This article presents the most relevant developments in 2013 in 3 key areas of cardiology: congenital heart disease, clinical cardiology, and heart failure and transplant. Within the area of congenital heart disease, we reviewed contributions related to sudden death in adult congenital heart disease, the importance of specific echocardiographic parameters in assessing the systemic right ventricle, problems in patients with repaired tetralogy of Fallot and indication for pulmonary valve replacement, and confirmation of the role of specific factors in the selection of candidates for Fontan surgery. The most recent publications in clinical cardiology include a study by a European working group on correct diagnostic work-up in cardiomyopathies, studies on the cost-effectiveness of percutaneous aortic valve implantation, a consensus document on the management of type B aortic dissection, and guidelines on aortic valve and ascending aortic disease. The most noteworthy developments in heart failure and transplantation include new American guidelines on heart failure, therapeutic advances in acute heart failure (serelaxin), the management of comorbidities such as iron deficiency, risk assessment using new biomarkers, and advances in ventricular assist devices.
Keywords
Two studies have analyzed the risk factors for sudden death (SD) in adult congenital heart disease. Koyak et al1 conducted a multicenter study using 3 large databases that included more than 25000 patients. The total mortality rate was 5%, of which 19% was due to SD. The underlying congenital heart disease in SD patients was classified as mild, moderate, and severe in 12%, 33%, and 55%, respectively. Risk factors associated with SD were supraventricular arrhythmias, ventricular dysfunction, increased QRS duration, and QT dispersion. In Spain, Gallego et al2 analyzed the incidence of SD in 936 adults with previously repaired congenital heart disease. During follow-up, the total mortality rate was 5.3% and the incidence of SD was 2.6/1000 patient-years. The highest incidence of SD occurred in patients with transposition complexes. Independent risk factors of SD were delayed initial examination in adults and severe systemic ventricular dysfunction.
Systemic Right VentricleThe assessment of ventricular function in the systemic right ventricle is particularly challenging. Cardiac magnetic resonance (CMR) imaging has become the gold standard, but is of limited use in patients with pacemakers or implantable cardioverter-defibrillators. A group from the University of Bern3 compared echocardiography-derived parameters with CMR-derived systemic right ventricle ejection fraction in adults with transposition of transposition the great vessels who had undergone the Mustard/Senning procedure. Routine nongeometric echocardiographic parameters (lateral tricuspid annular plane systolic excursion, lateral right ventricle systolic motion velocities assessed by tissue Doppler, total ejection isovolume index) were weakly correlated with CMR-derived systemic right ventricle ejection fraction. The dp/dt measured across the tricuspid regurgitant jet and fractional area change were significantly correlated with the CMR-derived systemic right ventricle ejection fraction. A fractional area change<33% (area under the receiver operating characteristic curve=0.73) identified an systemic right ventricle ejection fraction<50% with high sensitivity and specificity. Furthermore, a study conducted at the Royal Brompton Hospital4 demonstrated that heart deformation or systolic right ventricle longitudinal strain is significantly reduced in patients with systemic right ventricle, is related to subpulmonary ventricular function, and predicts adverse clinical outcomes in adults following physiological repair of transposition the great vessels (atrial switch).
Van der Bom et al5 conducted a multicenter, randomized, double-blind, placebo-controlled pilot trial of valsartan on systemic right ventricle function, functional capacity, B-type natriuretic peptide concentrations, and quality of life of patients with atrial switch or congenitally corrected transposition the great vessels. Although no significant treatment effects were found, possibly due to the small sample size, the most positive aspects were: a) the absence of adverse effects; b) a smaller increase in ventricular volume and mass in the treatment group, and c) less deterioration of ventricular function in symptomatic patients treated with valsartan. This pilot trial opens the door to other larger trials to explore the long-term effect of drugs routinely used in adults with ventricular dysfunction in this specific group of patients.6
Tetralogy of FallotTetralogy of Fallot has the highest postoperative survival rate among cyanotic congenital heart disease and is the most studied congenital heart disease in the adult population. The greatest uncertainty associated with this defect is the long-term risk of SD. To date, more than 30 risk factors have been proposed, of which age at repair, QRS duration, right ventricle enlargement, and left ventricular dysfunction are most predictive.7 Diller et al8 included in this long list echocardiographic parameters that measure longitudinal left venticular function, particularly mitral annular plane systolic excursion and longitudinal strain. Unfortunately, the plethora of proposed risk factors indicates the difficulty of finding simple methods that have high predictive value.
Hickey et al9 analyzed the functional health status of adults with Tetralogy of Fallot in a large patient population. Although long-term survival was excellent, almost 50% of patients had cardiorespiratory symptomatology, and physical functioning decreased with advancing age. A similar study found that functional health status was significantly worse in adults surviving Tetralogy of Fallot repair than that of their age-matched healthy siblings.10 Chronic pulmonary disease is the main hemodynamic problem associated with decrements in functional health status. Thus, the optimal timing of pulmonary valve replacement remains an unresolved issue.11 The use of CMR has become the main focus in the debate. If the goal is to normalize right ventricle volumes after valve replacement, surgery is recommended12 before the end-diastolic volume index is>160mL/m2 or end-systolic volume index is>80mL/m2. However, if the target is midterm survival or the incidence of arrhythmias or SD, these criteria have no demonstrated predictive value.13 Early indications based on ventricular volume should be weighed against the great number of reoperations for deterioration of prosthetic valve function. Moreover, other authors14 have not found a ceiling beyond which right ventricle end-diastolic and end-systolic volumes did not “normalize”.
It has been suggested that in both Tetralogy of Fallot and transposition of the great vessels there is an aortic pathology involving histological changes that are similar to those found in Marfan disease. This aortic disease can manifest in these patients as increased aortic root diameter, abnormal wall distensibility, and progressive aortic regurgitation.15 However, in a multicenter study16 of 474 adults with Tetralogy of Fallot, although nearly a third of the patients had an aortic root diameter≥40mm, the prevalence of an observed-to-expected aortic root dimension ratio>1.5 was only 6.6%, and the prevalence of moderate or severe aortic regurgitation was only 3.5%.
Fontan CirculationPatients born with a single functional ventricle can be treated using palliative techniques such as total cavopulmonary connection with intracardiac tunnel or extracardiac conduit. These procedures are the result of successive modifications of the original Fontan procedure or atriopulmonary connection, and attempt to prevent overpressure, progressive right atrial dilatation, and its associated complications: energy loss and antegrade flow, atrial arrhythmias, stasis, thromboembolic events, etc. However, despite more than 40 years of experience, uncertainty continues to surround this technique.
A key element is patient selection. The 10 criteria published in 1977 by Choussat et al17 have been modified and reduced over the years, and variations in the application of some of these criteria have been reported by different surgical teams. In any case, in a retrospective study of 32 patients undergoing Fontan surgery between 2000 and 2009, Mendoza et al18 suggested that elevated pulmonary arterial pressure remains an excellent predictor of postoperative complications and late mortality. In contrast to other studies that have queried the need for catheterization before the Fontan procedure and suggested its replacement by other imaging techniques (echocardiography and CMR), these authors support its use, emphasizing its value in identifying high-risk patients to whom other measures can be applied such as drug regimens (pulmonary vasodilators) or specific surgical interventions (Fontan fenestration), while drawing attention to its therapeutic potential in the embolization of possible fistulas or abnormal connections. In fact, the techniques are not mutually exclusive and the information provided by the CMR may be relevant. For example, given the remaining doubt concerning the need to embolize some systemic-to-pulmonary collaterals, CMR can effectively quantify flow in these collaterals, thereby helping to identify preoperative risk factors and determine their influence on postoperative outcomes.19
In many centers, fenestration of the Fontan circuit is commonly performed in patients identified during the preoperative procedure as being at high risk. However, its subsequent closure is required and can be done percutaneously, as confirmed by Santiesteban et al,20 who performed fenestration closure in 14 patients undergoing an extracardiac Fontan procedure.
NEW DEVELOPMENTS IN CLINICAL CARDIOLOGYFamilial Heart DiseaseThe European Society of Cardiology working group has published a study outlining a clinical approach to the correct diagnosis of cardiomyopathies,21 based on the recognition of red-flag alerts, whether clinical, electrocardiographic, or imaging tests, and including recommendations on the rational use of certain tests, such as complete biochemical, histological, and molecular analysis.
A study that sequenced titin22 in 312 patients with dilated cardiomyopathy and 231 patients with hypertrophic cardiomyopathy found 72 titin mutations (27% in patients with dilated cardiomyopathy and 1% in patients with hypertrophic cardiomyopathy). The authors concluded that, although these mutations did not predict a poor outcome, they are the most common known cause of dilated cardiomyopathy and suggested the incorporation of this sequencing approach into routine genetic testing.
Regarding SD, a descriptive study conducted in Spain of 168 sports-related deaths23 showed that SD predominantly occurred in men (163) and was related to cycling (29%) and playing football (25%). The main cause was congenital heart disease (50%) in those aged between 9 years and 69 years, and cardiomyopathies were more frequent in those younger than 35 years.
An update24 on cardiac amyloidosis focused on the inherited form, whose most common variant is caused by mutations in the transthyretin gene. The correct identification of patients with this variant is crucial, as it affects the diagnostic approach and treatment decisions and is of importance to genetic relatives.24 Another study25 investigated the diagnostic accuracy of 99mTc-DPD (99mTc-3.3-diphosphono-1.2-propanodicarboxylic acid) scintigraphy in differentiating between monoclonal immunoglobulin light chain and transthyretin-related cardiac amyloidosis. The study evaluated 19 patients and concluded that 99mTc-DPD scintigraphy is a useful test for their differential diagnosis: a scintigram showing intense cardiac uptake in both ventricles indicates a diagnosis of transthyretin-related cardiac amyloidosis, whereas a negative scintigram rules it out.
Surface ElectrocardiographyA common problem in emergency departments is the differentiation between early repolarization and ST-segment elevation acute coronary syndrome (ACS). Smith et al26 studied 355 patients with ST-segment elevation ACS and 171 with early repolarization. They derived an equation based on 3 measurements: R-wave amplitude in lead V4, ST-segment elevation 60ms after J-point in lead V3, and QTc. If the value of the equation was greater than 23.4, overall sensitivity was 86% and specificity was 91%. The presence of an early repolarization pattern has recently been associated with increased cardiovascular mortality and idiopathic ventricular fibrillation. Rollin et al27 studied 1161 patients, of whom 13.3% had an early repolarization pattern; 2.1% died from cardiovascular causes during a follow-up of 14 years. On electrocardiogram, the malignant form of the early repolarization pattern showed notching at the end of the QRS interval and horizontal or descendant ST-segments.
The differential diagnosis of myopericarditis and ST-segment elevation ACS is a common procedure in emergency departments. Porela et al28 showed that PR-segment depression in both precordial leads and limb leads has high positive (96.7%) and negative (90%) predictive power to diagnose myopericarditis.
Changes in the ST-segment in lead aVR in ACS have become a recent focus of attention. In the case of ST-segment elevation ACS, this lead can show ST-segment elevation or reciprocal ST-segment depression (mirror image). Wong et al29 studied changes in aVR in 15315 patients. ST-segment elevation in lead aVR >1 mm was associated with higher 30-day mortality for both anterior and inferior infarction.
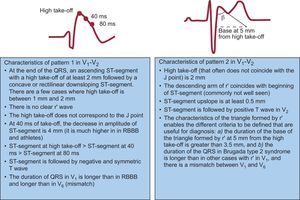
Bayés de Luna et al30 reviewed the electrocardiographic criteria for the diagnosis of Brugada syndrome. In the new electrocardiographic criteria, only 2 patterns are considered (Figure). The article also describes the key points for the differential diagnosis of other conditions, especially right bundle-branch block, athlete's heart, pectus excavatum, and arrhythmogenic right ventricular cardiomyopathy.
Electrocardiographic patterns of Brugada syndrome in V1-V2. RBBB: right bundle branch block bundle. Adapted from Bayes de Luna et al30 with permission.
A study31 assessed trends in awareness of cardiovascular disease risk among 2432 women between 1997 and 2012. The results showed that the rate of awareness of cardiovascular disease as the leading cause of death nearly doubled in this period (30% vs 56%; P<.001), although the results differed when analyzed by race. The rate among black and Hispanic women was 36% and 34%, respectively, similar to that of white women in 1997. Also in 1997, women cited cancer as the leading cause of death and only a third were aware of cardiovascular disease as a leading cause of death, but in 2012 the trend reversed.
Valvular Heart DiseaseSeveral recent studies have been published on diagnosis and prognosis in the field of valvular heart disease. Melis et al32 have drawn attention to the importance of the analysis of aortic flow by Doppler echocardiography in risk stratification of patients with severe aortic stenosis and normal ejection fraction. The analysis of aortic flow, aortic valve area, and aortic pressure gradient were of prognostic value: patients with low-flow aortic stenosis had higher mortality regardless of the aortic gradient. The majority of patients with an aortic valve area>0.8cm2, aortic gradient<40mmHg, and normal flow had a similar prognosis to that of patients with moderate aortic stenosis, whereas patients with an aortic valve area<0.8cm2, aortic gradient<40mmHg, and low flow had a worse prognosis.
The DEcIDE AVR Research Team33 performed follow-up of patients aged 65 years to 80 years undergoing aortic valve replacement with a biological (n=24 410) or mechanical (n=14 789) prosthesis between 1991 and 1999. The researchers concluded that among patients undergoing aortic valve replacement, the long-term mortality rates were similar for those who received biological prostheses vs mechanical prostheses.
In a recent study, Zilberszac et al34 included asymptomatic patients with stenosis and at least moderate aortic regurgitation and preserved left ventricular ejection fraction. During follow-up, 50 patients needed valve surgery, 33 due to symptoms, 3 due to symptoms revealed during stress testing, and 5 due to the rapid progression of aortic stenosis. Event-free survival was 82%(5%), 62%(6%), 49%(6%), 33%(6%), and 19%(5%) at 1, 2, 3, 4, and 6 years, respectively. Multivariate analysis showed that peak aortic jet velocity and concomitant coronary heart disease independently predicted event-free survival.
In the field of transcatheter aortic valve implantation (TAVI), the PRAGMATIC study directly compared the two leading CoreValve and Edwards-SAPIEN devices. After propensity score adjustment, at 30 days there were no differences in all-cause mortality and cardiovascular mortality. Finally, a cost-effectiveness study35 of the PARTNER trial showed that cumulative 12-month costs and quality-adjusted life-years were similar in both treatment arms (transfemoral and transapical TAVI vs aortic valve replacement surgery), despite the procedure-related costs being higher in the TAVI arm ($36 652 [$4703] vs $14 475 [$2612]). However, the costs were slightly lower and quality-adjusted life-years were slightly higher in the transfemoral TAVI cohort than in patients undergoing aortic valve replacement surgery. In the transapical TAVI cohort, 12-month costs remained substantially higher than in the cohort undergoing aortic valve replacement with cardiopulmonary bypass. Furthermore, quality-adjusted life-years were lower in the transapical TAVI cohort than in the conventional surgery cohort.
Aortic DiseaseAn interdisciplinary expert consensus document on the management of type B aortic dissection36 has recently been published, presenting a meta-analysis of 63 studies involving 1548 medically treated patients, 1706 who underwent open surgery, and 3457 who underwent thoracic endovascular therapy. The study suggests that patients with uncomplicated acute or subacute dissection should receive medical treatment, whereas the majority of patients with chronic dissection should receive initial conservative treatment and have their blood pressure closely monitored.
The American Society of Thoracic Surgeons clinical practice guidelines37 on the management and treatment of aortic valve and ascending aorta disease provide a comprehensive overview of aortic valve, aortic root, and ascending aorta disease, distinguishing aortic valve disease from the other valvular heart diseases. This new perspective is reasonable given the close clinicopathological relationship and frequent association of aortic diseases with aortic valve diseases.
DEVELOPMENTS IN HEART FAILURE AND TRANSPLANTATIONAcute Heart FailureThe main developments in the management of acute heart failure (HF) are based on 2 recently published clinical trials: RELAX-HF and CARRESS. The RELAX-HF study compared the efficacy and safety of serelaxin in a randomized, placebo-controlled trial in patients admitted for acute decompensated HF. Intravenous infusion of serelaxin for 48h was associated with dyspnea relief at 5 days, but had no effect on other clinical outcomes such as rehospitalization for HF. Other results included a significant reduction in cardiovascular mortality and total mortality at 180 days, although the latter was a secondary objective because the study design did not permit prognostic comparisons.38 In a substudy of the RELAX-HF trial, Metra et al showed that at day 2 of intravenous serelaxin improvements in biomarkers of cardiac (high-sensitivity cardiac troponin T), renal (creatinine and cystatin-C), and hepatic (aspartate transaminase and alanine transaminase) damage and of decongestion N-terminal pro-brain natriuretic peptide were associated with 180-day mortality.39 Serelaxin had a similarly positive effect in all the subgroups analyzed, due to the rapid relief of congestion and multiorgan protection.
The CARRESS study was a randomized, open, phase-III trial to compare the efficacy and safety of ultrafiltration vs a stepped pharmacologic-therapy algorithm with the aim of improving renal function and reducing fluid volume in hospitalized patients with acute decompensated HF and cardiorenal syndrome. The study found that pharmacologic therapy was superior to ultrafiltration for the preservation of renal function at 96h, with a similar weight loss and lower rate of adverse effects at 60 days.40 The authors found that the patients had a worse clinical profile than patients described in previous studies and that the duration of ultrafiltration was longer than in other trials, possibly contributing to more fluid loss, and hence worsened renal function.
Regarding the non-pharmacologic management of acute decompensated HF, a study by Aliti et al41 randomized 75 acute decompensated HF patients to an aggressive sodium-restricted and water-restricted diet or a diet with no restrictions. Aggressive water and sodium restriction had no effect on clinical outcomes and significantly increased the perception of thirst.
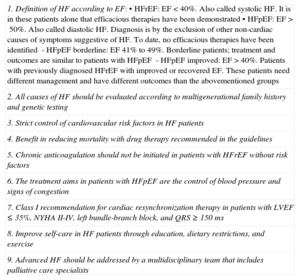
Chronic Heart FailureThis year, new guidelines42 were published by the American College of Cardiology Foundation and the American Heart Association with important developments in both format and content (see Table).
Key Aspects of the 2013 American College of Cardiology Foundation/American Heart Association Clinical Practice Guidelines on the Diagnosis and Management of Acute Heart Failure42
| 1. Definition of HF according to EF:• HFrEF: EF<40%. Also called systolic HF. It is in these patients alone that efficacious therapies have been demonstrated• HFpEF: EF>50%. Also called diastolic HF. Diagnosis is by the exclusion of other non-cardiac causes of symptoms suggestive of HF. To date, no efficacious therapies have been identified- HFpEF borderline: EF 41% to 49%. Borderline patients; treatment and outcomes are similar to patients with HFpEF- HFpEF improved: EF>40%. Patients with previously diagnosed HFrEF with improved or recovered EF. These patients need different management and have different outcomes than the abovementioned groups |
| 2. All causes of HF should be evaluated according to multigenerational family history and genetic testing |
| 3. Strict control of cardiovascular risk factors in HF patients |
| 4. Benefit in reducing mortality with drug therapy recommended in the guidelines |
| 5. Chronic anticoagulation should not be initiated in patients with HFrEF without risk factors |
| 6. The treatment aims in patients with HFpEF are the control of blood pressure and signs of congestion |
| 7. Class I recommendation for cardiac resynchronization therapy in patients with LVEF ≤35%, NYHA II-IV, left bundle-branch block, and QRS≥150ms |
| 8. Improve self-care in HF patients through education, dietary restrictions, and exercise |
| 9. Advanced HF should be addressed by a multidisciplinary team that includes palliative care specialists |
EF, ejection fraction; HF, heart failure; HFpEF, heart failure with preserved ejection fraction; HFrEF, heart failure with reduced ejection fraction; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association functional class.
New developments continue to take place regarding the role of anemia and iron deficiency in HF patients. Klip et al43 studied iron deficiency (defined as a ferritin level<100μg/L or ferritin 100μg to 299μg/L with a transferrin saturation<20%) in 1506 chronic HF patients. Iron deficiency was present in 50% of patients, relates to the severity of HF, and has even greater predictive power than anemia. Apart from its prognostic impact, evidence suggests that health-related quality of life is improved by iron replacement therapy in chronic HF patients with iron deficiency.44 In contrast, the RED-HF study investigated treatment with darbepoetin alpha. Despite improvements in hemoglobin levels, darbepoetin alpha had no effect on morbidity and mortality in patients with HF and depressed systolic function.45.
New data from a recently published subanalysis of the SHIFT study demonstrated the safety and efficacy (morbidity and mortality and readmissions for HF) of treatment with ivabradine in different patient populations: advanced age, left bundle branch block, renal failure, or chronic bronchitis.46
In HF patients with preserved systolic function, initial findings suggest that the use of drugs that act specifically on pulmonary vascular resistance leads to hemodynamic improvement.47 However, the recent report from the RELAX study has generated further debate on this topic. The RELAX study included 113 patients in New York Heart Association class II-III with left ventricular ejection fraction>50% receiving sildenafil 20mg 3 times daily for 3 months, followed by 60mg 3 times daily for 3 months. Compared with the placebo group (n=103), there was no improvement in exercise capacity or other clinical status.48
In assessing the risk and prognosis of HF patients, the use of new biomarkers (multimarker strategy) might be the most efficacious and accurate approach. These include biomarkers of myocardial stretch, such as N-terminal pro-brain natriuretic peptide, biomarkers of myocardial necrosis, such as hs-cTnT (high-sensitivity troponin), and biomarkers of fibrosis/remodeling, such as ST2.49 According to the study by Lupón et al, the added prognostic value of these biomarkers has been shown to be useful in predicting events in HF patients, although the addition of N-terminal pro-brain natriuretic peptide to the new generation of biomarkers (hs-cTNT and ST2) had a limited effect on risk stratification in a cohort of 876 chronic HF patients.50
Advanced Heart Failure and Cardiac TransplantationThe final 12-month results of the controversial IABP-SHOCK II51 study have recently been published. This trial randomized 600 patients with acute myocardial infarction complicated by cardiogenic shock and undergoing optimum medical therapy to receive intra-aortic balloon counterpulsation vs control. Of the 595 patients who completed 12-month follow-up, 155 (52%) of 299 patients in the intra-aortic balloon counterpulsation group and 152 (51%) of the 296 patients in the control group had died (relative risk=1.01; 95% confidence interval, 0.86-1.18; P=.91). There were no differences in other secondary endpoints, such as the rate of reinfarction, need for revascularization, or quality-of-life measures.
The use of left ventricular assist devices (also known as destination therapy) as a bridge to heart transplantation has grown significantly in recent years, but is especially indicated in patients with advanced or refractory HF. The most recent INTERMACS registry included more than 6000 patients and updated the risk factors for continuous flow pumps (Heart Mate II® and Heart Ware®)), showing actuarial survival of 80% at 1 year and 70% at 2 years.52 The 2013 International Society for Heart and Lung Transplantation guidelines for mechanical circulatory support were also published in 201353
The most important topic of debate in cardiac transplantation has been cardiac antibody-mediated rejection (AMR) or humoral rejection. There are no evidence-based management guidelines for AMR in heart transplantation. A survey published in 2013 evaluated international practice for the management of AMR based on the International Society for Heart and Lung Transplantation classification of AMR (pAMR 0-3), the presence of donor-specific antibodies, and allograft function. The different treatments used in AMR were of particular interest: intravenous steroids, intravenous immunoglobulin, plasmapheresis, rituximab, and thymoglobulin.54
CONFLICTS OF INTERESTNone declared.