To the Editor:
Behçet's disease is a systemic illness characterised by orogenital ulcers and uveitis that can affect the articular, gastrointestinal, cardiovascular, and neurological systems.1
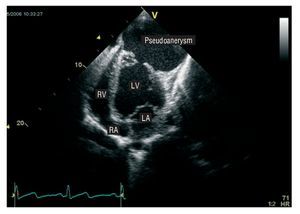
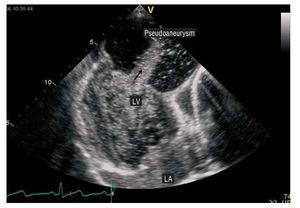
We present the case of a 23 year-old North African male without cardiovascular risk factors, who arrived at the emergency room with chest pain that had been developing for 15 days. The chest pain was made more acute when taking deep breaths. The patient also experienced dysthermia and was shivering. Physical examination revealed a fever of 38.5oC, orogenital ulcers, pansystolic murmur upon cardiac auscultation, and an apical beat displaced upwards and to the left. The ECG registered sinus rhythm with Q waves in the precordial derivations. Concentrations of troponin I (5.5 ng/dL) and C-reactive protein (15.4 mg/dL) were high, and so was the globular sedimentation velocity (108 mm/s). The chest x-ray showed a left paracardiac mass that obscured the cardiac silhouette. The transthoracic echocardiography showed a pseudoaneurysm of massive dimensions (59´86 mm) on the anterolateral wall of the left ventricle, with a thin neck (2.5´3 mm) (Figure 1) The contrast echocardiography showed that there was flow between the left ventricle and the pseudoaneurysm (Figure 2), which eliminated the possibility of thrombi in the interior. The rest of the examination was normal. The coronariography showed epicardial arteries of normal size and only the second diagonal artery, a branch of the anterior descending artery, was occluded.
Figure 1. Transthoracic echocardiography, apical view with 4 cameras. This image shows the massive pseudoaneurysm located along the anterolateral wall of the left ventricle. RA: right atrium; LA: left atrium; RV: right ventricle; LV: left ventricle.
Figure 2. Contrast echocardiography. Administration of contrast shows the close connection between the ventricular cavity and the aneurysmal sac with flow between the 2 cavities (arrow). LA: left atrium; LV: left ventricle.
The patient underwent operation to remove the pseudoaneurysm, and there were no complications in the post-operatory period. The anatomopathologic study showed abundant fibrous tissue with areas of acute and chronic inflammation, with an abundance of neutrophils and thrombotic areas.
To study the febrile syndrome, a thoraco-abdominal computerised tomography was taken that clearly showed thrombosis of the hepatic portal vein. Blood, urine, and faeces tests, and those from the extirpated mass, were negative.
The co-existence of orogenital ulcers and the extensive cardiovascular damage, together with the high concentration of acute phase reactants led to the diagnosis of Behçet's disease.
Behçet's disease is a vascular illness that affects the skin, mucous membranes, articulations, and the cardiovascular, neurological, and gastrointestinal systems.2 Cardiovascular conditions in particular have been described in 7%-46% of all patients.2 It generally affects young patients and includes coronary and valvular heart disease,2-3 myocarditis, and pericarditis,2 and the formation of intracavity thrombi. Ventricular pseudoaneurysms in Behçet's disease are exceptional4,5 and they appear most frequently after an acute myocardial infarction. In this instance, the coronariography showed total occlusion of a diagonal branch of the descending anterior artery. The anterolateral position of the pseudoaneurysm could be related to the thrombosis of the mentioned coronary artery and the resulting infarction of the anterolateral ventricular wall. Unlike other published studies, our case did not present aneurysmal lesions in the other epicardial coronary arteries.6 However, peripheral vascular conditions were found with thrombosis of the portal vein. Thrombosis of large veins, particularly the upper and lower venae cavae and the hepatic veins, has also been described, with frequency of up to 22%.1