Heart failure (HF) is becoming a modern epidemic and, despite advances in therapy, is still characterized by adverse prognosis, with significant residual mortality and high hospitalization rates.1,2 One of the main reasons is the high prevalence of the disease and the lack of effective disease-modifying therapies for HF with preserved left ventricular ejection fraction (HFpEF). In fact, HFpEF represents the most prevalent form of the syndrome in elderly patients, particularly women, and patients with comorbidities, while all clinical trials that have tested neurohormonal blocking agents, which represent the mainstay of treatment of HF with reduced ejection fraction (HFrEF), have failed in HFpEF.1,3 Some of the potential reasons for the failure of HFpEF trials are the poor understanding of the underlying pathophysiology and thus the inappropriate selection of therapeutic targets and interventions, the heterogeneity of the affected populations, and the choice of trial endpoints. As a result, there is a substantial unmet need for alternative therapies and clinically relevant endpoints for HFpEF.
Reduced exercise capacity is a key symptom of HF patients that is generally overlooked compared with other manifestations such as dyspnea or peripheral edema. In HFpEF, in particular, exercise intolerance is the primary chronic symptom. Peak oxygen consumption is up to 70% lower in HFpEF patients than in age-, sex- and comorbidity-matched controls without HF and is similar to that observed in HFrEF patients, even though HFpEF was once deemed a less severe syndrome than HFrEF.4,5 In addition, exercise parameters, particularly the relationship between minute ventilation and the rate of CO2 elimination (VE/VCO2 slope), have prognostic significance in HFpEF.5 Bearing in mind the above, exercise intolerance should be treated both as a therapeutic target and a surrogate endpoint for HFpEF.
Previous studies have shown that exercise training in HF is safe and confers beneficial effects mainly in terms of exercise capacity and quality of life, with some evidence of a reduction in hospitalization and doubtful evidence on survival.6,7 In the case of HFpEF, a meta-analysis of 6 small randomized trials showed that exercise training improved exercise capacity, as documented by peak oxygen consumption, as well as quality of life.8 Despite the limited evidence on “hard” endpoints, such as survival and hospitalization, exercise capacity is per se an important endpoint, as previously stated, which should be focused on by HF care. However, physical training is limited by the often low patient adherence to exercise protocols, due to either poor functional status and severe exercise intolerance and thus inability to train or due to lack of proper motivation or willingness to exercise.6,9 Thus, the need for alternative modes of training that would allow the benefits of exercise and at the same time overcome the issues of inability or unwillingness to train could represent an important therapeutic modality in HFpEF.
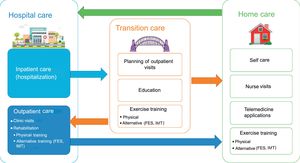
Alternative modes of exercise, including functional electrical stimulation (FES) and inspiratory muscle training (IMT), offer the possibility of training to patients who are either unable or unwilling to exercise physically. Small clinical studies, concerning mainly HFrEF patients, have shown beneficial effects of both modalities, including improvement in functional status, exercise capacity, emotional status and quality of life, while some studies have further documented benefits in diastolic and endothelial function indices.10–14 The alternative training programs can be used either as a “destination therapy” in patients with limiting comorbidities, such as mobility issues or those with advanced HF, or as a “bridge to physical training” in patients uncompliant with exercise programs or with less severe functional impairment expected to improve.9 These methods have additional advantages as they are low-cost and safe and do not require sophisticated facilities, meaning that they can be easily performed at home after a short training session. Home-based HF management programs have lately attracted much of attention as they combine higher adherence with lower costs and they further contribute to the transition of hospital to outpatient care (Figure 1).15
Overview of comprehensive heart failure management, including hospital-based and home-based care. Alternative forms of exercise training, including FES and IMT can be performed either in rehabilitation centers or at home, and can thus be part of both hospital and home heart failure care. Transition to chronic outpatient care following hospitalization is crucial to ensure improved outcomes and reduced health care expenditure, including low rehospitalization rates. FES, functional electrical stimulation; IMT, inspiratory muscle training.
In a recent article published in Revista Española de Cardiología, Palau et al.16 report the results of a study addressing the effects of FES and IMT, either as separate or combined interventions, on exercise capacity in patients with HFpEF. This is actually the first randomized study testing the combination of these 2 alternative modes of training in HFpEF. Patients enrolled in the trial had severe baseline exercise limitation, with a mean peak oxygen consumption of 9.9mL/min/kg, only to confirm the importance of exercise intolerance in HFpEF. In line with previous studies in HFpEF,11,14 the authors were able to show that the 2 interventions, applied either separately or in a combined protocol, significantly improved exercise capacity and quality of life at the end of a 3-month training period, an effect that persisted at 6 months, while no benefit was observed in biomarkers or diastolic function indices.
Selecting the proper study population for a clinical trial in HFpEF can be quite challenging. In the study by Palau et al.,16 the authors had to exclude patients unable to perform a cardiopulmonary exercise test, such as those with mobility issues, as this was the primary endpoint of the study. In addition, the authors also excluded patients with severe pulmonary disease, including chronic obstructive pulmonary disease. Both chronic obstructive pulmonary disease and inability to perform an exercise test are, however, expected to be prevalent in an elderly HFpEF population, and thus their exclusion may have resulted in over-selection of the study population. The lack of incremental effect of the combined FES-IMT protocol may actually be relevant to the selection of the study population and thus further studies addressing the combination of the 2 modalities in a broader HFpEF population may be warranted.
In summary, exercise training is beneficial and should be part of HF management programs, particularly in the case of HFpEF, in which no disease-modifying therapies exist so far and in which exercise intolerance is the primary symptom. This is clearly stated in the recent HF guidelines, according to which exercise training should be part of multidisciplinary HF management.3 In this context, alternative modes of exercise training, such as FES and IMT, could be considered if patients are unable to follow or are not compliant with physical training programs, as these methods are beneficial, safe, low-cost, and can be easily performed even at home. Since clinical studies on FES and IMT in HF have hitherto been small and rather proof-of-concept, these alternative methods should be studied in larger randomized trials with broad HF populations, longer periods of training, and clinically meaningful surrogate endpoints as outcome measures.
CONFLICTS OF INTERESTThe authors declare having no conflicts of interest related to this work.