To the Editor,
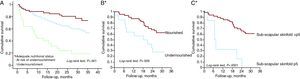
We were very interested to read the article by Bonilla-Palomas et al., “Influence of undernourishment on long-term mortality in patients hospitalized for heart failure” (Influencia de la desnutrición NS la mortalidad a largo plazo de pacientes hospitalizados por insuficiencia cardiaca),1 in which the authors analyze nutritional status (NS) and its influence on patient prognosis after acute hospitalization for heart failure (HF). The role of NS in the prognosis for HF has also been studied by our group with a similar follow-up period (median: 26.7 months) in an outpatient context.2 The results from both studies indicate that properly nourished patients have a significantly higher cumulative survival rate than undernourished patients (Figure 1).
Figure 1. Kaplan-Meier survival curves for the population from Bonilla-Palomas et al., organized according to Mini Nutritional Assessment (A) and the population from Gastelurrutia et al. according to the combination of undernourishment markers (B*) and sub-scapular skinfold (C*).*Taken from Gastelurrutia P et al. 2 with the permission of Elsevier.
The definition of undernourishment is heterogeneous, since there are several different methods used to evaluate NS and no single method of choice exists. The Mini Nutritional Assessment (MNA) is a method suggested by many authors to provide a rapid and simple evaluation of NS. However, HF patients frequently are not euvolemic during their evolution,3 and the MNA includes a measurement of body mass index (BMI), which is based on weight. In hyperhydrated patients, an excessively high weight value would ensue, causing error that would be based on the level of liquid retention and the dose of diuretics received by the congestive patients. As such, we believe that a more appropriate method for evaluating NS would be one that does not require a measurement of patient weight. In our study, we used a definition for undernourishment that combined 2 or more nutritional markers from among the most commonly used in the medical literature (albumin, total lymphocytes, triceps skinfold (TSF), sub-scapular skinfold (SF), and mid-arm muscle circumference) within a threshold of normality.4, 5
In the study by Bonilla-Palomas et al.,1 albumin markers and TSF were analyzed as possible predictors of mortality in a multivariate analysis and were eliminated from the model. However, continuous variables were used in lieu of categorical variables as in the MNA (undernourished/not undernourished). In our study, the parameters that retained their statistical significance with mortality were lymphocytes and subnormal SSF. Upon inclusion in the multivariate analysis, SSF remained in the model along with New York Heart Association functional class and age. The measurement of SSF is quick and simple, and can serve as a screening process for HF patients with worse prognosis. These results must be confirmed by more powerful studies.
It is vital to understand the type of undernourishment suffered by these patients, and the application of parameters that elucidate the proteic (albumin, visceral protein or mid-arm muscle circumference, muscle protein), caloric (subcutaneous skinfolds), and immune (lymphocytes) aspects of undernourishment can be very useful for a better understanding of the situation, allowing for appropriate interventional strategies. Both studies were carried out taking into account mortality due to any cause. It would be interesting to examine whether the results from both studies would be maintained after an analysis based on type of mortality, especially cardiac-related mortality. In this context, our group is performing a larger clinical trial in an attempt to answer these questions (NCT01396824).
We are in agreement with Bonilla-Palomas et al.1 and the editorial accompanying the article6 in that the evaluation of NS should be a part of the integral evaluation of patients with HF. Statistically powerful studies are also needed to evaluate the effect of possible interventional strategies in undernourished patients with HF.
.
Corresponding author: pgastelurrutia@gmail.com