A 62-year-old previously asymptomatic man was attended in the emergency room for anginal chest pain of 6 hours’ evolution. His medical history was remarkable for a combined aortic and mitral valve replacement 15 years previously for endocarditis (anticoagulation with acenocoumarol) and an aneurysm of the noncoronary sinus and ascending aorta, treated with an end-to-end anastomosis (Dacron graft) 2 months previously.
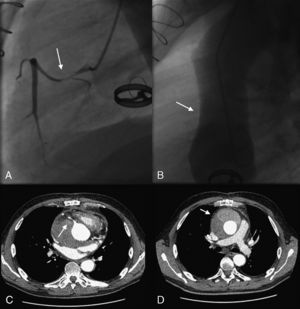
The patient was hemodynamically stable and had persistent pain. The physical examination was not contributory and the surgical wound appeared to be healing well. The ECG showed a known left bundle branch block without changes. During the initial evaluation, echocardiography showed inferior akinesia that was not present on the postoperative study, and a normally functioning graft, without clear visualization of the ascending aorta. An onset of infarction was suspected and 250 mg of aspirin was administered. Angioplasty was contemplated, and coronary angiography performed 60min after his arrival showed subtotal occlusion of the right coronary artery (RCA) (Figure 1A). Aortography disclosed deformation of the anterior aortic wall, indicating extrinsic compression (Figure 1B). Conventional computed tomography demonstrated a hematoma affecting RCA flow (Figure 1C and D). The troponin I level and creatine kinase-MB fraction were 4 ng/mL and 10 ng/mL and reached levels of 26 ng/mL and 40 ng/mL, respectively (data available at 90 min after his arrival). The international normalized ratio was 3.68. The patient underwent drainage and closure of the leak, which was located in the proximal suture of the Dacron graft. Blood cultures were negative and there were no postoperative incidents. This case illustrates the advantages of primary angioplasty with respect to fibrinolysis, particularly when there is an uncertain diagnosis of acute infarction and a risk of unnecessary fibrinolysis.
Figure 1.
Corresponding author: pablo.pazos.lopez@gmail.com