An 85-year-old woman with moderate-to-severe mitral regurgitation (MR) with preserved left ventricular (LV) function successfully underwent transapical neochord mitral valve repair, with access closure using double pledgeted purse-strings. No perioperative complications were registered, and a predischarge transthoracic echocardiogram showed only mild MR.
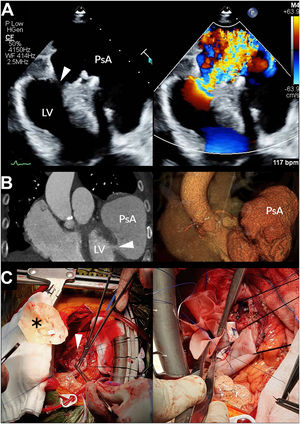
Seven months later, the patient underwent a routine transthoracic echocardiogram (figure 1A, videos 1-3 of the supplementary data), revealing a contained rupture of the LV lateral wall (arrowhead) and severe MR. The patient reported recent worsening of exertional dyspnea and orthopnea, which she overlooked, and showed a grade III/VI murmur, jugular vein distension, and bilateral rales. Electrocardiogram-gated cardiac computed tomography scan (figure 1B) disclosed a pseudoaneurysm of the LV anterolateral wall, with a wide neck (arrowhead), corresponding to previous ventricular access site.
The patient underwent surgery through full sternotomy. LV free wall rupture repair (figure 1C) was accomplished with a heterologous pericardium patch (asterisk), designed to re-establish LV geometry. The patch was sutured with pledgeted interrupted sutures, with the edge oversewn to the myocardium with a continuous Prolene running suture. Mitral valve replacement with a bioprosthesis was also performed. The patient made an uneventful recovery and was discharged 7 days later in New York Heart Association functional class II.
Access site complications related to the transapical approach, such as aneurysm formation, have been described. LV rupture is a rare but potentially catastrophic complication of neochordoplasty using transapical access. We highlight the peculiarity of this clinical presentation, which is unusual in the outpatient setting, and the successful intervention that avoided an unfavorable outcome.
The patient consented to this publication during her latest follow-up visit.
FUNDINGThe authors did not receive any funding.
AUTHORS’ CONTRIBUTIONSS. Simões Costa, and M. Brandão equally contributed to the article (conception, writing of the manuscript and selection and edition of image material), and therefore share first authorship. D. Martins was the senior cardiothoracic surgeon involved in the case, and reviewed the manuscript and supervised the selection of image data.
CONFLICTS OF INTERESTNo conflicts of interest to declare.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2021.03.004