Keywords
INTRODUCTION
Although common AV nodal reentrant tachycardia (AVNRT) typically occurs in patients with dual anterograde AV nodal physiology, many of these patients do not fulfill classical criteria for dual AV nodal pathways during programmed atrial stimulation.1-3 It is thought that there is dual AV nodal conduction during incremental atrial pacing when the interval from the atrial stimulus to the conducted QRS complex is greater than the pacing interval during stable 1:1 atrioventricular (AV) conduction.4 This finding also predicts the induction of AVNRT and could be useful in evaluating the effectiveness of perinodal slow pathway ablation.5
Our study prospectively evaluated the usefulness of incremental atrial pacing to assess the effect of radiofrequency catheter ablation on perinodal slow pathway conduction in patients with AVNRT.
METHODS
Patients
The characteristics of anterograde AV node conduction were evaluated in consecutive patients, in sinus rhythm, referred for electrophysiological study with or without final induction of AVNRT (AVNRT and control groups, respectively).
Electrophysiological Study
The diagnostic electrophysiological study and catheter ablation procedure were done in the same session, patients having given written informed consent; the patient fasted during the study and antiarrhythmic agents were previously suspended for at least 5 half-lives. Intravenous propofol was used for sedation. Two quadripolar catheters were introduced into the right ventricular apex (4 Fr) and right atrium (6 Fr) via the right femoral vein; the latter was progressed toward the area of the bundle of His during the study for baseline recording and during tachycardia; a third catheter was placed in the coronary sinus when necessary. Standard electrocardiographic leads and intracavitary ECG bipolar recordings of the right atrium and right ventricular apex were digitally recorded at a sampling frequency of 1 kHz and stored on optical disk. The recordings were analyzed at a paper speed of 200 mm/s.
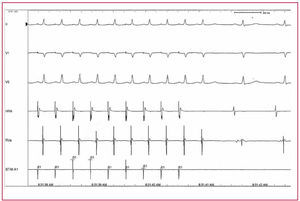
Pacing from the right atrium was done at a 2-ms pulse width and dual threshold voltage using a programmable stimulator (UHS 20, Biotronik. Berlin, Germany). The PR interval was measured from the pacing spike to the beginning of the conducted QRS complex. Incremental atrial pacing was done by decreasing the pacing cycle length of 10 by 10 ms every 10-15 stimuli until a stable PR interval greater than the RR interval (10 consecutive cycles) (Figure) was obtained or AV nodal block occurred. Stable 1:1 conduction with PR>RR interval indicates the presence of anterograde perinodal slow pathway conduction.5 Programmed atrial stimulation was done with an extrastimulus and two basic drive cycle lengths of 600 and 400 ms. The extrastimulus coupling interval was shortened by 10 ms in each drive-train stimulus until AV conduction block occurred or the refractory atrial period was reached.
Figure 1. Atrial stimulation with CL 330 ms showing PR>RR interval. From top to bottom: electrocardiographic leads DII, V1, and V5, intracavitary recordings of right atrium (HRA) and right ventricle (RVa), and stimulation channel (STIM A1).
The intervals were measured with online calipers at a recording speed of 200 mm/s. During programmed atrial stimulation we defined the presence of dual AV nodal pathway as an increase in the A2H2 interval ≥50 ms in response to a 10-ms decrement in the A1A21 coupling interval. After the initial study, intravenous isoprenaline was administered, when necessary, to induce sustained AVNRT (initial dose 0.4 µg/min, raising this, when needed, to increase the initial heart rate by up to 30%-40%). Common AV nodal reentrant tachycardia was diagnosed according to standard criteria.6 Radiofrequency catheter ablation of the perinodal slow pathway was done, starting in the inferoseptal area and the catheter moved to upper positions in case of failure; electrograms showed an AV relationship <0.57. The aim of the ablation was complete elimination of slow pathway conduction or significant modification (persistence up to a single AV nodal echo beat); thus, when we speak about successful slow pathway ablation we refer both to its complete elimination and its modulation. In the AVNRT group, measures were done before ablation and 30 min after successful radiofrequency catheter ablation. Isoprenaline was administered after ablation only when it was initially necessary to induce tachycardia. Thus, the postablation study was done under the same conditions in those patients who only presented an AH jump or PR>RR interval during infusion of isoprenaline. Measurements were only taken in the control group during the initial diagnostic study; isoprenaline was only used in the patients with atrial tachycardia in this group.
Statistical Analysis
Continuous variables were expressed as mean (standard deviation [SD]) and compared using the Student t test. Discrete variables were compared using the Fisher exact test. A P value less than .05 was considered significant.
RESULTS
The AVNRT group included 52 females and 33 males, with an age of 49 (15) years. Nodal reentrant tachycardia was not induced in 60 patients. Of these, 56 were included in the control group, 19 females and 37 males, with an age of 45 (19) years; 4 patients admitted due to palpitations with negative electrophysiological study were excluded from the analysis. There were 21 patients with accessory pathways in this group, 14 with atrial flutter, 3 with atrial tachycardia, 3 with ventricular tachycardia, 4 with Brugada syndrome, 1 patient with depressed ejection fraction and unsustained ventricular tachycardia, 1 with atrial fibrillation, and 9 with syncope with suspected infra-Hisian block or ventricular tachycardia as causes. There were more females in the AVNRT group than in the control group (61% vs 34%; P<.01).
Initial Electrophysiological Study
AVNRT Group (Table 1)
During programmed atrial stimulation, 52 patients (61%) presented dual nodal physiology, 5 of them during isoprenaline infusion. Incremental atrial pacing yielded sustained 1:1 conduction with PR>RR interval in 66 patients (78%), five of them during isoprenaline infusion. Only 10/85 (11.8%) patients presented evidence of slow pathway conduction during isoprenaline infusion. Nodal reentrant tachycardia was induced in 57/85 (67%) in the baseline study and in 28/85 (33%) during isoprenaline infusion. The AVNRT cycle length was shorter in patients with PR>RR interval during incremental atrial pacing (357 [51] vs 394 [51] ms; P<.01), with no significant differences between those with or without AH jump (372.2 [51.3] vs 354.7 [55.8] ms). The maximum PR interval was longer in patients with PR>RR interval than in those who did not present this (427 [64] vs 371 [83]; P<.05); there were no differences in the Wenckebach point (375 [47] vs 378 [94]) between the 2 groups. No significant relationship was found between the presence of dual nodal physiology during programmed stimulation and sustained conduction with PR>RR interval during incremental pacing.
Control Group (Table 2)
During programmed atrial stimulation, 10 patients (18%) presented dual nodal physiology. Incremental pacing demonstrated sustained 1:1 conduction with PR>RR in 7 patients (12%).
Thus, regarding induced AVNRT, the finding of sustained 1:1 conduction with PR>RR interval during incremental atrial pacing had a sensitivity of 78%, specificity 88%, positive predictive value 90%, and negative predictive value 72%, while the values for the finding of dual nodal physiology during programmed atrial stimulation were 61%, 82%, 84%, and 58%, respectively.
Atrial Stimulation After Slow Pathway Conduction Ablation
Successful slow pathway ablation conduction was achieved in 81/85 patients, complete elimination of conduction in 44/81 and modification up to a single AV nodal echo beat in 37/81. In the study done 30 min after successful ablation, an absence of sustained 1:1 conduction with PR>RR interval was found in 65 of the 66 patients who presented this in the initial study, despite the persistence of signs of dual nodal physiology during programmed stimulation in 37 of the 81 patients. Table 3 shows the result of incremental atrial pacing before and after ablation in those patients who presented PR>RR in the initial study. Induced AVNRT persisted in 4/85 patients at the end of the procedure (AH jump persisted in all four and sustained 1:1 conduction with PR>RR in 3/4). No patient without PR>RR preablation presented such a phenomenon postablation.
The positive predictive value of the absence of 1:1 conduction with PR>RR interval during incremental atrial pacing for successful slow pathway ablation was 98%.
DISCUSSION
Our study demonstrates the usefulness of incremental atrial pacing for evaluating the effectiveness of slow pathway conduction ablation, both when completely eliminating its capacity for conduction and when significantly modifying this (up to a single AV nodal echo beat). Incremental pacing has good sensitivity and specificity in predicting the inducibility of AVNRT during an electrophysiological study and is, in addition, a simple and rapid method for evaluating the effect of radiofrequency catheter ablation on slow pathway conduction in patients with this tachycardia.
As most patients with inducible AVNRT present stable conduction with a PR>RR interval, this method is widely applicable to this population.
Sustained slow pathway conduction during atrial stimulation was initially described by Rosen et al8 and subsequently, Wu et al4 found that this property could be demonstrated in 70% of patients with nodal reentrant tachycardia. The study by Baker et al5 included selected patients with AVNRT (by definition, one group with and one group without dual nodal physiology during programmed atrial stimulation), and patients with accessory pathway ablation located far from the AV node as the control group. In this study, the sensibility, specificity and positive, and negative predictive values of the finding of a PR interval greater than the atrial pacing cycle length to induce AVNRT were 93%, 89%, 90%, and 92%, respectively. We found lower sensitivity (78% vs 93%) and negative predictive values (72% vs 92%). The greater diagnostic spectrum in our control group and the use of a different sedation protocol could explain these differences. On the other hand, the same study,5 with the aim of completely eliminating slow pathway conduction via ablation, did not find any case of sustained conduction with PR>RR interval in the 28 patients with successful slow pathway ablation. However, the complete elimination of slow pathway conduction may not be necessary to achieve clinical success, and the persistence of residual slow pathway conduction can also be accepted as an aim up to a single AV nodal echo beat.9 The sensitivity of this criterion has not been described when implemented as the aim of ablation. We used this in our study and conduction with PR>RR interval was only maintained in 1/66 patients after slow pathway ablation. Successful ablation eliminated the sustained slow pathway conduction needed for AVNRT to develop in 37/81 patients, despite the persistence of dual nodal physiology during programmed atrial stimulation. Thus, the absence of sustained slow pathway conduction during incremental atrial pacing can be used for evaluating the effectiveness of radiofrequency catheter ablation in patients with AVNRT undergoing slow pathway ablation. Ablation/modification of the slow pathway is a safe procedure which achieves good results in treating nodal reentrant tachycardia.10 Our results show that incremental atrial pacing can be used in patients with dual anterograde AV nodal physiology during programmed stimulation as a simple method for evaluating the effect of radiofrequency catheter ablation. In patients who do not show dual AV nodal physiology during programmed stimulation, the absence of sustained slow pathway conduction during incremental atrial pacing would be the only practical method, in addition to tachycardia induction, to evaluate the effect of slow pathway ablation. Furthermore, in our population of patients with AVNRT, 1:1 AV conduction with PR>RR interval during incremental pacing was observed more frequently than AH jump with programmed stimulation. The fact that most of our patients were sedated with propofol can account for the low incidence of AH jump during programmed atrial stimulation.3 Another possible practical application of this finding would be in patients with documented electrocardiographic evidence of supraventricular tachycardia with suspected nodal reentry where only a dual nodal pathway is documented, without tachycardia induction (or with unreplicable induction). Slow pathway ablation is accepted as treatment in these cases and the objective is the presence of rapid nodal rhythm during the application or the complete elimination of slow pathway conduction.11-12 If these patients present PR>RR interval during the initial study, it could be simpler to use the absence of this event as a postablation objective.
The AVNRT cycle length was smaller in patients with PR>RR interval. Incremental atrial pacing, sustained, and at an increasing frequency, could promote a greater increase in sympathetic tone than programmed stimulation, thus accounting for the fact that the cycle length of the tachycardia induced with this stimulation protocol was shorter.
Study Limitations
In the AVNRT group, the proportion of females was greater than in the control group, but this is characteristic of this arrhythmia.13 We did not study the effect of autonomic stimulation (eg, isoprenaline) on these findings. Given that there were preferential atrial conduction pathways toward the AV node, the stimulation site could modify these results, and thus they may not be applicable to other stimulation points (eg, the coronary sinus). Most of the patients were sedated with propofol; this drug could influence the outcome of atrial stimulation, reducing the capacity to demonstrate dual nodal physiology and the possibility of inducing AVNRT. In a recent study by Heidbüchel et al,3 which included 344 patients with AVNRT and also employed propofol, only 41% were inducible without isoprenaline. We did not make a prospective comparison of the various criteria for effective ablation after each radiofrequency energy application, and thus cannot ensure that the absence of sustained conduction with PR>RR interval precedes the suppression of induced sustained tachycardia or not.
CONCLUSIONS
Stable 1:1 AV conduction with a PR>RR interval is obtained with incremental atrial pacing in most patients with inducible AV nodal reentrant tachycardia. This stimulation protocol can be used as a rapid and simple method for evaluating the effect of radiofrequency ablation on slow pathway conduction.
ABBREVIATIONS
AV: atrioventricular
AVNRT: common AV nodal reentrant tachycardia
See editorial on pages 7-9
Correspondence: Dr. J. Martínez Sánchez.
San Nicolás, 27, 1.° B. 30005 Murcia. España.
E-mail: juanmsmur@secardiologia.es
Received March 31, 2006.
Accepted for publication October 2, 2006.