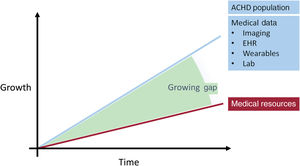
Medical advances in the treatment of young patients with congenital heart defects have led to a sharp increase in the number of adults with congenital heart defects (ACHD) in recent years, and their number will continue to rise.1 These patients require long-term medical monitoring with repeat examinations and interventions, which is a challenge for health systems worldwide. Treatment is mainly carried out in specialized tertiary centers, where it requires considerable resources. In the coming years, it will be crucial to improve the efficiency of medical care for this growing group of patients by adapting a new “intelligent” patient-centered approach. Artificial intelligence (AI) and new technologies have shown promising results in other medical fields and could therefore also improve the treatment of ACHD patients in the future.2,3 AI could particularly help facilitate the intelligent and rapid processing of large volumes of electronic health records (EHRs) and medical images, could assist in solving diagnostic problems, and make medical decisions with greater accuracy than traditional risk models.4 Last, but not least, remote monitoring of implantable or wearable electronic devices (eg, pacemakers) or of vital signs, clinical status and daily physical activity by using mobile smartphone applications or smart watches is a simple, time- and cost-efficient way to follow-up for patients. This could also reduce the burden on physicians and increase patients’ autonomy.
ARTIFICIAL INTELLIGENCEAI is an aspect of computer science and engineering that was introduced with the advent of adequate computing power and robotic technology in the middle of the 20th century. It aims to create “intelligent” machines that (to some degree) imitate human thinking processes.5 Several developments in recent years have led to the increasing use of AI in medicine. These include advances in computer development with powerful computers (especially fast graphic processing units), the availability of large amounts of medical data, and the emergence of novel and improved algorithms. These advances have led to its adoption in medicine as well, with the aim of improving the efficiency and quality of patient care, increasing cost-effectiveness, making predictions, exploring new genotypes and disease phenotypes, and ultimately increasing life expectancy.4
The application of AI in medicine includes machine learning (ML) and deep learning (DL). ML uses mathematical algorithms to solve complicated problems based on big data by identifying patterns of interaction between variables. Big data refers to extremely large and usually unstructured data sets, such as EHRs, “omic” data, portable technology, and mobile phone applications, which cannot be analyzed, searched, interpreted or stored using traditional data processing methods. ML aims to develop automated algorithms for prediction and clinical decision-making that provide a more accurate approach than simple estimated assessment systems.6 Overall, 3 general types of ML algorithms are worth mentioning: supervised, unsupervised, and reinforcement algorithms.2 Supervised algorithms use a human labeled data set to predict the desired outcome. Their application focuses on classifying the disease or predicting a known event based on previous examples.
In contrast, unsupervised learning only provides unlabelled input data and uses algorithms to find inherent clusters or associations (such as correlations). The hope is that these may represent a hitherto unknown clinical outcome, genotype, or diagnosis. Reinforcement learning combines supervised and unsupervised learning to maximise the accuracy of the algorithms through trial and error and should have a particular role in robotic technology (such as autonomous echocardiography robots) in the future.
DL is another aspect of AI that mimics the organization and function of the human brain. It includes recurrent neural networks, convolutional neural networks, and deep neural networks, which are widely used in cardiology and more recently in ACHD for computer-aided image analysis, as they promise to increase efficiency and diagnostic quality. DL involves the use of multiple hidden layers of artificial neural networks to generate automated predictions from input neurons (training imaging datasets).
POSSIBLE APPLICATIONS OF AI IN ACHD CAREIn “classical” medicine, diagnostic procedures, acquired knowledge and physician experience are used to identify and treat a patient's illness. Through their knowledge and experience, human experts accept a diagnosis, which then guides the treatment according to the common tenet. In this process, the available information is often reduced to a few, easily accessible parameters (eg, ejection fraction) and the patient is thus assigned to a specific disease entity (eg, heart failure). In contrast, the advantage of “AI-supported medicine” is the simultaneous evaluation of a multimodal input (unstructured clinical data, clinical signs, electrocardiogram data, raw imaging data, remote monitoring data, genetic and laboratory data), which in turn allows a completely new definition of the disease.
DL networks are trained using patient data (input) to develop precise mathematical models that can predict clinical outcomes, control the escalation of medication, or demonstrate the need for an interventional approach to treating disease complications. Theoretically, this also opens up opportunities for specific AI-based therapies.
Another aspect of AI in ACHD patients could be for disease prevention. There are usually considerable delays between the onset of symptoms, the patient's presentation to a physician and finally the establishment of a diagnosis, which in turn leads to subsequent treatment. An early or immediate diagnosis by a smartdevice with AI support would allow a diagnosis to be made much faster and the therapy to be started earlier by the physician (eg, anticoagulation for newly diagnosed atrial fibrillation). In addition, certain DL algorithms have been developed to improve the role of imaging in the diagnosis and prediction of prognosis in the ACHD population.
IMAGE ACQUISITION AND IMAGE OPTIMIZATIONCardiovascular imaging is perhaps the most obvious target area in cardiovascular medicine for testing ML. It is also the area where these technologies have shown the greatest immediate benefit for more efficient image acquisition and reconstruction, automated quality control and image segmentation, and computer-aided diagnosis in early feasibility studies.
AI can provide diagnostic assistance (classification) as early as during the acquisition of image data. For example, the long acquisition time for cardiac magnetic resonance imaging (MRI) examinations can be shortened by ML-based techniques.7 Specifically, AI offers a promising possibility to perform cardiac MRI acquisition with under-sampling strategies, in which fewer image data are acquired than necessary, followed by a learning-based estimation of the sparse area from existing data.
Transthoracic echocardiography is the central imaging modality in the treatment of ACHD patients.8 However, due to the complex cardiac anatomy, the often difficult visualization of the heart structures after previous surgery, an accompanying lung disease and the occasionally abnormal situs, the image quality can sometimes be suboptimal, hampering precise assessment and diagnosis. Recently, DL algorithms have been successfully used to denoise transthoracic echocardiographic images in patients with ACHD.9 In our work, we developed deep neural network-based autoencoders for denoising and removal of acoustic shadow artefacts based on routine echocardiographic apical 4-chamber views in ACHD patients and normal controls.9 Noise reduction autoencoders are a special form of deep neural networks that are used to reconstruct an output (improved quality of the original image) from a given input (original image with artefacts). In that study, the autoencoders significantly improved the image quality across the entire ACHD spectrum. Consequently, AI could be used in daily practice to improve echocardiographic image quality in selected patients, thus helping to avoid expensive and less widely used examinations such as cardiac MRI. These technologies are also essential for downstream applications of other DL networks.
SIGNAL PROCESSINGElectrocardiography is a very important examination for detecting arrhythmias and conduction abnormalities in the ACHD population. However, the interpretation of ECG signals is very subjective. Modern signal processing and AI techniques will significantly increase the accuracy and diagnostic power of ECGs and eliminate much of the ambiguity in interpretation. AI algorithms will be able to measure certain ECG characteristics such as - P, QRS and T wave duration, amplitude and end of ST segment amplitudes.10
In addition, studies on the interpretation of heart sounds in congenital heart defects have been carried out in recent years.11,12 Heart sound analysis is a noninvasive and cost-effective diagnostic method for both children and adults. Since the methods used could distinguish between normal and pathological heart sounds, they could be a suitable screening tool.
PREDICTION OF CLINICAL OUTCOMESIn addition to improving image quality and the possibility of image classification and segmentation, AI could also be used to predict clinical outcomes and to control patient management. In a prospective study of 372 patients with tetralogy of Fallot, DL models were used to analyze cardiac MRI images (image segmentation) and a prognostic model was developed based on specific MRI measurements.13 A model was trained using images from a single center (local training set) and then used on an independent observation cohort of patients with recorded clinical results (national validation set). The measurements from the volumetric analysis were used to create a prognostic model that showed increased right atrial area and decreased right ventricular longitudinal dilatation as independent predictors of adverse outcomes (cardiac death or near missed cardiac death or ventricular tachycardia). This study demonstrates the usefulness of ML-based DL algorithms trained on an external data set to predict prognosis directly on an independent multicenter cohort of cardiac MRI images of patients with tetralogy of Fallot. In the future, AI could provide longitudinal and automated assessment of ventricular function and dimensions and guide the management of patients with tetralogy of Fallot or other cardiac lesions on the go without human interference.
Another study also showed that in a large group of voluntary test persons such as the UK Biobank, certain cardiac changes can be filtered out by clustering.14 For example, examinations with an enlarged right ventricle could be identified using unsupervised analysis.
Finally, another clinical application of DL could be natural language processing of EHRs to extract data collected for routine care and combine them in risk stratification models. With the growing amount of patient data in the large tertiary centers, manual data collection and curation in a form suitable for statistical analysis is becoming a logistical challenge as it is very time consuming. Successful attempts have been made to create specific DL models based on raw data obtained from 44 000 medical records of 10 019 ACHD patients in a tertiary center and to automatically categorize the diagnostic group, disease complexity, and New York Heart Association class.15 In addition, models have been developed to assess the need for discussion at meetings of multidisciplinary teams and to predict medical therapy. Finally, an automatically (based on a DL model) derived disease severity score was developed, derived from clinical variables automatically retrieved from medical records (age, diagnosis, symptoms/clinical status, and medication) and related to survival, independent of demographic, exercise, laboratory and ECG parameters. This study offers a new perspective on the usefulness of ML algorithms trained on large data sets to accurately transform medical letters into meaningful clinical variables that could be used to estimate prognosis and possibly guide therapy in ACHD.
POTENTIAL PITFALLS AND FUTURE DIRECTIONS OF AI IN ACHDThe use of ML in the care of ACHD patients has huge potential, but is also associated with challenges that cannot be underestimated. For example, the applicability of algorithms developed under research conditions for the care of real ACHD patients must be evaluated in detail. In this respect, particular attention must be paid to typical pitfalls of AI, such as an unsuitable training data set or insufficient statistical adjustment for multiple tests. For example, an unbalanced consideration of sex or ethnicity in the training data set can make the transferability to a deviant patient collective incorrect. To avoid these pitfalls (bias), a deep understanding of AI and a careful evaluation by clinicians and researchers is essential.
The widespread use of AI in ACHD is an unmet need that will improve patient care in an efficient and cost-effective way (figure 1). The implementation of DL algorithms to improve image acquisition and interpretation, automatic processing of heterogeneous data for severity prediction and therapeutic decision-making across a broad clinical spectrum will increase the accuracy and effectiveness of clinical decisions and the overall long-term care of ACHD patients. In addition, analysis of genomic and proteomic data and their integration into predictive models will play a key role in the calculation of risk scores for predisposition to acquisition, phenotyping and survival.
CONCLUSIONAI is a novel computational tool that could be widely applied in the field of ACHD to increase the quality and precision of health care delivery in a cost-effective way. Prospectives studies in large populations are warranted to ensure applicability and reduce pitfalls and biases.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest in relation to this article.