Atrial fibrillation (AF) is the most common cardiac rhythm disorder in patients with or without structural heart disease.1–3 Known risk factors include aging, hypertension, diabetes mellitus, coronary artery disease (CAD) and pre-existing heart failure, to name the most frequent.4,5
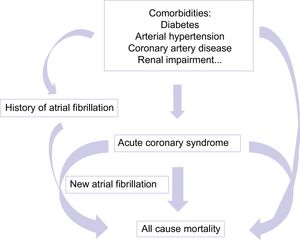
In patients with CAD who require percutaneous coronary intervention (PCI), approximately 5% to 8% have been diagnosed with AF and, due to an increased CHA2DS2-VASc score, are in need of oral anticoagulation.6 In terms of patient management, this condition is extraordinary complicated, with the possible occurrence of multiple problems (Figure 1).
As a first problem, the strategy of combining dual antiplatelet therapy (DAPT) including P2Y12 inhibitors with oral anticoagulation (vitamin K antagonists [VKA] or nonvitamin K antagonists oral anticoagulants [NOAC]) not only lacks data but also increases the risk of major bleeding.7 Only recently, 2 prospective multicenter trials have been published that attempt to determine the risk of major bleeding. Both showed that oral anticoagulation in combination with a P2Y12 inhibitor is a feasible approach, resulting in a better outcome than long-term “triple therapy” consisting of dual antiplatelet therapy or a PY12 inhibitor and aspirin and an additional oral anticoagulant, either a vitamin K antagonist or a NOAC. This strategy ensures that the risk of stent thrombosis and early in-stent stenosis is reduced, as well as the risk of cardioembolic events in patients with stable CAD.6,8
The second problem is that due to an increased risk of bleeding, especially if patients are treated with a VKA, the periprocedural risk of bleeding and severe complications during PCI are elevated, making the decision in favor of PCI more difficult. In particular, bleeding from the arterial puncture site is a dreaded complication, requiring safe access with a good possibility of manual compression if complications occur, leading to a preference for radial rather than femoral access for coronary angiography or PCI.4
The situation can be even worse if new-onset AF occurs during acute myocardial infarction (AMI), leading to poor prognosis with a 2-fold in the risk of death, congestive heart failure, and stroke.9 Episodes of new AF in acute coronary syndromes (ACS) occur most frequently within the first 4 days after AMI. This might be related to frequently coinciding conditions such as heart failure, mitral regurgitation, or a general acute phase/inflammatory response caused by myocardial infarction.10 In a general AF population, the risk of death due to ACS is 5.9%, exceeding that of ischemic stroke (5.1%).11
There are several aspects worth discussing in the context of AMI and AF related to the findings of the work by Biasco et al.12 recently published in Revista Española de Cardiología. In the analysis, 35 958 patients were included in total. The included patients had been treated in Switzerland from 2004 until 2015 due to ACS and had been included on a voluntary basis in the Acute Myocardial Infarction in Switzerland registry (AMIS) Plus. In the analysis, patients were first divided into groups, depending on their known history of AF at hospital admission: no known history of AF group (no-AF), history of AF (pre-AF) and admission in sinus rhythm and first diagnosis of AF during hospital stay (new AF). Interestingly, this analysis showed 1644 patients (4.7%) with pre-AF and 309 (0.8%) with a first diagnosis of AF during hospital stay because of AMI. This is astonishing, since other trials and registries have reported the incidence of AF in such patient groups as 6% to 8%, respectively.9,10 This could possibly be explained by the different definition of new AF and pre-AF in this retrospective registry, which therefore differs from the patient cohorts in other clinical investigations.
In the comparison of patients with pre-AF vs new AF, there are interesting differences in patient comorbidities. As known risk factors of AF and CAD, pre-existing hypertension was significantly more frequent in patients with pre-AF; however, the prevalence of prior CAD and ST-segment elevation myocardial infarction was approximately 2-fold higher in patients with new AF. In addition, the need for intra-aortic balloon pulsation was higher. In contrast, heart failure on admission was twice as frequent in patients with pre-AF than in those with new AF. During hospital stay, there was no difference in terms of cardiogenic shock or mortality between the AF groups in the current study.
A key observation in the huge set of data and inclusion period over a decade is the following finding: only 56.5% of patients presenting with an ACS and pre-existing AF in this registry underwent coronary angiography. The reasons can only be speculated: patients with known AF are already treated with VKA or NOAC at admission to hospital because of ACS and therefore the risk of a bleeding complication during coronary angiography or PCI is elevated. Furthermore, at the beginning of the data analysis of this registry, use of femoral access for coronary angiography and PCI was more common than radial access. It is known that femoral access can cause higher complication rates.
The next interesting observation concerns the reported patient symptoms at admission. In the pre-AF group, only 75.4% patients presented with chest pain, but 49.6% had dyspnea, which was the leading cause of hospital admission. In comparison, in the non-AF group, more than 80% of patients underwent coronary angiography and presented with rather typical symptoms (87.6% with chest pain and only 29.6% with dyspnea).
The decreasing rate of all-cause mortality, observed in the pre-AF group, is in line with an increasing rate of coronary angiography and PCI in this group. This phenomenon was not observed in the new-AF group, in which the percentages of CAD and PCI were increased but without a decrease in mortality. This phenomenon was not observed in the new AF group, in which the percentage of CAD and PCI also rose without a decline in mortality.
As previously mentioned, patients with VKA therapy are at higher risk of bleeding complications during PCI. The guidelines stress that radial access is superior to femoral access.4
Interestingly, in the work by Biasco et al.,12 in patients with pre-existing AF, radial access was used only in 24.2% of patients compared with over 30% in the other groups.
Bleeding complications were also higher in the AF groups, as expected; however, patients with new AF more frequently had clinically relevant bleedings and cerebrovascular events than pre-AF patients. This is particularly interesting, since these patients receive DAPT after the intervention, which would consist of either prasugrel and ticagrelor, rather than clopidogrel, which is the only P2Y12 inhibitor eligible for combination with oral anticoagulation.6,8 This could possibly be a confounding factor.
In summary, this registry analysis shows the complicated and sometimes conflicting situation of patients in AF presenting with ACS in a real world setting. The patients were analyzed during a decade when important studies were published and relevant changes were made to guidelines. In this special setting and with patients classified into those with new AF vs pre-AF and with division of the inclusion time in the registry, there were 2 very important findings. First, the prognosis of patients presenting with pre-AF markedly increased over the 10-year time period. Second, until now, patients with AF, whether pre-existing or new-onset during AMI, had a worse prognosis, even though patients with new-onset AF had fewer comorbidities and risk factors. Finally, the importance of “undertreatment” with fewer interventions should be considered as an additional confounder for higher mortality rates.
In line with previous studies, the registry demonstrates that patients with ACS and severe comorbidities, such as AF, are at high risk of increased mortality, which has therefore to be taken into special account in decision-making on further therapy strategies. Regarding anticoagulation and DAPT, an individually-tailored approach is essential.
CONFLICTS OF INTERESTV. Johnson: speaker honorary from BMS/Pfizer, Biotronik. J. Schmitt: Advisory Board: Biotronik, BMS/Pfizer; speakers bureau: Abbott, Biotronik, BMS/Pfizer, CVRx, Daiichy Sankyo, Medtronic, Zoll CMS; Research Grant: Abbott, CVRx, Zoll.
.