eβ1+γe1)x100.
RESULTS
Between 1990 and 1999, 3951 eligible cases were recorded: 75.8% were classified as definite AMI and the remainder as possible AMI (fatal), or unclassifiable due to insufficient data (Table 1).
Table 2 presents the mean annual attack rate (first and recurrent) in the population aged 35-74 years between 1990 and 1999. The standardized mean annual incidence rate (first AMI only) was: 178 (95% confidence interval [CI], 170-185) per 100 000 males between 35-74 years and 39 (95% CI, 35-42) per 100 000 females. It could not be determined if there was a background of AMI in 14.1% of the cases. If the cases without information on a background of AMI were all incident cases, the standardized mean annual incidence rate would be 212 (95% CI, 203-220) per 100 000 males and 48 (95% CI, 44-51) per 100 000 females. Both approaches showed that the conclusions regarding the trends were similar.
On the other hand, the mean annual age-specific and age-standardized mortality rates are presented in Table 2. The standardized mean annual out-of-hospital mortality rate for the population between 35-74 years was 68 (95% CI, 63-72) and 16 (95% CI, 14-18) per 100 000 males and females, respectively. The standardized mean annual hospital mortality rates were 31 (95% CI, 28-34) and 9 (95% CI, 7-10) per 100 000 males and females, respectively.
Table 3 shows the distribution of mean case-fatality by age and by sex. The standardized population mean 28-day case-fatality rate in the age group between 35-74 years in the study period was 42.1% (95% CI, 41.5%-42.8%). The age-standardized hospital case-fatality rate in the period 1990-1999 was 20.0% (95% CI, 19.6%-20.5%). Both were significantly higher in females than in males (Table 3). Some 66.8% of the fatal episodes occurred without patients accessing specialized hospital care: 67.8% in males and 63.2% in females.
Trend Analysis
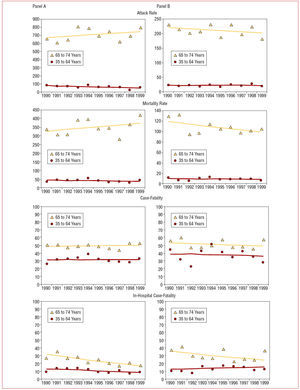
Models were adjusted to analyze the effect of the year of registry on the different rates, including age groups 35-44, 45-54, 55-64, and 65-74 years. A different trend was found in the age group 65-74 years compared to age groups 35-44, 45-54, and 55-64 years, which behaved similarly. This interaction between age group and year of registry was statistically significant in males for attack rates (P=.01) and recurrence (P=.04) and was marginally significant for mortality (P=.09) (Figure 1A). The interaction did not reach statistical significance in any of the indicators for females (Figure 1B). Table 4 presents the mean annual changes in the linear trend for different indicators for age groups 35-64 and 65-74 years in males. There was a statistically significant decrease in attack, incidence, recurrence, and hospitalization rates in males aged 35-64 years. There were no statistically significant annual changes in any of these in males aged 65-74 years. On the other hand, mortality rates remained stable in males in both age groups during the period studied. In-hospital case-fatality significantly decreased in males aged 65-74 years, whereas population case-fatality remained stable in both groups.
Figure 1. Evolution of attack and mortality rates per 100 000 population, and total and in-hospital case-fatality rates due to myocardial infarction for two age groups in males (A) and females (B) with their linear trends. Definite infarction, fatal or non-fatal, possible fatal or those with insufficient data are included. Period 1990-1999.
No statistically significant changes were found in any of the frequency or case-fatality indicators analyzed in females (Table 4).
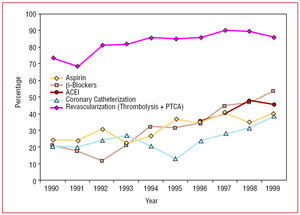
Figure 2 shows the evolution of the percentage of patients hospitalized and treated in the acute phase of AMI with those drugs and procedures demonstrating their efficacy in clinical trials. Thus, between 1990 and 1999, a significant increase was seen in the percentage of patients who received the different treatments. On the other hand, patient severity as measured by maximum Killip class did not change significantly (from 17.2% Killip class III-IV to 19.3%, respectively) during the period studied.
Figure 2. Percentage of patients hospitalized due to myocardial infarction receiving therapies with proven efficacy in the acute phase. Period 1990-1999.
DISCUSSION
Our results show that Girona, as in other areas of Spain and southern Europe, has lower AMI attack and mortality rates in the population aged 35-64 years than those of other industrialized countries.3-6 The incidence in the population aged 65-74 years is much higher than that in younger people of both sexes and, alarmingly, the population 28-day case-fatality due to AMI continues to be above 40%.18 The evolution of the indicators is different according to age group in males: the decrease in the number of cases in the population aged 35-64 years was not found in those aged 65-74 years. This indicates that the combination of primary and secondary prevention in the area has contributed to a delay in the incidence or recurrence of AMI in those aged 35-64 years to more advanced ages.
In males, the decrease in in-hospital case-fatality indicates that health care in the acute phase in AMI patients has significantly helped to reduce the number of fatal cases in the patients who reach hospital, although those over 64 years seem to have benefited more. There is no significant change in any indicator in females. This is probably due to the limited statistical power of the study, due to the very small number of cases of AMI in the female population and, perhaps, to the structural impossibility of modifying the indicators which are among the lowest in the world.
The population 28-day case-fatality after AMI in the present registry was lower (33.3% in males and 39.1% in females) than the mean in the MONICA project (49.0% and 53.8%, respectively) for the age group 35-64 years.4,19 This indicates that patient prognosis is better in Girona due to hospital treatment improving in the period between the two registries, the patients presenting less severe AMI or better access to hospitals. Case-fatality is 19% higher in females than in males. The countries with the lowest incidence of AMI have greater case-fatality in females than in males.4 It has been hypothesized that in the countries with low incidence non-fatal cases are diagnosed less frequently in females.4,7,20 The reasons for this variability should be investigated via specific in-depth studies.21,22
Some 66.8% of the patients who die do so before arriving at hospital. This percentage is higher in males than females, suggesting that, in women, death is basically due to heart failure rather than acute complications such as ventricular arrhythmias.22
Trend Analysis
Changes in incidence, attack, and out-of-hospital mortality rates tend to reflect the effects of primary prevention due to the changes in risk factors at the population level. On the other hand, the changes in case-fatality, especially in-hospital, are related to changes in the treatment of AMI patients or to severity in patients admitted to hospital. The changes in the recurrence rate would depend on the success of secondary prevention, both regarding controlling risk factors and the pharmacological treatment of the CHD patients.4,23-25 The situation is probably more complex in practice since the effects of treatment in the acute phase and primary and secondary prevention overlap.4,10,24
The decrease in the incidence, attack and recurrence rates in the population under 65 years, which is not found in the population aged 65-74 years, may reflect an improvement in the prevalence of risk factors thanks to primary and secondary prevention, thereby delaying the appearance of incident and recurrent AMI to more advanced ages. Other studies have supported the likelihood of this hypothesis in other contexts.13,26,27
In-hospital case-fatality has improved in males. This indicates that the treatment of the patients who arrive at hospital alive has been optimized, since its severity has not changed during the period studied. In fact, the percentage of patients who receive therapies with proven efficacy has increased during the study period. The effectiveness of this process of improvement in the use of platelet aggregation inhibitors and thrombolysis in the region has been shown in previous studies.9,28,29
Although the case-fatality of patients arriving at hospital alive (in-hospital case-fatality) has decreased considerably, the population case-fatality remains stable, both for males and females.18 In fact, some two-thirds of the deaths occur before the patient contacts the health system. This high percentage of out-of-hospital deaths highlights the key role of primary prevention in reducing AMI mortality.
The two main multicenter collaborative studies, MONICA, and Atherosclerosis Risk In Communities (ARIC), which were designed to analyze the trends in mortality and its determinants, differ in their conclusions regarding assessing the relative importance of changes in treatment or modification of risk factors in the reduction in observed mortality.4,8 Whereas the MONICA project researchers concluded that the reduction in mortality observed between 1985 and 1994 was basically due to a decrease in the number of cases, the ARIC study researchers (done in several communities in the United States) pointed out the key role in increased patient survival of improvements in treatment. Part of this discrepancy could be explained by the differences in the age groups analyzed (35-74 in the ARIC study and 35-64 years in MONICA), case definition, and study periods, in addition to the high percentage of Afro-American patients in the ARIC study and inequalities in access to the health services in the United States.
The results from the different centers in the MONICA study4 varied considerably regarding the age group 35-64 years. Both the attack and case-fatality rate decreased or remained stable in most western European centers. In the MONICA-Catalonia center the attack rate increased in males (1.0% per year) and case-fatality decreased in all the age groups (35-74 years).4,19 Part of these differences could be explained by the overlap of only 5 years between our registry and the MONICA-Catalonia registry, and the presence of an interaction between our age group and year of selection data, which is not addressed in the MONICA-Catalonia study.
Characteristics and Limitations of the Study
One of the problems common to AMI population registries is that it is not possible to obtain all the information necessary for definitively classifying the etiology of death, usually sudden, in some fatal out-of-hospital cases. Cases with "insufficient data" form a percentage of deaths similar to the MONICA study mean.4
The linear trend is the simplest of those trends that can be compared and the one more frequently used by authors who have addressed this type of analysis.4,8,19,25-27,30 Analyzing the trends via other nonlinear functions (quadratic or cubic) may present difficulties given the number of years available. A steady increase in the indicators of incidence and mortality in males was observed up to 1994 which subsequently decreased; thus, the evolution of these two indicators seems to be quadratic in form.
The trend analysis in woman and its interpretation is limited by the low number of events and the consequent instability of the estimations.
The results of the IBERICA6 (Research, Specific Search, and Registry of Acute Coronary Ischemia) study indicate that Girona has the lowest rate in the regions studied and, thus, cannot be extrapolated regarding magnitude to the rest of Spain. However, there is no reason why the temporal changes should be different from those observed in other regions.
CONCLUSIONS
Incidence and mortality rates due to AMI are low in Girona. Almost half of the patients with AMI die within 28 days following symptom onset and two-thirds of these without accessing hospital care. The improvements found in the attack, incidence and recurrence rates of cases of AMI in males aged 35-64 years between 1990 and 1999 were not seen in those aged 65-74 years, indicating a delay in age regarding AMI onset or recurrence. Attention in the acute phase of AMI has probably helped to reduce the number of fatal cases in hospitalized males, especially in those over 64 years. There are no changes in any indicator in females, who present extraordinarily low rates.
ACKNOWLEDGMENT
The authors would like to thank Rosa Gispert and Ana Puigdefábregas from the Servicio de Información and Estudios (Registro de Mortalidad) de la Dirección General de Recursos Sanitarios del Departamento de Salud for their collaboration and the Sistema de Emergencias Médicas SA del Servei Català de la Salut de la Generalitat de Catalunya. We also would like to thank Susanna Tello for database management, Marta Cabañero for interviewing the certifying physicians, and the relatives of the deceased, and Isabel Ramió for patient selection in the Josep Trueta hospital coronary unit in Girona. We would also like to thank all the registered physicians in Girona for their collaboration.
See editorial on pages 342-5
ABBREVIATIONS
ARIC: atherosclerosis risk in communities
CHD: coronary heart disease
AMI: acute myocardial infarction
IBERICA: Research, Specific Search, and Registry of Acute Coronary Heart Disease
MONICA: Monitoring Trends and Determinants of Cardiovascular Diseases
REGICOR: Girona Heart Registry
A complete list of the REGICOR researchers can be found at: www.regicor.org/regicor_inv
This study has been financed by the Health Research Fund: grants FIS90/0672, FIS93/05, HERACLES network (RD06/0009 68), RCESP network (C03/09), CIBER de Epidemiología y Salud Pública (CB06/02) and Agència de Gestió d'Ajuts Universitaris de Recerca SGR-2005/00577, and research contract FCI CP05100290.
Correspondence: Dr. R. Elosúa.
Unidad de Lípidos y Epidemiología Cardiovascular.
Instituto Municipal de Investigación Médica.
Dr. Aiguader, 88. 08003 Barcelona. España.
E-mail: relosua@imim.es
Received July 18, 2006.
Accepted for publication November 23, 2006.