This article summarizes the main developments reported in 2014 on ischemic heart disease, together with the most important innovations in intensive cardiac care.
Keywords
According to data from the RECALCAR registry,1 31.2% of the total number of deaths in 2010 in Spain were due to cardiovascular diseases. Nevertheless, Spain has one of the lowest mortality rates for coronary artery disease (CAD) in Europe for both sexes. Recent data indicate that Spanish mortality rates for cardiovascular diseases have dropped 36% in men and 40% in women since the mid-1970s.
This year, results from the DIOCLES2 study have been published for the management and prognosis of acute coronary syndrome (ACS) in Spain. This is part of an ongoing project by the Coronary Artery Disease and Acute Cardiac Care Group to promote periodical ACS registries. These registries provide valuable information about the prognosis and management of ACS over time in our country.3–5 The DIOCLES study included 2557 patients who were hospitalized between January and June, 2012, with suspected ACS in 44 randomly-selected Spanish hospitals. Hospital mortality was 4.1%, which is significantly lower than the rate reported in the latest MASCARA6 registry (5.7%), as seen in the Table.7–28 Among the 1602 patients with non—ST-segment elevation ACS (NSTEACS) included in the registry (62.7% of the total), the use of p2y12 inhibitors increased (from 42%- 91%), the use of glycoprotein IIb/IIIa inhibitors decreased (from 21% to 4%, respectively), and the use of angiography during hospitalization increased (from 63% to 81%) as did percutaneous coronary intervention (PCI) rates (from 34% to 53%). These data confirm the gradual incorporation of clinical practice guideline recommendations in Spain; at the same time, ACS-related in-hospital mortality had significantly decreased.
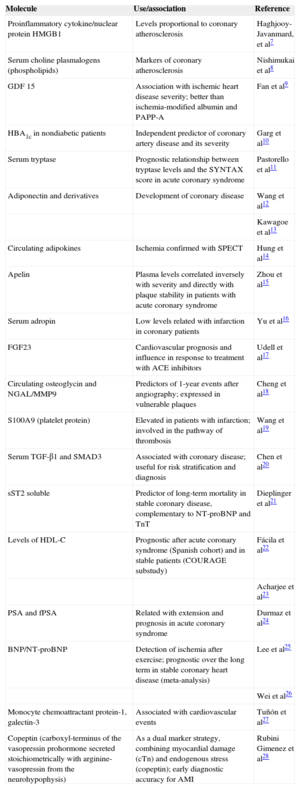
Relevant Molecular Biomarkers in Studies Published in Recent Months
| Molecule | Use/association | Reference |
|---|---|---|
| Proinflammatory cytokine/nuclear protein HMGB1 | Levels proportional to coronary atherosclerosis | Haghjooy-Javanmard, et al7 |
| Serum choline plasmalogens (phospholipids) | Markers of coronary atherosclerosis | Nishimukai et al8 |
| GDF 15 | Association with ischemic heart disease severity; better than ischemia-modified albumin and PAPP-A | Fan et al9 |
| HBA1c in nondiabetic patients | Independent predictor of coronary artery disease and its severity | Garg et al10 |
| Serum tryptase | Prognostic relationship between tryptase levels and the SYNTAX score in acute coronary syndrome | Pastorello et al11 |
| Adiponectin and derivatives | Development of coronary disease | Wang et al12 |
| Kawagoe et al13 | ||
| Circulating adipokines | Ischemia confirmed with SPECT | Hung et al14 |
| Apelin | Plasma levels correlated inversely with severity and directly with plaque stability in patients with acute coronary syndrome | Zhou et al15 |
| Serum adropin | Low levels related with infarction in coronary patients | Yu et al16 |
| FGF23 | Cardiovascular prognosis and influence in response to treatment with ACE inhibitors | Udell et al17 |
| Circulating osteoglycin and NGAL/MMP9 | Predictors of 1-year events after angiography; expressed in vulnerable plaques | Cheng et al18 |
| S100A9 (platelet protein) | Elevated in patients with infarction; involved in the pathway of thrombosis | Wang et al19 |
| Serum TGF-β1 and SMAD3 | Associated with coronary disease; useful for risk stratification and diagnosis | Chen et al20 |
| sST2 soluble | Predictor of long-term mortality in stable coronary disease, complementary to NT-proBNP and TnT | Dieplinger et al21 |
| Levels of HDL-C | Prognostic after acute coronary syndrome (Spanish cohort) and in stable patients (COURAGE substudy) | Fácila et al22 |
| Acharjee et al23 | ||
| PSA and fPSA | Related with extension and prognosis in acute coronary syndrome | Durmaz et al24 |
| BNP/NT-proBNP | Detection of ischemia after exercise; prognostic over the long term in stable coronary heart disease (meta-analysis) | Lee et al25 |
| Wei et al26 | ||
| Monocyte chemoattractant protein-1, galectin-3 | Associated with cardiovascular events | Tuñón et al27 |
| Copeptin (carboxyl-terminus of the vasopressin prohormone secreted stoichiometrically with arginine-vasopressin from the neurohypophysis) | As a dual marker strategy, combining myocardial damage (cTn) and endogenous stress (copeptin); early diagnostic accuracy for AMI | Rubini Gimenez et al28 |
ACE, angiotensin-converting enzyme; AMI, acute myocardial infarction; BNP, brain natriuretic peptide; cTn: cardiac troponin; FGF23, fibroblast growth factor 23; fPSA, free prostate-specific antigen; GDF 15, growth differentiation factor 15; HBA1c, glycated hemoglobin; HDL-C, high-density lipoprotein cholesterol; HMGB1, high-mobility group protein B1; MMP-9, matrix metallopeptidase 9; NGAL, neutrophil gelatinase-associated lipocalin; NT-proBNP, N-terminal pro-brain natriuretic peptide; PAPP-A, pregnancy-associated plasma protein A; PSA, prostate-specific antigen; SMAD3, decapentaplegic homolog 3; SPECT, single-photon emission computed tomography; sST2, soluble suppression of tumorigenicity 2; TGF-β1, transforming growth factor β1; TnT, troponin T.
Interesting data have also been provided by the EURHOBOP registry,29 which shows important differences among European countries in ACS management. The study included 12 231 consecutive ACS patients who had been admitted to hospital from 2008 to 2010 in 7 European countries (Germany, Spain, Finland, France, Greece, Italy, and Portugal). There was a higher prevalence of smokers in Greece, France and Spain, and there were more diabetic patients in Spain and Portugal. In patients with NSTEACS (67.2% of the total), the most notable difference was fewer angiographies and coronary revascularizations in southern European countries: 66.1% in France, 57.4% in Germany, 44.1% in Finland, 37.3% in Spain, 33.4% in Portugal, and 19.6% in Greece. It should be remembered that these data are from 2010 and, as shown by the DIOCLES study data from 2012, these differences have been decreasing in recent years in Spain.
The differences in CAD prognosis according to sex are still controversial. In the recently published RESCATE II study,30 mortality was similar in women and in men 28 days after an initial ACS (5.57% and 4.46%, respectively; P = .39), but 7-year mortality was higher in men (hazard ratio [HR] = 1.93; 95% confidence interval [95%CI], 1.46-2.56; P < .001).
PathogenesisThere is a growing interest in understanding which underlying mechanisms lead to atherosclerotic plaque destabilization and the subsequent appearance of ACS. Local and systemic inflammation play a fundamental role in the pathophysiology of ACS. A related review by Libby et al31 merits attention as it offers a global perspective of the mechanisms by which inflammation can lead to the appearance of ACS. These observations have important potential therapeutic implications for the prevention of ACS and its recurrence.
CARDIOVASCULAR PREVENTIONThe RECALCAR registry1 has demonstrated a high prevalence of classic cardiovascular risk factors in Spain, which is disproportionate with the low incidence of cardiovascular diseases compared with other European countries. A possible explanation for this contrast is that the negative impact on health of some of these risk factors, such as the increasing rates of obesity and diabetes as well as smoking in women, still has not had sufficient time to increase the incidence of cardiovascular diseases.
In the EUROASPIRE (European Action on Secondary Prevention through Intervention to Reduce Events) IV study,32 most patients did not meet the established therapeutic objectives for their risk factors, even though a high percentage of patients with CAD received proper treatment. According to a recent meta-analysis, approximately 9% of cardiovascular events in Europe could be attributed to a low degree of adherence to treatment with statins and antihypertensive medications as there is an inverse association between the degree of adherence and the risk of events.33
The latest data from clinical drug trials have focused on antidiabetic and hypolipidemic agents. Two dipeptidyl peptidase-4 inhibitors, saxagliptin and alogliptin, were tested in the SAVOR-TIMI 5334,35 and EXAMINE36 studies, respectively. Both inhibitors were not inferior to placebo for the appearance of adverse cardiovascular events. Saxagliptin, however, was associated with an increase in hospitalizations due to heart failure (HR = 1.27; 95%CI, 1.07-1.51), especially in patients with elevated levels of natriuretic peptides, a history of heart failure, or chronic kidney failure. Therefore, its use is not recommended in patients with cardiovascular disease.35
Although low high-density lipoprotein cholesterol levels are a powerful independent predictor for cardiovascular risk, recent data suggest that this may not be applicable to high-risk patients treated with statins. When low high-density lipoprotein cholesterol levels were evaluated in patients treated with different statin doses low high-density lipoprotein cholesterol levels were only related to increased cardiovascular risk in those not taking statins or only taking low statin doses, but not in those taking high doses.37 In a recent meta-analysis, high-density lipoprotein cholesterol-targeted drug treatments with niacin, fibrates, and cholesteryl ester transfer protein inhibitors (combined with statins) did not reduce the number of cardiovascular events.38
An important innovation is the publication of the results obtained with PCSK9 inhibitors. These drugs had already been shown to be effective at significantly reducing low-density lipoprotein cholesterol in phase II studies. The reduction was maintained with a 1-year treatment, showing good tolerance to the drug, in the recent OSLER study.39 The results of the LAPLACE-2 study40 have also shown that the combination of evolucumab and a statin significantly reduced low-density lipoprotein cholesterol when compared with a statin plus ezetimibe or a statin alone.
The GAUSS-241 and MENDEL-242 studies evaluated the efficacy of evolucumab in hypercholesterolemic patients with intolerance to statins. In both studies, significant reductions were obtained in low-density lipoprotein cholesterol compared to ezetimibe and placebo, with no increase in adverse effects. Despite promising results, PCSK9 inhibitors will have to demonstrate their superiority over statins in the prevention of cardiovascular events. Lastly, we should not forget that the greatest efforts for prevention should target lifestyle changes.
DIAGNOSTIC TECHNIQUESThe field of biomarkers continues to be dominated by troponins, as seen in the TRAPID-AMI study,43 which was presented at the most recent congress of the European Society of Cardiology. It involved a prospective validation of an algorithm that predicted the determination of ultrasensitive troponin T both at admission and 1 h afterward in a cohort of 1282 individuals who were treated for chest pain in the emergency department. The algorithm was able to rule out ACS in 63.4% of the patients, with a negative predictive value for infarction of 99.1%. The mortality rate in this group of patients was 0.1%, which confirms that this algorithm is safe and effective when used in conjunction with the patient medical history, physical examination, and electrocardiogram.
We have also seen the presentation of new and interesting diagnostic/prognostic point scales that combine clinical variables and biomarkers, such as the BIO-VILCAD44 in chronic CAD and INTERHEART-cholesterol,45 which analyzed a Spanish cohort with chest pain.
Data about the value of membrane microvesicles (particles that are generally derived from platelets) in infarction46 or microRNA in several contexts have expanded the scope of both diagnostic and prognostic studies.47–49 New data have also been published about B-type natriuretic peptide24,26 and copeptin.27 The current state of nontroponin biomarkers is summarized in the Figure and is discussed in extensive detail by Millard and Tranter50 in their excellent review.
Hospital mortality (A) and 6-month mortality (B) stratified by type of acute coronary syndrome in the DIOCLES and MASCARA registries; ACS, acute coronary syndrome; DIOCLES: Descripción de la Cardiopatía Isquémica en el Territorio Español; MASCARA: Manejo del Síndrome Coronario Agudo. Registro Actualizado; NSTEACS, non—ST-segment elevation myocardial infarction.
As for physiological or imaging techniques, it is important to highlight the publication of consensus documents: one about the definitions of ischemia with various diagnostic methods,51 and another about the criteria for the appropriate use of the different multimodal diagnostic techniques in chronic CAD.52
A prospective study of 3656 patients evaluated the usefulness of additional diagnostic tests after diagnostic ergometry. The diagnostic performance of ergometry was lower in patients with a negative test and those who showed rapid recovery of electrical changes. Meanwhile, it was higher in those who had a clinically positive test (typical angina), even in the absence of electrocardiographic changes, or in patients with positive clinical and electric ergometry.53 Using speckle tracking on stress echocardiography, Peteiro et al54 observed that basal rotation at peak exercise is deteriorated in patients with an ischemic response to exercise. In contrast, apical rotation and torsion are similar to those of patients with normal tests.
In noninvasive angiography by multidetector computed tomography (CT), a new analysis of the ROMICAT-II (Rule Out Myocardial Infarction/Ischemia Using Computer-Assisted Tomography II) study showed that, in patients with chest pain and initially normal electrocardiogram and troponins, the detection of high-risk plaque on multidetector CT was an independent prognostic factor of significant coronary disease, and it was shown to be useful for clinical staging.55 Furthermore, several articles have validated the long-term prognostic value of multidetector CT in patients with suspected CAD.55–57
In nuclear medicine, the combination of single-photon emission CT/CT to determine fractional flow reserve also improved the detection of coronary disease.58 In addition, the SPARC study59 analyzed the 2-year treatment costs in 1703 patients with suspected coronary disease, which were less for single-photon emission CT compared with multidetector CT and positron emission tomography, with no differences in mortality rate. Researchers of the BASKET LATE IMAGING study60 showed the prognostic value of single-photon emission CT for detecting ischemia 5 years after percutaneous revascularization. They indicated that abnormal findings are frequent, regardless of symptoms, and are usually located in regions that had not been treated.
Inducible ischemia, detected with stress cardiac magnetic resonance, was the most powerful predictor for major events in 391 patients with ventricular dysfunction.61 Last of all, the CE-MARC study62 showed higher sensitivity of cardiovascular magnetic resonance compared with single-photon emission CT in 235 women and 393 men with suspected angina; no differences were detected between sexes.
STABLE CORONARY ARTERY DISEASEThe results of the SIGNIFY63 clinical trial were presented at the most recent congress of the European Society of Cardiology. The study randomly assigned 19 102 patients with stable CAD, without heart failure, and with a heart rate of ≥ 70 beats per minute to receive either ivabradine or a placebo with optimal medical treatment. The primary outcome was a composite of cardiovascular mortality and nonfatal myocardial infarction. The incidence of bradycardia was significantly greater in the ivabradine group (18.0% vs 2.3%; P < .001), and was the main reason for suspending the drug. After a follow-up of 27.8 months, no significant differences were observed in the primary objective between the ivabradine and placebo groups (6.8% vs 6.4%, respectively; HR = 1.08; 95%CI, 0.96-1.20; P = .20). Likewise, no significant differences were found between the ivabradine and placebo groups for the secondary endpoints of cardiovascular death and nonfatal myocardial infarction. In the patients with angina, ivabradine significantly reduced the number of angina episodes (P = .01). However, in patients with Canadian Cardiovascular Society functional class ≥ II, ivabradine significantly increased the incidence of the primary objective (7.6% vs 6.5%; P = .02) while the absolute risk for cardiovascular death and nonfatal myocardial infarction increased by 1.1%. Given these results, it is expected that the indications for ivabradine in stable CAD will be revised.
At the same congress, the 2-year follow-up results were presented from the FAME 2 study.64 In 1220 patients with stable CAD, the fractional flow reserve (FFR) was measured of the stenoses that were visible on angiography. The 888 patients with at least 1 stenosis with an FFR ≤ 0.80 were randomized to either FFR-guided PCI and treatment with medication or medication alone. The primary outcome was a combination of all-cause death, nonfatal myocardial infarction and urgent revascularization. The incidence of the primary endpoint was significantly lower in the PCI group (8.1% vs 19.5%; HR = 0.39; 95%CI, 0.26-0.57; P < .001), basically due to less urgent revascularization in the PCI group, and no significant differences were observed in mortality or nonfatal myocardial infarction. Therefore, in patients with stable CAD, FFR-guided PCI improves results compared with medication alone. Furthermore, in this study, patients with angiographic stenosis and FFR > 0.80 showed good results with drug therapy alone.
ACUTE CORONARY SYNDROME WITHOUT ST-SEGMENT ELEVATIONResults have been published from an interesting subanalysis of the PLATO study centered around 5366 patients (48.4% of all NSTEACS) managed without revascularization for the first 10 days after randomization.65 Researchers observed a reduction in the risk for ischemic events that was similar to the PCI treatment groups, with no increased risk of hemorrhages.
As for the optimal duration of treatment with dual antiplatelet therapy after ACS, data continue to appear that corroborate the importance of following the recommendation of clinical guidelines and maintaining dual antiplatelet therapy for at least 12 months. The data of a prospective cohort of 56 440 patients with ACS out of the SWEDEHEART (Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies) registry66 clearly show an increase in risk of death, stroke and reinfarction (HR = 0.84; 95%CI, 0.75-0.95) in patients who stop dual antiplatelet therapy within 3 months after ACS, compared with those who continued this therapy for more than 3 months. Although the risk for major hemorrhages was higher in patients with longer dual antiplatelet therapy (HR = 1.56; 95%CI, 1.18-2.07), the number of bleeding events in absolute terms was small.
The FAMOUS-NSTEMI study67 randomly assigned 350 patients with NSTEACS to either an FFR-guided revascularization strategy or angiography-guided standard care. The 12-month revascularization rate was higher in the group without FFR, but no differences were seen in quality of life or other events. Fractional flow reserve measurement was associated with a change in treatment for 21.6% of the patients.
With regards to pharmacological innovation, this year there has been a report of the failure of Lp-PLA2 inhibitors (lipoprotein-associated phospholipase A2) to prevent ischemic events after ACS. The VISTA-16 study68 randomized 5145 patients to receive either varespladib (500mg/day) or placebo; treatment was initiated within the first 96h following an ACS and lasted for a duration of 16 weeks. This study was prematurely interrupted due to the lack of effectiveness in the main outcome of cardiovascular death, infarction, stroke or unstable angina, and due to a greater risk of infarction in patients treated with varespladib (3.4%) compared with placebo (2.2%) (HR = 1.66; 95%CI, 1.16-2.39). Results have also been published from the SOLID-TIMI 52 study,69 which compared darapladib (160mg/day) with placebo in 13 026 patients after ACS. Treatment with darapladib did not reduce the incidence of recurrent coronary events (death, infarction, or urgent need for revascularization) compared with placebo: 16.3% and 15.6% at 3 years, respectively (HR = 1.00; 95%CI, 0.91-1.09).
ACUTE CORONARY SYNDROME WITH ST-SEGMENT ELEVATIONAmong the new studies presented within the last year, 2 clinical trials merit comment as they reexamine an old argument: should all the arteries be revascularized during primary PCI or only the culprit artery? The PRAMI study70 attempted to answer this question by randomly assigning 465 patients in 5 hospitals in the United Kingdom to either a complete, preventive revascularization strategy or to revascularization of only the culprit artery. The complete revascularization strategy significantly reduced the primary outcome of death from cardiac causes, nonfatal myocardial infarction, or refractory angina at 2 years, with no differences observed in cardiac death. This strategy was most recently evaluated in another British randomized trial, the CvLPRIT study,71 with only 296 patients. The results were similar in the significant reduction of the primary endpoint (which in this instance also included hospitalizations due to heart failure) with revascularization of all the lesions, although mortality was similar and the benefits obtained were in the reduction of repeat PCI or rehospitalizations.
The new guidelines on myocardial revascularization72 maintain the recommendation of revascularizing only the culprit artery during primary PCI and opting for revascularization that is as complete as possible in patients with shock or persistent ischemia after opening the hypothetical culprit artery (class II indication, level of evidence A). A “staged” revascularization strategy that takes place over several days or weeks continues to be the recommendation for the revascularization of nonculprit lesions in patients with symptoms or inducible ischemia (class II indication, level of evidence A).
Another aspect that is still being analyzed is thrombus aspiration during primary PCI. The 1-year follow-up has been published from the TASTE (Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia) study,73 which randomly assigned 7244 patients to routine thrombus aspiration or conventional PCI. Routine aspiration did not reduce mortality, the combined primary endpoint, or thrombosis of the stent the first year. The new guidelines for coronary revascularization reduce the indication of thrombus aspiration during primary PCI, which is currently class II, level of evidence B (may be considered in selected patients).72
The ATLANTIC study74 is a double-blind trial that studied the effectiveness and safety of prehospital treatment with ticagrelor in conjunction with acetylsalicylic acid compared with in-hospital administration. It analyzed coronary flow restoration in the blocked artery, resolution of the ST segment, as well as pretreatment safety. The objective of effectiveness, however, was not met. The pretreatment strategy was safe, with a hemorrhage rate that was low and identical to that in the patients with in-hospital ticagrelor treatment. There was a significant reduction in stent thrombosis in the prehospital strategy group. Furthermore, there was a benefit of pretreatment in the patient subgroup not receiving morphine. The most important limitation of this study is undoubtedly the short time interval between drug administration and reperfusion (48min between randomization and angiography; 31min between the 2 loading doses).
This year, 2 Spanish groups have published their results in the field of reperfusion injury. The METOCARD study75 showed a reduction in infarct size with metoprolol treatment before primary PCI in patients with Killip class I or II infarction. A large-scale clinical trial will analyze the impact of this strategy in terms of the reduction of clinical events. Furthermore, the Ischemic Postconditioning on Microvascular Obstruction in Reperfused Myocardial Infarction clinical assay76 studied the role of postconditioning with balloon inflations after the opening of the artery in patients treated with primary PCI. There was no significant difference between the treatment groups in microvascular obstruction or other parameters for myocardial injury measured by cardiovascular magnetic resonance on the fourth day. Interest in this strategy seems to be waning due to the lack of consistent results and objective benefits.
SPECIAL POPULATIONSSenior patientsElderly patients have higher baseline risk, comorbidities and frailty, which makes them more susceptible to iatrogenesis, which can restrict the use of certain therapies. This year, Revista Española de Cardiología has published an excellent review about the management of these patients.77 It shows that, despite the lack of representation of this age group in many studies, older patients generally benefit from the same therapeutic measures as younger adult populations. Along this same idea, data from a Swedish series have shown that senior patients with ACS are treated conservatively and have fewer angiographies than younger patients, even in advanced healthcare systems in this day and age.78 A meta-analysis of more than 9100 clinical trial patients with NSTEACS has demonstrated that elderly patients experience greater benefits from an invasive approach with early angiography than younger patients, while mortality and recurrence of infarctions are lower.79
Undoubtedly, frailty assessment should be considered part of the systematic medical workup of hospitalized senior patients. In this regard, data should be highlighted from the Swedish SCAAR registry80 about 4876 primary PCI in octogenarian patients (mean age 83 years) who had had NSTEACS in the previous 10 years. The data showed a small reduction in mortality in the first year (26% vs 23%) but no significant reduction in the rates of reinfarction, heart failure, stroke, or bleeding.
WomenRegarding women with ACS, a recent review underlines the well-known disparities in greater diagnostic delay, less use of the invasive approach and other measures with demonstrated effectiveness, higher risk of hemorrhage, and poorer short-term prognosis than in men of the same age.81 The greatest gap was observed among younger adults and patients with ST-segment elevation myocardial infarction, which persisted after controlling for other risk factors. These differences could be explained not only by biological and hormonal factors, but also by others that make men and women different, such as their distinct social roles.
The impact of cardiovascular risk factors is not the same in both sexes. In a recent meta-analysis with more than 850 000 patients and more than 28 000 events, the presence of diabetes mellitus had a much greater impact in women than in men, which resulted in the women having a 40% higher risk for developing CAD.82
It is also clear that women have a greater prevalence of nonatherosclerotic coronary disease, especially before menopause. A recent article studied 366 women under the age of 55 with ACS from the GENESIS PRAXY study,83 all of whom had undergone angiography. In 10% of patients, the lesions were spontaneous coronary dissection, which in many cases had angiographic findings that were compatible with fibromuscular dysplasia. Despite having a lower lesion load and fewer risk factors on hospital admission, the prognosis after hospital discharge of these patients was poor, with a 1-year mortality rate of 7% and a rehospitalization rate of 17%.
CRITICAL CARDIOVASCULAR CAREFirstly, we highly recommend the excellent series of review articles about different topics related to critical care that has been published since August 2013 in the New England Journal of Medicine.84
General critical careIt is important to highlight a new contribution to one of the classic debates in medicine: should patients with hypovolemic shock be resuscitated with colloids or crystalloids? The multicenter CRISTAL study85 compared treatment with either colloids or crystalloids in more than 2800 patients with hypovolemic shock. There was no difference in the primary outcome of 28-day mortality, but at 90 days there were fewer deaths in colloid-treated patients (relative risk = 0.92; 95%CI, 0.86-0.99; P = .03), who also needed less vasopressor treatment and mechanical ventilation (secondary outcome). Unlike previous reports, no differences were detected in renal failure or the need for renal replacement therapy between the 2 groups.
Another controversial topic refers to the theoretical renal protective effect and increased diuresis of low-dose dopamine treatment in patients with acute heart failure. The multicenter, double-blind, randomized ROSE trial86 compared the effect of additional treatment with dopamine at a dose of 2μg/kg/min with nesiritide at a dose of 0.005μg/kg/min in more than 200 patients with acute heart failure and renal dysfunction (estimated glomerular filtration rate, 15-60mL/min/1.73 m2) treated with diuretics. No differences were observed in the primary endpoints of 72h cumulative urine volume and change in serum cystatin C concentrations. The authors conclude that neither of the 2 drugs had a favorable impact on diuresis or renal function.86
Healthcare personnel attire is an aspect of the medical profession that is rooted in culture and tradition. Nonetheless, information about its role in the cross-transmission of infectious diseases is limited. In an interesting consensus article, Bearman et al87 analyzed the available evidence in order to develop attire recommendations. In short, the recommendations for in-hospital apparel include: “bare below the elbow strategy”, meaning a short-sleeve shirt or scrubs with no wristwatch or jewelry; limited use of white coats and, whenever possible, removal of the white coat before coming into contact with the patients; if a necktie is worn, it should not come into contact with the patient; the hospital should provide frequent laundering (daily would be ideal) of white coats and hospital scrubs; and, stethoscopes should be cleaned between patient visits.
Cardiac arrestIn the last year, the results from a new and controversial international randomized trial have once again discussed the indication of therapeutic hypothermia in unconscious patients after resuscitation from cardiac arrest. In the TTM trial,88 a total of 939 unconscious patients were randomly assigned after resuscitation from cardiac arrest to receive treatment with therapeutic hypothermia with a target temperature of either 33°C or 36°C (control group). Surprisingly, there were no differences in the primary outcome of all-cause mortality between the 2 treatment groups (50% in patients from the 33°C group and 48% in the 36°C group). After 180 days, there was also no significant difference observe in the secondary composite endpoint: poor neurological function or death evaluated with the Cerebral Performance Category scale and the modified Rankin scale. The results from the analyses adjusted for known prognostic factors were similar. As mentioned in the accompanying editorial article,89 perhaps the most important message that can be extracted from this trial is that the care that these patients received, including temperature control, is effective and improves survival after cardiopulmonary resuscitation. Few medical procedures have achieved an absolute improvement of this magnitude in the same period.
Another aspect that has been debated is the optimal moment to begin therapeutic hypothermia. In a recent randomized trial, Kim et al90 assigned 1359 patients with prehospital cardiac arrest who had been resuscitated by paramedics to a strategy of rapid prehospital cooling with 4°C saline compared with standard care. Although the prehospital cooling group reached the target temperature of 34°C more quickly, there were no differences in the primary outcomes of survival or neurological status between the 2 groups. Due to the above reasons, future studies will be necessary to clarify which temperature control strategy is best in patients who have been resuscitated after cardiac arrest and to define the optimal moment for the application of this strategy.
Finally, in an interesting analysis of more than 18 000 patients who had been resuscitated after cardiac arrest, significant differences were found in survival according to the season of the year and time of day of the cardiac arrest. Nighttime and winter cardiac arrests were associated with lower survival. These differences continued to be significant in the multivariate analysis after adjusting for several recognized prognostic factors.91
CONFLICTS OF INTERESTNone declared.