In recent years a number of articles reflecting advances in the field of heart valvulopathies have been published in different cardiology journals. The aim of this editorial comment is to provide the general cardiologist with an annotated overview of the main ones. For additional details the reader is referred to 3 recent articles.1-3
Concerning the area of cellular processes and neurohormones, recent research into defining cellular mechanisms for degenerative valvular disease revealed that an endochondral bone process expresses cartilage in myxomatous mitral valves and bone in the calcified aortic valves (AV). Valve degeneration occurs due to thickening from an osteoblastic differentiation process mediated by the low-density lipoprotein receptor-related protein (Lrp5) signaling pathway.4 Other studies have shown neoangiogenesis and increased heat shock protein hsp 60 gene expression in end-stage calcified stenotic AV that was not present in control valves.5
Natriuretic peptide measurements in 130 patients with severe aortic stenosis demonstrated higher levels with increasing New York Heart Association (NYHA) functional classes, decreasing left ventricular ejection fraction and increasing severity of disease.6 The additional clinical value of these measurements needs to be determined.
Infective Endocarditis
In the field of infective endocarditis (IE), the use of serial trans-thoracic echocardiography (TTE) or trans-esophageal echocardiography (TEEs) to improve the diagnostic yield in IE was studied. The positive diagnostic findings from TTE and TEE in the first examination were 21.2% and 68.5%, respectively; reclassifications after the second examination were 13.5% and 46.9%, respectively, and after the third examination were 7.5% and 20%, respectively. TEE had a better sensitivity than TTE. For both TTE and TEE if three studies were negative no additional information was obtained from further examinations.7
A double blind, randomized, placebo-controlled trial in children undergoing intubation or dental procedures compared bacteremia occurrence rates in those that received the American Heart Association-recommended dose of amoxicillin versus those assigned to a placebo. The bacteremia rates were lower in the amoxicillin group supporting the need for antibiotic prophylaxis.8 In comparison to placebo in a randomized controlled trial aspirin did not decrease embolic events in IE and showed a trend towards higher bleeding risk (P=.075).9
One hundred and fifty three patients with complicated, left sided native-valve IE were treated with antibiotics. Forty five percent underwent valve surgery and 55% received medical therapy alone. The 6-month mortality in the valve surgery group was 16% versus 33% in the medically treated arm.10 Most of the deaths in the no surgery group occurred in the first two weeks. Those with significant heart failure showed the greatest reduction in mortality with surgery (14% vs 51%, P=.001) (Figure 1).
Figure 1. Kaplan-Meier curve relating valve surgery to time to death among propensity-matched patients. (From Vikram HR, et al.10)
Surgical repair of the mitral valve for IE was investigated. Sixty-three of 78 patients underwent mitral valve repair (MVrep). Five-year survival after MVrep for acute endocarditis was 96 (4)% and for healed endocarditis was 91 (5)%.11 In another study including 37 consecutive patients who had MVrep for active IE using Carpentier's techniques between 1989 and 1994, the 10-year survival was 80% and freedom from MV reoperation was 91%.12
In another study of 154 patients with IE undergoing surgery, 63% had mitral valve replacement (MVR) and 37% had MVrep. Patients with MVrep had a lower incidence of atrial fibrillation, less dyspnea, were less likely to be in NYHA functional classes III/IV and needed reoperations less frequently. The 30-day mortality was better with MVrep (1%) than with MVR (4%).13
In a Spanish series, mid-term outcomes after medically successfully treated IE in sixty-seven of 151 (44%) patients were as follows: Thirty-five patients required late surgery to correct sequelae of the infection, and 21 of these (68%) died during follow-up, and survival rates without cardiac surgery at 1, 3 and 5 years were 54%, 29% and 20% respectively. Thus, mortality with only medical treatment was high.14
Early clinical predictors of in-hospital death were embolic events, diabetes mellitus, staphylococcus aureus, and APACHE II scores.15 Predictors of major embolic events as determined by multivariate logistic regression analysis were young age (P=.006), vegetation size (P=.045) and C-reactive protein (P=.028).16
Aortic Stenosis
Another area in which considerable progress has taken place is aortic stenosis. In the Framingham Heart Study, electron beam computed tomography (EBCT) when compared to echocardiography in 327 patients, exhibited a sensitivity of 24% and a specificity of 94% for the detection of "degenerative" AV disease.17 Comparing cardiovascular magnetic resonance imaging (CMR), transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE), in patients undergoing cardiac catheterization to detect AV area of ≤0.8 cm2 by cardiac catheterization showed the sensitivity and specificity for CMR was 78% and 79%; for TTE was 74% and 67%, and for TEE was 70% and 70%.18 At the present time EBCT and CMR are not superior to echocardiography/Doppler; their role in clinical practice needs to be further evaluated.
In a study of 405 patients with acute coronary syndrome, independent predictors of cardiac death and myocardial infarction (MI) at one year were coronary artery disease, MI at index admission, ascending terciles of C-reactive protein, congestive heart failure, and age.19 Identification of AV sclerosis in patients with chest pain at presentation to the emergency department was not a predictor of cardiac death or MI.
In the article by Monin et al, 136 patients with severe aortic stenosis, aortic valve area <0.7 cm2 , and LVEF <0.31, were enrolled in a prospective study. "Contractile reserve" was measured using echo Doppler and was defined as a ≥20% increase in stroke volume with intravenous dobutamine infused to a maximum dose of 20 µg/kg/min. Comparison of two groups, one with and the other without contractile reserve, showed that surgical treatment was better than medical management in both groups,20 and thus, estimation of "contractile reserve" failed to accurately identify a subset of individuals in whom surgery was not beneficial. Six hundred and twenty two asymptomatic patients who were ≥40 years of age with valvular AS who did not have early AV replacement (AVR) were followed prospectively to determine their natural history. During follow-up, while unoperated, the probability of remaining free of cardiac symptoms was 82% at one year, 67% at two years, and 33% at five years.21 Unfortunately, in the above study no reference is made to the number of patients with co-existing coronary artery disease and the incidence of coronary arteriography is not reported.
Several studies performed during the last years have evaluated the role of different drugs in aortic stenosis. β-blockers, ACE-inhibitors, angiotensin receptor blockers and statins, have not been shown to slow the progression of the disease.22-24
Bicuspid Aortic Valve
A number of interesting reports on bicuspid aortic valve (BAV) have shed light on different aspects of this entity. Prevalence of bicuspid aortic valve (BAV) was 0.5% in a prospective study of 817 children, age 10 years, of whom 400 were males and attended school in an area with 41 432 inhabitants.25 Echocardiography showed BAV in 0.75% males and 0.24% of females. The dimensions of the aortic root were larger in the BAV when compared to the tricuspid AV (at the level of the annulus, 20.5 (2.6) mm versus 18.4 (2.6) mm; at the sinuses of Valsalva, 25.7 (2.0) mm versus 22.2 (2.4) mm [P=.02]; and in the ascending aorta, 22.2 (4.4) mm versus 19.7 (2.3) [P<.001]).25 In another study of 162 patients with BAV without valve dysfunction, age 23.6 (19.8) years, all aortic measurements at the sinuses of Valsalva, sinotubular junction, and ascending aorta were increased.26
BAV is a heritable disorder that was demonstrated by echocardiography of 309 probands and relatives. 74 were shown to have BAV (prevalence of 24% and heritability [h2] of 89%) and 97 had BAV and/or other cardiovascular malformations (prevalence of 31%, h2 of 75%).27
The presence of fundamental cellular abnormalities in aneurysmal segments of BAV thoracic aortas was studied. Some of these changes were similar to the histopathological findings of Marfan syndrome. Cystic medial necrosis without inflammatory infiltrate in tissues was seen in both. Cultured BAV and Marfan syndrome vascular smooth muscle cells (VSMC) showed intracellular accumulation of fibrillin, fibronectin, and tenascin.28
Sixty-eight patients with BAV and a mean age of 44 years had at least two echocardiograms >12 months apart during a follow-up of 47 months. Along with increasing aortic diameters the mean aortic gradient went from 17.6 to 25.7 mm Hg (P<.001) and the degree of AR worsened in 17 patients (25%). All of these changes occurred irrespective of baseline BAV function.29
In one study, out of 185 patients post-AVR, only 9.3% had further aortic dilation and 7% of the study group had a BAV.30 A second study compared patients with BAV and tricuspid aortic valves (TAV) undergoing AVR versus those who had BAV but not AVR. It showed that in BAV there was further progressive dilation of the aorta irrespective of whether the patient had an AVR or not. No further dilation was observed in those patients who had a TAV and underwent AVR.31 When comparing aortic dilatations, BAV show further progressive dilatation in the aorta as compared to those with TAV, with increasing age.
Aortic Regurgitation
A small group of papers have addressed different aspects of aortic regurgitation. Forty consecutive patients with aortic regurgitation, left ventricular ejection fraction (LVEF) ≥0.55, LV end-diastolic pressure ≤15 mm Hg, right ventricular (RV) systolic pressure ≤30 mm Hg, and normal coronary arteries were studied by echocardiography/Doppler. They were all noted to have evidence of abnormal RV relaxation and filling.32 This is probably the Bernheim syndrome/effect first described in 1910.33 Clinically at the bedside the patients with Bernheim effect have an elevated jugular venous pulse, absence of RV heave, and since there is no increase in pulmonary vascular resistance the intensity of pulmonary valve closure (P2) would be normal. Paul Wood described this pathophysiological process in the following terms: the dilation of the LV along with rapid filling of the LV in early diastole (eg, from left sided valve regurgitation) results in the septum bulging into the RV and interfering with the proper filling of the RV. Therefore the RV is small and the right atrium is enlarged.34 A large series of 1410 individuals undergoing surgery for aortic regurgitation between 1986 and 2001 was analyzed by Minakata et al. A subgroup of 160 patients (11%) had valve repair with one operative death (0.6%) and two patients required early re-repair. At a mean interval of 2.8 years 10% had a re-operation; at 7 years this number increased to 15%. At seven years the survival was 89%. Aortic valve (AV) repair with good results was therefore found to be feasible in selected patients.35 Another study reported on AV repair when this was performed in patients undergoing surgery for aortic regurgitation. Re-operation rates for recurrent AR were 3.3% and in-hospital mortality was 3.9%. In those with isolated valve repair, isolated root repair and a combination of both, the incidence of AR grade ≥II at five years was 19%, 16% and 6% respectively; the incidence of re-operation was 7%, 5%, and 2% respectively.36 Tornos et al, studied the postoperative outcomes of 170 patients undergoing aortic valve replacement, either early per the guidelines or late, for chronic severe aortic regurgitation. 60 patients were operated on early according to the guidelines advice and 110 patients were operated on later. The outcomes in the early and later groups were as follows: death was 12% and 37%, and cardiac death was 9% and 28% respectively. Overall survival in the early and late groups was 90% (4) versus 75% (8) at 5 years, 86% (5) versus 64% (5) at 10 years, and 78% (7) versus 53% (6) at 15 years, respectively (P=.009)37 (Table 1).
Mitral Stenosis
In the field of mitral stenosis, a prospective study calculated mitral valve area (MVA) by pressure half time, two-dimensional echocardiography, proximal iso-velocity surface area, and real-time three-dimensional echocardiography (RT3D). These were compared with MVA obtained within 24 hours by using the Gorlin formula (simultaneous LV-left atrial pressures and cardiac output by thermodilution) in 80 patients. RT3D showed the best agreement with MVA obtained from the Gorlin formula when compared to all other echocardiographic methods. Also RT3D had the best interobserver and intraobserver variability with Kappa indexes of 0.84 and 0.96, respectively.38
Catheter balloon commissurotomy (CBC) was performed in 36 pregnant patients (mean age 25.8 [4.3] years, mean gestational period 26.5 [5.3] weeks), with 25 in NYHA functional class III/IV. Fluoroscopy time was ≤4 min in 63.9% of the patients. MVA increased from 0.74 to 1.59 cm2 with procedure success in 35 of 36 patients. Increase in mitral regurgitation >2 grades was observed in only 19.4% and none needed valve surgery. Fetal outcomes were normal. All patients were in NYHA functional class I/II on follow-up.39 Three hundred and twenty three consecutive patients undergoing CBC for MS had no change in their risk for developing subsequent atrial fibrillation. At baseline 181 had no history of atrial arrhythmias. Eventually, atrial fibrillation developed in 37 (20%) patients.40
Fifty-three patients with severe MS and moderate to severe tricuspid regurgitation (TR) underwent CBC. TR regression occurred in 51% of them. Patients in whom the TR decreased were younger, had higher pulmonary artery (PA) pressures, higher prevalence of functional TR and more severe MS (P<.005).41
Mitral Regurgitation
Many different aspects of mitral regurgitation (MR) have been the focus of recently published papers. Some of those investigating neurohumoral activation and cellular processes deserve special comment. Plasma tumor necrosis factor-alpha (TNF-α) expression is increased in the plasma and myocardium of patients with chronic mitral regurgitation (MR) and in instances of mitral valve (MV) repair where the volume overload state is corrected this expression is reversed. The extent of regression in the left ventricular remodeling after MV repair is proportionate to the amount of pre-operative TNF-α levels.42 Another study showed that in 49 patients with MR, the plasma natriuretic peptide (NP) levels in symptomatic patients were greater than in asymptomatic patients and greater in asymptomatic patients with MR than in normal controls. NP levels also increased with worsening severity of MR and further enlargement
of the LA (P<.001).43 Calculated extravascular norepinephrine release rates (NE2) were increased in patients with MR who were clinical class I, or had a mean PA wedge pressure <12 mm Hg, or had LVEF ≥0.60. Mean NE2 values were also increased further in patients who had an LVEF <0.60 (P=.02). This indicates that the sympathetic nervous system is activated in MR.44 The structure of MV leaflets and chordae in patients with mitral valve prolapse (MVP) and Marfan syndrome were studied by Grande-Allen et al. Histological examination of the leaflets in areas of myxoid degeneration revealed abnormal fibrillin and altered protein matrix architecture. The MV leaflets and chordae in MVP had a 3% to 9% higher water content and 30% to 150% higher concentration of glycosaminoglycans than normals (P<.005). There were also lower collagen concentrations in the leaflets compared to normals (P<.002).45 The structural abnormalities of the MV leaflets and chordae in patients with MVP were therefore similar to those seen in Marfan syndrome.
A study of 70 patients who had exercise stress echocardiography and who were in the chronic post-MI phase and had LVEF <0.45, showed a wide range of variation in the effective regurgitant orifice (ERO) unrelated to the severity of resting MR. Independent predictors of ERO on exercise were changes in mitral deformation (ie, differences in systolic mitral tenting area, systolic annular area, and coaptation height; P<.0001) and wall motion score in anterior and inferior MI groups. Overall the changes in ERO were related to those in LV remodeling and in mitral deformation but not those in global LV function.46 Seventy-four patients with previous acute myocardial infarction and LV systolic dysfunction were divided into two groups based on the presence or absence of acute pulmonary edema. On exercise, patients who developed acute pulmonary edema due to ischemic mitral regurgitation had less reduction of LV end-systolic volume, less reduction of LV wall motion index, and greater increases of tenting area, regurgitant volume, effective regurgitant orifice area, and tricuspid pressure gradient.47
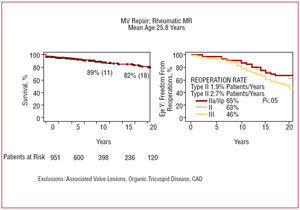
Long-term follow-up data was published with MV repair in nonrheumatic and rheumatic mitral regurgitation using the Carpentier's techniques, used in the first 1113 patients between 1970 and 1994. Of those with a nonrheumatic etiology of MR, 90% had a "degenerative" MV, mean age was 56 years, operative mortality was 1.9% and the median follow-up was 17 years. In patients with rheumatic MR, the mean age was 25.8 years, sinus rhythm was present in 63%, operative mortality was 2% and mean follow-up was 12 years. Survival, cardiac event-free survival, and reoperation rates are shown in figures 2 and 3.48,49
Figure 2. Survival at 10 and 20 years and freedom from cardiac death (left panel). Reoperations according to leaflet prolapse (right panel). MR indicates mitral regurgitation. (From Braumberger E, et al,48)
Figure 3. Actuarial survival after mitral valve (MV) repair of patients with rheumatic mitral regurgitation (MR) is shown in left panel. Freedom from reoperation after MV repair of patients with rheumatic MR is shown in right panel. (From Chauvand S, et al.49)
Tricuspid Regurgitation
In reference to tricuspid valve disease, a review of 41 patients with asymptomatic severe tricuspid regurgitation (TR) after permanent pacemaker (PPM) or implantable cardioverter-defibrillator (ICD) placement showed that 7 patients had perforation of the tricuspid valve (TV) by PPM or ICD leads, 4 had lead enlargement of the TV, 16 had lead impingement of the TV leaflets, and 14 had lead adherence to the TV. TEE was more successful in diagnosing TV malfunction or in establishing the presence of significant TR when compared to transthoracic echocardiography. Time from implantation to operation was 72 months (range 2 to 228 months).50 Two-dimensional transthoracic echocardiography before and 5 (4) days after TV annuloplasty and left heart valve surgery was used to determine resolution of pre-operative functional TR. Multivariate analysis showed that age, tethering distance and severity of pre-operative TR (all P<.001) were independent predictors of residual TR.51 In a separate cohort of 60 patients with TR due to flail leaflets, 33 eventually had tricuspid surgery at five years. The causes of flail leaflets included blunt trauma and iatrogenic chordal severing most from RV biopsy. The survival at 10 years was 61 (10) %.52
Prosthetic Heart Valves
Regarding prosthetic heart valves and their associated complications, some valuable works have been published recently. Thrombosis of a prosthetic heart valve (PHV) is a life threatening emergency. A single-center study reported 127 instances of prosthetic heart valve thrombosis (PHVT) in 110 consecutive patients (between 1978 and 2001) who received fibrinolytic therapy. Full success was achieved in 70.9% of instances. Of these outcomes 69% were achieved with the use of a single fibrinolytic agent, an additional 17% with the use of multiple agents, and 12% failed fibrinolysis altogether. Streptokinase and rt-PA did better than urokinase. There were 25.2% complications.53 In a multi-center study, 107 patients who underwent TEE showed a mortality rate of 5.6% and a complication rate of 17.8% with thrombolytic therapy. Complete hemodynamic success (defined as return of gradient to "normal" levels) was achieved in 76.3% and partial success in 8.6%. Clinical success (defined as hemodynamic success without clinical complications) achieved for aortic, mitral and tricuspid was 63.6%, 74.6%, and 93.3% respectively. The independent predictors of success were smaller thombus area by TEE and lack of previous history of stroke (Table 2).58 Therapeutic suggestions are listed in Table 3.
The choice of a PHV is influenced by multiple factors. These include known long-term results from randomized trials and databases, patient characteristics such as age and gender, associated cardiovascular, and other co-morbid conditions, expected survival of the patient and unique patient needs.54 An algorithm for choosing a PHV in an adult patient is given in Figure 4.
Figure 4. Choice of prosthetic heart valve in adult patient. (From Rahimtoola SH.1)
During pregnancy, a patient with a mechanical PHV should be managed with intravenous unfractionated heparin used in the first 3 months, which clinically is realistic in the 6-12 week time period, warfarin from week 13 to the last 2 weeks of pregnancy, and intravenous unfractionated heparin again at the end of pregnancy. Ten studies with 427 pregnancies reported that the incidence of warfarin embryopathy was zero. Four recent studies from 1994 to 1999 reported an incidence of 1.6% of live births.55 For those patients with bioprosthetic PHVs in pregnancy the main problen is the rate of structural valve deterioration (the incidence may average 24%) and at 10 years the incidence of PHV-related reoperation is 60% to 80%.
A prospective randomized trial of the Starr-Edwards and the St. Judes valve for both AVR and MVR showed the average reduction in NYHA functional classes from preoperative levels to five years for Starr-Edwards and St Jude for AVR was 1.4 and 1.5, respectively, and for MVR was 1.8 and 1.6, respectively. The event-free survivals at 1, 5 and 8 years after AVR were 84%, 56%, and 45% for St Jude, and 81%, 54%, and 43% for Starr Edwards valves respectively (P=.65). The event-free survivals at 1, 5, and 8 years after MVR were 64%, 37%, and 25% for St Jude, and 79%, 35%, and 29% for Starr Edwards valves respectively (P=.46).56
In 812 patients, who underwent MVR with a mechanical prosthesis with or without a Maze procedure, risk factors for late mortality, by multivariate analysis, were preoperative NYHA functional class IV and age >65 years. Late incidence of atrial fibrillation was much lower in those patients that had a concomitant Maze procedure. The risk factors for stroke on multivariate analysis were: history of stroke, chronic atrial fibrillation, no Maze procedure, and year of operation.57
Correspondence: Dr. Shahbudin H. Rahimtoola.
University of Southern California.
2025 Zonal Avenue, Room GNH 7131,
Los Angeles, California 90033 USA.
E-mail: rahimtoo@usc.edu