Keywords
INTRODUCTION
In spite of the numerous therapeutic advances, the prognosis for heart failure (HF) continues to be poor.1 It is important to develop awareness of the prognostic factors in this clinical setting, as these can easily be reproduced, and will help us to identify patients with the most unfavourable clinical evolution. Cardiac troponin (Tn) is a specific, sensitive marker of damage to the myocardium the introduction of which into clinical practice has changed the definition and management of acute coronary syndromes.2,3
A variable percentage of patients hospitalized as a result of acute HF (23%-80%) have detectable levels of Tn, which appears to be related to the severity of the clinical condition and a higher incidence of death and re-hospitalization as a result of HF during follow up.4-9
It has been suggested that the presence of myocyte necrosis phenomena during acute decompensation may be contributing to the progression of the disease. The aetiology of HF in these studies was predominantly ischemic.4-7 With regard to patients with stable and out-patient HF, there are fewer data on the value of Tn, and these have also been gathered predominantly from populations with predominantly ischemic aetiology.10-12
On the other hand, in these studies Tn was measured transversally meaning the usefulness of prolonged Tn monitoring in patients with dilated nonischemic cardiomyopathy and its incidence was not clarified.12
The hypothesis of our study was the long-term monitoring of troponin values (TnT) in an outpatient clinic and in a population whose HF was not caused by ischemia, which may be helpful for prognostic stratification and clinical management. We therefore studied the incidence of its positivisation (TnT+), its clinical determinants and its prognostic value in long-term follow-up.
METHODS
Study Population
The study population consisted of 80 consecutive patients, attending an outpatient service specializing in HF during 2002-2004 and meeting the following criteria: a) an established diagnosis of chronic HF13;
b) stable clinical situation, without hospitalization during the previous 3 months and functional class of the New York Heart Association (NYHA) II-III (II/III 51/29); c) diagnosis of systolic function defined as a left ventricular ejection fraction (LVEF) <40% in the ultrasound study performed during the month prior to their inclusion; and d) nonischemic aethiology defined in all patients as the concurrence of absence of a history of ischemic cardiopathy and absence of coronary lesions. All patients had at least 1 coronary angiographic study and the study excluded all those with coronary lesions of any severity or with any history of acute coronary syndrome, as well as those on chronic haemodialysis. The aethiology was established as idiopathic in 62 (78%), of patient, valvular in 8 (10%), familiar in 6 (7%) and alcoholic in 4 (5%).
Their parameters and clinical, ECG, and analytical characteristics were included with the data from the initial visit. Patients were subsequently monitored at the outpatient clinic with an average frequency of 3.1 months (1.8-5.0 months). At each visit, the clinical evaluation included evaluation of the clinical status and blood samoling for TnT determination. All the patients had a conventional ECG during the month before they were included in the study (Sonos 550, Phillips, Andover, Massachusetts). The left ventricular ejection fraction was calculated using the modified Simpson method, using image with second harmonic second, and the projections and standard measurements were performed for the study of anatomy and cardiac function.14 The written, informed consent was obtained from all patients before they were included in the study.
Laboratory Parameters
Blood samples were obtained by venous puncture when the patients arrived to surgery, between 8 am and 10 am, fasting and after resting for 20 minutes. The cardiac TnT was measured using Electrochemiluminescence Immunoassay with a Roche Elecsys 2010 (Roche Diagnostics, Manheim, Germany) modular analyser. The detection limit provided by the supplier was <0.01 ng/mL and the variability coefficient was 5.6% to 0.04 ng/mL. Raised TnT was defined in accordance with the supplier, as a percentage value in excess of 99 percentile (>0.01 ng/mL) obtained from a population of 1951 healthy volunteers.15 The patients with a value of >0.01 ng/mL during the follow-up period were identified as TnT+, while patients with values <0.01 ng/mL during the entire follow-up period were classed as TnT-. Additionally, the index of TnT was calculated as the relationship between TnT maximum/0.01 ng/ml.10 The plasma levels of NT-proBNP were diagnosed using the test "proBNP assay" using the Elecsys 2010 (Roche Diagnostics. Manheim, Germany) analyser. The precision of the assay was from 1.8% at 800 pmol/L to 2.7% at 20.7 pmol/L and the detection limits were 0.6 pmol/L and 4130 pmol/L. The conversion ratio of pmol/L to pg/ml was ´8457. The haemoglobin and hematocrit concentrations were determined with the automatic haematological analyser XE-2100 (Symex, Kobe, Japan) and the biochemical measurements were obtained with the Roche/Hitachi Modular analyser (Roche diagnosis, Manheim, Germany). The glomerular filtration rate (GFR) was calculated using the simplified MDRD formula (mL/min/1.73 m2, 186.3 ´ [plasma creatinine]-1.154 ´ [age]-0.203) (the correction factor for women was ´0.742).
Follow-up and Clinical Events
All patients were followed up, obtaining the vital status of all of them. The main events in the study were death for cardiac causes, defined as death due to heart failure and/or sudden death and the need for emergency heart transplant, the decision for which were not influenced by any of the biochemical findings of the study. Patients dying from non-cardiac causes or elective transplant were followed up until death, but this was not considered an event.
Analysis of Results and Statistics
Test the normality of the distribution of the quantitative variables was checked using Kolmogorov-Smirnov test; the variables with abnormal distribution were expressed as medium [interquartile range, IQR], the rest as mean (standard deviation [SD]) for quantitative variables and number (%) for qualitatives. At baseline level, the comparison of quantitative variables among patients with TnT+ y TnT- was performed using the Wilcoxon Student t test for independent samples, as appropriate, and the Fisher's test for qualitative variables. The variables with P<.1 in the univariable analysis, were introduced in the Cox multiple regression for the identification of TnT+ predictors. The Kaplan-Meier analysis and the statistical log rank were used for the description of the accumulated incidence of TnT+ and the differences between groups. The association between levels of TnT and the appearance of events is studied using the Wilcoxon test for independent samples and the receiver operating characteristic curve (COR). The Cox regression analysis was used for the univariable study of event predictors.
The variables with P<.1 in the univariable were introduced in a multivariable Cox model, that was also adjusted by known risk factors (LVEF, class NYHA) and by the baseline characteristics associated in a significant manner with TnT+. The TnT+ and the TnT index were introduced separately into the model. The adherence to the proposed proportionality of risks was checked using logarithmic representations of the accumulated risks, the analysis of the Schoenfeld residuals and the Ln representation (-Ln S[t]) for each variable after its categorization. The event-free survival after the appearance of an initial TnT+ value was studied using Kaplan-Meier curves and the log rank statistic.
A P<.05 was considered significant. The statistical analysis was performed using the statistical software package for social sciences (SPSS v. 14.0 for Windows, SPSS Inc., Chicago, Illinois, USA).
RESULTS
Clinical Characteristics and TnT+
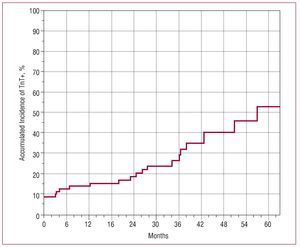
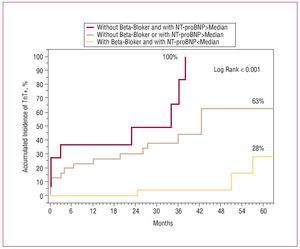
The study population consisted of 80 patients, whose clinical characteristics are set out in Table 1. At the initial visit, 7 patients (8.7%) presented TnT+. The Kaplan-Meier analysis showed an accumulated incidence of TnT+ of 52.8% at 5 years during the follow up (Figure 1). In TnT+ patients, the levels measured presented a median of 0.059 ng/mL (IQR, 0.023-0.100; minimum, 0.013; and maximum, 0.500). At baseline, the variables associated with the appearance of a TnT+ were: raised NT-proBNP levels, deteriorated renal function with greater figures of plasmatic creatinine, and a lower rate of glomerular filtration and a lower percentage of beta-blocker use (Table 1). The aetiology of the cardiomyopathy (P=.44) and the time of evolution of the disease since diagnosis was similar in patients with TnT+ as opposed to TnT-(6.4 [4.9] vs 7.3 [5.4] years; P=.491). The interval of time between analyses did not show differences (3.0 [1.9-4.8] vs 3.1 [1.8-5.1] months; P=.640). In a multivariate model, the level of NT-proBNP was associated with a greater risk of TnT+ (P=.021; HR, 1.005, 95% CI, 1.001-1.010) while receiving beta-blockers was a protector and was associated with a lower risk of positivization (P=.001; HR, 0.220; 95% CI, 0.089-0.540), with renal function parameters failing to reach significance (P>.4). Figure 2 shows the accumulated incidence of the TnT+ according the presence or absence of beta-blocker treatment and/or NT-proBNP above the median (839 pg/mL) (log rank <0.001). All (100%) patients with raised NT-proBNP and absence of beta-blockers presented TnT+.
Figure 1. Accumulated incidence of troponin T>0.01 ng/mL (TnT+).
Figure 2. Accumulated incidence of troponin T>0.01 ng/mL (TnT+), in accordance with the presence or absence of beta-blocker treatment and/or NT-proBNP >median (839 pg/mL).
Prognosis and TnT
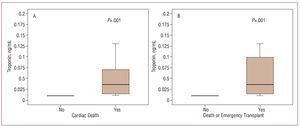
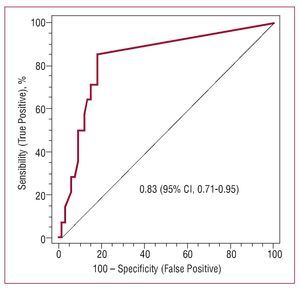
During the clinical follow-up (median, 28.5 months [IQR, 12.9-39.4]), a total of 14 (17.5%) patients presented adverse clinical events: 9 cardiac deaths (2 sudden deaths and 7 due to refractory heart failure) and 5 emergency code heart transplants; and no patients presented acute coronary syndrome. The levels of TnT were the highest in patients developing events (P<.001) (Figures 3A and 3B). The ROC analysis of the levels of TnT showed an area under the curve of 0.83 (95% CI, 0.71-0.95) (P<.001) for the detection of events during the follow up (Figure 4). The optimum cut off point was a detectable value of TnT (>0.01 ng/mL or TnT+), with a sensitivity of 86%, specificity 82%, positive predictive value 50% and negative 96%.
Figure 3. Block diagram showing the values of troponin T in accordance with the presence of absence of death (A) and of death or transplant (B) during the follow-up.
Figure 4. Analysis of the characteristic operator/receptor curve for the levels of troponin T and the appearance of events during the follow-up.
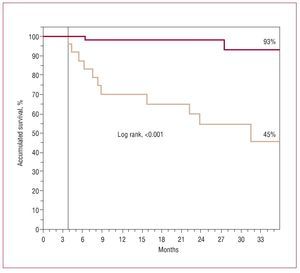
During the follow-up, the adverse events occurred in 12 (50%) of 24 patients with TnT+ compared with 2 (3.6%) of 56 with TnT- (P<.001). Of the patients with TnT+, 7 (29%) died of cardiac causes and 5 (21%) required an emergency heart transplant. The Kaplan-Meier survival analysis (Figure 5) showed that the first adverse event occurred in the fourth month of follow up after positivization of TnT, the survival being significantly decreased among patients with TnT+ (log rank <0.001). The results of the Cox regression analysis for the appearance of events is set out in Table 2; after adjusting the multivariable model, a value of TnT+ (>0.01 ng/mL) was the most powerful predictor of adverse events (model 1), and when considering the TnT index (model 2), this showed that each increase of 0.010 ng/mL in the TnT was associated with a 36% increase in the risk of adverse events (Table 2).
Figure 5. Kaplan-Meier survival curves for the appearance of events from the first value of troponin T >0.01 ng/mL (broken line) versus all the troponin values T£0.01 ng/mL (red line).
DISCUSSION
This study evaluated the usefulness of monitoring TnT in an outpatient population with nonischemic HF and severe systolic dysfunction. In this population we found that: a) the frequency of positivization of TnT occurs in a high population of patients during a broad time range; b) the risk of positivization was greater in the presence of greater severity of the clinical situation and greater myocardial stress (NT-proBNP) while the use of beta blocker therapy was associated with lower levels of risk; c) the appearance of a TnT+, even at low levels, led to a poor prognosis, which is independent of other clinical, analytical and ECG variables; and d) after the positivization of the TnT, the occurence of the adverse events occurs after several months (>4 months), which could be interpreted as an opportunity to treat these patients more intensely.
Prevalence, Frequency, and Determinants
The majority of the information is drawn from transversal prevalence studies, that show variable percentages (15%-80%) depending on the population evaluated.4,6-11,16-20 Most studies were performed with hospitalized populations with acute HF, where the greatest prevalence is reported (45%-80%).4,6-9,16-19 There are fewer data gathered from outpatient populations with stable HF: Missov20 (n=33; 55% ischemic) found a prevalence of 15%, Perna et al10 (n=115; 50% ischemic) of 32% and Hudson et al11 (n=136; 62% ischemic) of 24%; which suggests a lower prevalence in the out-patient setting. Our study showed a prevalence at inclusion of only 9%, which could be due partly to the absence of coronary disease, as some authors have suggested the frequency is higher in the presence of ischemic aetiology.7,21
On the other hand, different works have shown an association between TnT+ and lower LVEF, worse NYHA class, greater BNP, and deterioration of renal function.11,16
These associations suggest that the variability of prevalence is also a consequence of the differences in the severity of the HF syndrome. Thus, recently Miller et al describe a frequency of TnT+ of 54% in 190 out-patient patients, most of them with ischemic aetiology (55%).12 However, this work included patients who had recently been hospitalised with acute HF, all of whom were in NYHA III-IV and with associated deterioration of renal function (TFG, 45 mL/min/1.73 m2). Compared to this, our population did not present recent hospitalizations, the majority (64%) were in NYHA II and the GFR was clearly greater (74 mL/min/1.73 m2). In the light of all these findings, it seems to be that the characteristics of the population and the severity of the HF syndrome determine the variability in the prevalence described for TnT+.
The greatest contribution of our work is the description of the frequency or positivization of TnT during the long-term follow-up. The accrued frequency is high (53%) but during a wide range of time (5 years). Previously, only the work carried out by Miller et al had contributed data regarding monitoring TnT.12 However, as has been indicated, in this study, the initial prevalence was already high, being 54%, and reaching 71% after 2 years of follow-up. The increased severity of the HF syndrome appears to be responsible for the high initial prevalence, however, the annual rate of incidence was similar; being 8.2% in the work by Miller and 8.9% according to our findings.
An important finding of our study is the decreased risk of the appearance of a TnT+ in patients receiving treatment with beta-blockers, which, together with the increased risk associated with NT-proBNP, was independent after the multivariable adjustment. The association between the levels of NT-proBNP and TnT has been described in a standard manner by several authors,9,17,19 showing a greater degree of ventricular stress. However, none of the studies have shown the protective effects of beta-blockers on positivization of TnT, and consequently of myocyte necrosis. It is a known fact that circulating catecholamine are predictors of the severity and prognosis in HF22 and that in other clinical situations, a high adrenergic influx can lead to cardiomyopathy with myocyte necrosis even in the absence of coronary disease.23,24 In experimental models the stimulation of the b1 receptors leads to necrosis and apoptosis, leading to progressive of dysfunction and adverse ventricular remodelling.25-27 In animal models of HF, blocking the b1 receptors protected against necrosis and apoptosis of the cardiomyocytes, suggesting this blockade as one of the mechanisms explaining the benefits of beta-blockers.28,29 Our Study illustrates this protection in a clinical setting, regardless of the NT-proBNP level, and supports that in all the aetiopathogenic mechanisms suggested, excess b1 stimulation might be the main cause contributing to nonischemic myocardial damage in HF.
Prognosis
Our work confirmed the significant association between the presence of TnT+ levels and a worse prognosis in patients with nonichemic HF. During recent years, the presence of TnT+ in hospitalized patients with acute HF has been related to a greater frequency of death, transplant and rehospitalization due to HF.4-8 In the outpatient setting, raised levels have also been associated with adverse events.10-12 In our work, the levels of TnT detected were minimum (range, 0.013-0.500) and independently of the amount, the presence of measurable levels (>0.01 ng/mL) is associated with increased risk, which was independent of other clinical, analytical, and ECG variables. The prognostic value of TnT, even minimum detections, has also been shown by others, and in the case of the TnT the majority of authors describe an increase risk after it is detected.5-7,10,11,17
One interesting observation is the timeline of appearance of the events after TnT+ has been detected. In earlier studies, the appearance of events is earlier and described during the first month, however, the results of this are not comparable as these are prevalence studies on hospitalized populations with predominantly ischemic aetiology.6,8,10,11 In our study, the events occurred as from the fourth month after TnT+ was detected, although we cannot rule out the possibility that close monitoring meant this was detected sooner before the occurrence of the first event. In any case our work shows that in the outpatient population with HF, the detection of TnT+ can open a therapeutic window during which the treatment given to patients can be intensified, thus helping to improve their prognosis.
The results obtained from this study draw attention to the importance and usefulness of monitoring TnT when following up outpatients with chronic stable HF. In our opinion, from all the findings described, it is evident that TnT is a useful tool in this area. In the future, the use of more sensitive methods for detecting TnT and their integration together with the measurement of NT-proBNP could contribute to new applications. One advantage of TnT is the absence of a variable cut-off point or population dependent cut-off point, meaning that a single detection is associated with increased risk, while the cut-off point for BNP is dependent on the population being tested.30
In our analysis, both were quantitative predictors of risk, which, together with the numerous works identifying both as independent prognostic markers, suggests there is a need to use both jointly.
Limitations
The main limitation of the study was the selective nature of the population, which could have led to a bias that interfered with the extrapolation of the results to other populations. On the other hand, the analytical monitoring was not standard and, although programmed every 3 months, it must be acknowledged that there was a variable inherent to the healthcare practices themselves, neither could we exclude that although all the samples were outpatient and scheduled, some were taken during phases of decompensation. Lastly, the observational nature of the association between beta-blockers and a decreased elevation of TnT, does not enable us to infer the protective role of the same, but establishes the need to investigate this aspect more deeply.
CONCLUSIONS
In outpatients with stable chronic HF of a nonischemic nature, the detection of TnT, even at low levels, means an increased risk of adverse cardiac events, which is independent of other clinical, analytical and ECG variables. Treatment with beta-blockers had a protective effect, which was independent of the level of NT-proBNP.
ABBREVIATIONS
HF: heart failure
IQR: interquartile range
NT-proBNP: N-terminal probrain natriuretic peptide ROC: receiver operating characteristic
Tn: troponin
TnT: troponin-T
SEE EDITORIAL ON PAGES 667-9
This work has been partly financed with resources from the Heart Failure Research Network REDINSCOR. Ministry of Health and Consumers, dossier number RD06/0003/0013.
Correspondence: Dr. D.A. Pascual Figal.
Servicio de Cardiología. Hospital Universitario Virgen de la Arrixaca. Ctra. Madrid-Cartagena, s/n. 30120 Murcia. España.
E-mail: DomingoA.Pascual@carm.es
Received November 20, 2007.
Accepted for publication March 6, 2008.