To the Editor,
Steinert's disease is the most common muscular dystrophy in adults.1 It is an autosomal dominant disease that mainly affects the neuromuscular system. A heart condition is common and is mainly due to degeneration in the conducting tissue. Therefore, arrhythmias are often the first manifestation of the disease2 and can occur in 50% of patients.2-4 We describe the case of a patient with Steinert's disease after an episode of recovered cardiac arrest secondary to syncopal ventricular tachycardia (VT).
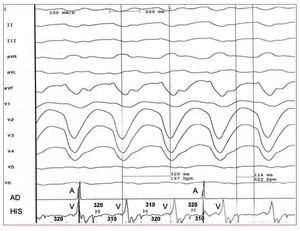
A 33-year-old woman had a sudden episode of retrosternal tightness and palpitations followed by syncope. In Emergency Unit, a heart rate of 220 beats/min was recorded and the electrocardiogram (ECG) showed regular broad QRS tachycardia (160 ms), morphology of left bundle branch block (LBBB) and right superior QRS axis (Figure 1). A few minutes later she went into cardiorespiratory arrest and ventricular fibrillation (VF) was documented, which was reversed with defibrillation at 200 J. The subsequent ECG showed atrial flutter with variable conduction. Analytical and physical examinations showed no abnormalities. The echocardiogram showed a slightly dilated left ventricle with biventricular general hypokinesia (ejection fraction, 42%). The electrophysiological study showed an atrial flutter with cavotricuspid isthmus-dependent counterclockwise activation, and ablation was performed. Baseline intervals in sinus rhythm showed a diffuse (AH, 151 ms; HV, 104 ms) conduction disorder, predominantly an infrahisian conduction disease. The right ventricular pacing (cycle 500 ms and extra stimulus 240 ms) triggered a well-tolerated sustained monomorphic VT with a cycle length of 320 ms (187 beats/min) and LBBB morphology with right superior axis. It was shown to be a bundle-branch reentry VT (Figure 2). Given the history of syncopal VT that degenerated into VF, a dual chamber defibrillator was implanted and ablation of the right bundle branch was performed. Subsequent thorough neurological examination of the patient revealed a facial weakness with myotonia in the tongue and impaired muscle relaxation in the distal extremities. An electromyogram was performed, which showed abundant myotonic activity. A genetic study confirmed the diagnosis of myotonic dystrophy type 1. The patient was discharged and after 24 months of follow up is asymptomatic.
Figure 1. Regular tachycardia at admission, at 220 beats/min, broad QRS (160 ms), with morphology of left bundle branch block and right superior QRS axis.
Figure 2. Surface electrocardiogram and intracardiac electrograms of ventricular tachycardia induced during electrophysio-logical study. The characteristics of re-entry between the branches are: QRS morphology of left bundle branch block (due to orthodromic activation of the right bundle branch) atrioventricular dissociation during tachycardia, and a prolonged HV interval greater than the baseline, H before each QRS tachycardia and HH changes precede the changes in the VV. HH intervals are shown in the bottom and VV in the His upper register.
The gene causing Steinert's disease contains an unstable enlargement of the cytosine-thymineguanine trinucleotide.3 This disease mainly affects the neuromuscular system, but may affect other systems. The heart condition consists of a diffuse degeneration of the conducting tissue; the myocardium is affected less frequently. Arrhythmias are often the first cardiac manifestation of the disease and can occur in 50% of patients. Sinus bradycardia, atrioventricular block, atrial fibrillation and flutter and ventricular tachycardia and fibrillation have been reported.2-4
The findings of the clinical history, physical examination and electrophysiological study suggested adult type 1 myotonic dystrophy type muscle disease (Steinert's disease). Recently, it has been reported that severe abnormalities of the ECG and atrial tachyarrhythmias are independent predictors of sudden death in Steinert's disease.5
The typical VT mechanism in patients with myotonic muscular dystrophy is bundle-branch reentry,4 facilitated by delayed conduction in the His-Purkinje system. Drug therapy in these patients is poor4 and it has been shown that the ablation of the His bundle branches (usually the right) is the treatment of choice. However, some patients with successful ablation of the right bundle branch and a pacemaker implant die suddenly (probably malignant ventricular arrhythmia), so that the implantation of an automatic defibrillator may be indicated for this type of patient.6