One of the cornerstones of the prevention of cardiovascular diseases is the identification of individuals at higher risk of these conditions. The cardiovascular risk (CVR) factors causing cardiovascular diseases have been investigated in epidemiological studies since the middle of the 20th century. These studies have also tried to determine the strength of the association of each factor with each disease. On the back of these studies, mathematical models were developed to permit the identification of individuals with a greater likelihood of developing, in the more or less near future, a cardiovascular condition.
The best-known epidemiological study and the most lucrative single source of predictive models is known as the Framingham study, named after the town of residence of its participants, in Massachusetts (United States).1 Diverse mathematical models, largely based on Cox proportional hazards regression, enable calculation of absolute CVR, sometimes abbreviated as simply CVR.2,3
When CVR is calculated, the following parameters must be considered: the source population, the cardiovascular event being measured, and time horizon (typically 10 years). These calculations generally use risk evaluation systems based on primary prevention populations, that is, individuals who have not had the cardiovascular event whose risk is being calculated. Some models calculate the probability of a subsequent event, known as secondary prevention, but such an approach is uncommon.4
The cardiovascular event of interest may vary. Although the most commonly used models initially calculated the risk of a coronary event (fatal or nonfatal),2,3 there is also interest in evaluating the absolute (also known as global) risk of a fatal or nonfatal cardiovascular event.5 Fatal CVR (fatal stroke or coronary heart disease) is calculated with the SCORE system.6
Any CVR calculation system obtained from a specific population must be adapted or calibrated before it can be applied to a different population. The Wilson equation3 was derived from the Framingham study but was calibrated for Spain in the REGICOR trial.7 Equations for 10-year fatal CVR were obtained for high- and low-risk countries (Spain was included in the latter group) in the SCORE trial, with more specific calibrations subsequently published for various countries, including Spain.8
One criticism of risk evaluation systems is that they involve the application of a population probability calculation to specific individuals, meaning that some individuals who will develop the cardiovascular event will be overlooked. Accordingly, the sensitivity and specificity, and consequently the positive and negative predictive values, are far from 100%. The models can be slightly improved by including more predictive variables. Other variables, including socioeconomic level, inflammatory markers such as C-reactive protein, and laboratory data such as triglyceride and creatinine levels, to mention just some examples, have been included in different risk evaluation systems without being adapted to Spain. Experts debate which are more effective: complex and exhaustive systems with many variables but higher implementation difficulty or simpler systems with a small loss of predictive capacity but improved ease of use. Regardless, CVR quantification is a step performed in the application of clinical management guidelines.
Therefore, CVR evaluation systems can be used in clinical practice to identify individuals at greater risk of a cardiovascular event who should receive more aggressive therapeutic measures: drug therapy, as well as lifestyle changes, and stricter therapeutic targets.
Most of the common clinical practice guidelines in Europe require risk evaluation because strategies and therapeutic targets depend on the level of risk.9,10 Thus, individuals are classified as low, moderate, high, and very high risk. For example, the European guidelines for dyslipidemia state that individuals with a risk SCORE higher than 10% are at very high risk and should have a low-density lipoprotein cholesterol target of less than 70mg/dL; if the risk is between 5% and 10%, they are considered to be at high risk and their target is 100mg/dL.
Nonetheless, the same guidelines also recognize the limitations of the risk evaluation systems, with one particularly important aspect: young individuals can have an absolute risk that is not high despite having multiple risk factors.9 For example, a 40-year-old Spanish man, active smoker, with blood pressure of 180mmHg and total cholesterol of 320mg/dL, would have a risk SCORE of 2% (moderate). This man would have a coronary risk of 9% with REGICOR. Although his absolute risk is not high, his risk situation is far from acceptable. The possible solutions to this paradoxical situation will be discussed below.
RELATIVE RISKThe first calculable alternative is relative risk, defined as the ratio between the absolute risk of the patient in question and the risk of the ideal situation or of the reference risk factors.
Since 2007, European cardiovascular disease prevention guidelines have supplied a relative risk table to try to solve this problem. According to this table, the relative risk of our patient is 12, considering the ideal situation, in which he does not smoke and has a systolic blood pressure of 120mmHg and cholesterol of 190mg/dL. However, the guidelines fail to clearly define high and very high relative risk, and so we lack operational criteria.
LONG-TERM OR LIFETIME RISKA second alternative involves the use of a time horizon much longer than 10 years in risk calculation.11 Because young adults have life expectancies much longer than 10 years, calculation of the 30-year risk, or even the lifetime risk, would be of greater clinical interest than a restricted 10-year risk. There are no guidelines for the management of CVRs using these scales, and there are no cutoff points to define the distinct risk levels. Accordingly, one simple question still requires an answer: do individuals of a specific age with a higher long-term risk also have a higher short-term risk than their peers?
CARDIOVASCULAR RISK PERCENTILESA third option is CVR percentile.12 The absolute risk can be converted to a risk percentile by using data on the population containing our individual. For the above example of the 40-year-old man with a risk SCORE of 2%, his percentile is above the 90th percentile, meaning that less than 10% of his contemporaries are at higher risk than he is. Thus, even though his absolute risk is not high, surely he warrants especially intensive treatment? Take a different patient. A 65-year-old man with a risk SCORE of 5% (high) has a percentile lower than 40, meaning that more than 60% of his contemporaries have higher risk than he does. Should he be treated as intensively as the guidelines recommend?
These questions should make us reflect on the appropriateness of establishing absolute risk cutoff points to decide whether to implement more intensive treatments. Similarly, cutoff points could be used for the percentiles.
An important advantage of percentiles is their high concordance among the distinct risk evaluation systems. The kappa coefficient values for the agreement among the scales derived from the Framingham study (Wilson, DORICA, REGICOR) for the identification of high absolute risk range from 0.083 to 0.386, whereas the kappa indices of the percentiles are 1. Similar results are obtained when the SCORE system is used for high- and low-risk countries: the concordance among percentiles shows a perfect score.
VASCULAR AGEAnother indicator suitable for patients with CVR factors is vascular age (VA), also known as heart age or CVR age.
A measurement scale for general CVR derived from the Framingham study was published in 2008.5 The same article presented a VA scale based on absolute risk. The VA of a patient with CVR factors is defined as the age that an individual of the same sex as our patient would have if he or she were to have the same absolute risk but controlled risk factors. This approach transforms the absolute risk into another concept more easily understood by patients.
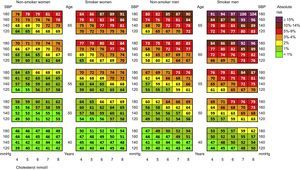
In 2010, VA calculated with the SCORE system13 was published (Figure 1), enabling the absolute risk to be converted into VA. Thus, our example—the 40-year-old male smoker with hypertension and hypercholesterolemia and a risk SCORE of 2% (moderate)—has a VA of 63 years; that is, he has the same probability of dying from a cardiovascular event as a healthy 63-year-old. In other words, if he fails to change his habits and risk factors, he could lose 23 years of cardiovascular life.
Table of vascular age according to the SCORE (Systemic Coronary Risk Estimation) scale for low-risk countries. SBP, systolic blood pressure. Reproduced with the permission of Cuende et al.13
Calculation of VA with the SCORE was included in the European cardiovascular prevention guidelines of 2012 as a tool allowing patients, especially young patients, to better understand their risk, even if their absolute risk is not high.
Because patients with CVR factors are notably asymptomatic during most of the atherosclerotic process, adherence to drug and lifestyle/dietary treatments can be low. This low adherence to the therapies is also discussed in the clinical practice guidelines, with such causes as young age, asymptomatic disease, and confusing, complex, or insufficient advice.9 Thus, use of VA is crucial to better explain the risk situation.
The message of VA is clear and easily understood by patients, and it is not a confusing, abstract, or mathematical concept like absolute risk. Application of VA to young people situates them in a time other than the present. Accordingly, this tool can be used to improve adherence and better communicate risk.
When making therapeutic decisions in the current clinical situation, far from the paternalistic models, patients must accept, understand, and be satisfied with the treatments offered by their physicians, once they have discussed the therapy together.9 It is difficult to make 40-year-old patients understand why their risk SCORE of 2% is alarming. Even if they understand the 2% message, patients might think that they have a 98% probability of surviving the next 10 years. Which is true. But patients will understand their current situation if their physician explains that their heart and arteries are 65 years old, even when their identity card states that they are 40 years old. This message could help patients to improve their adherence to the drug therapy and lifestyle modifications recommended by their physician.
From the point of view of the patient, there are 2 sides to the concept of risk: on the one hand, risk is a mathematical concept that some people fail to understand well while, on the other hand, risk has a personal interpretation that makes the patient be more or less accepting of the risk situation. The acceptance of the risk is lower if the risk (or the situation it causes) is frequent, severe, immediate, involuntary, avoidable, uncontrollable, new, catastrophic, or caused by humans. In contrast, the acceptance of the risk is higher if it is infrequent, mild, delayed, voluntary, unavoidable, controllable, familiar, daily, or natural.14 The CVR has many components favoring greater patient acceptance: a time delay, its control depends on the patient's willpower, and it is controllable, familiar, daily, and natural.
In summary, patients fail to understand the concept of risk and, even if they understand it, are highly accepting of their own risk situation. A recommendation included in the management guidelines of CVR factors is that approaches should be developed that permit a better understanding of risk in order to better communicate the message and achieve better treatment adherence and reduced acceptance of the risk situation. Accordingly, the concept of VA is an ideal tool for achieving these objectives because it converts an abstract concept into a perfectly understandable message.
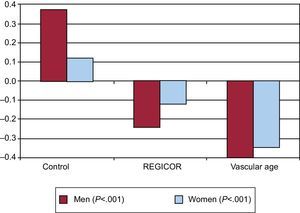
Despite these considerations, we may still wonder if the message of VA really enables better risk factor control. Recently, a randomized clinical trial of 3000 individuals compared 3 different strategies: standard clinical care with no information on vascular risk or VA (control group), clinical care with information on the individual's absolute risk, and clinical care with information on the individual's VA.15 The change in risk factors was evaluated after 12 months: body mass index, waist circumference, smoking status, physical activity, blood pressure, lipid profile, and glycemia. All factors except physical activity were worse in the control group. The group showing the greatest improvement (which was statistically significant) in all risk factors was the group informed about VA, who showed the largest decrease in their CVR (Figure 2). The results of this study should compel us to treat our patients by informing them about their risk and VA.
Change in the vascular risk according to the information received by the patients. REGICOR, Registre Gironí del Cor. Graph created by using data from López-González et al.15
Finally, a different view of cardiovascular prevention can be considered. The current guidelines set out targets and therapeutic approaches based on specific absolute risk cutoffs, an approach that is partly motivated by cost-effectiveness: individuals with higher risk are those who can benefit most from risk reduction. In other words, considering the same relative risk reduction, the higher the initial risk, the lower the number of individuals needed to avoid a cardiovascular event, that is, fewer patients require treatment. Several questions can nonetheless be posed: How many years are patients willing to lose before accepting the proposed treatments? How many years can be gained if the treatments are followed? How much does each year of VA cost? Lastly, does it cost the same at different ages?
CONFLICTS OF INTERESTNone declared.