Within just a few years, transcatheter therapies targeting functional tricuspid regurgitation (TR) have evolved into one of the most discussed topics in structural heart interventions. In light of the remarkable symptomatic and functional benefit observed after edge-to-edge transcatheter tricuspid valve repair (TTVR) in nonrandomized analyses, the field has seen a rapid evolution in terms of techniques, devices, and clinical applications.1 Taking these early data into account, the 2021 European Society of Cardiology/European Association for Cardio Thoracic Surgery guidelines for the management of valvular heart disease provide a class IIb (level of evidence: C) recommendation for transcatheter treatment of symptomatic functional severe TR in inoperable patients at dedicated heart valve centers. 2
Meanwhile, 2 edge-to-edge TTVR devices (TriClip, Abbott, United States and PASCAL, Edwards Lifesciences, United States) and 1 direct percutaneous annuloplasty device (Cardioband, Edwards Lifesciences, United States) obtained the CE mark for TR treatment. The TriClip device is specifically designed to overcome the challenges of transfemoral tricuspid valve treatment encountered during the first attempts at edge-to-edge TTVR with the MitraClip (Abbott, United States) in off-label use, such as steering toward the valve after entering the right atrium, orientation above the tricuspid valve, and leaflet grasping. Although the general design and handling appears similar to those of the widely used MitraClip, the TriClip offers important novel features, including modifications of the steerable guide and delivery system, including an additional steering knob significantly improving perpendicular alignment toward the tricuspid valve.
In a recent article published in Revista Española de Cardiología, Freixa et al.3 report the very initial experience obtained with the TriClip at 4 Spanish centers after limited release of the device on the national market. Thirty-four patients were treated and followed up for 3 months with remarkable results considering that the TriClip was just added to the therapeutic armamentarium: mild-to-moderate TR on echocardiography at discharge and after 3 months of follow-up in 91% and 80% of patients, respectively; no relevant safety issues; and nearly 90% of patients were in New York Heart Association functional class ≤ 2 on assessment after 3 months.
The authors should be congratulated for their joint effort to report these data right after implementing the device at their hospitals as well as the superb procedural and clinical outcomes achieved. While the application of edge-to-edge TTVR spreads rapidly, the present results underline that the TriClip can be applied safely and effectively to treat TR at centers with sufficient prior experience in transcatheter heart valve interventions and clip-based mitral valve interventions.
However, while it is good to know that we have a reliable edge-to-edge TTVR technology in our hands, the (long-term) success of tricuspid valve interventions as well as the further evolution of this technique within the broader context of heart failure therapies will also depend on factors other than device performance and interventional teamwork in the operating room. Given the advanced stages of right heart failure and complex clinical scenarios in most patients considered for transcatheter TR treatment, careful patient selection based on a multidisciplinary Heart Team discussion as well as preprocedural optimization of the patient's condition and continuous monitoring of patients after the procedure, preferably within a heart failure clinic, are just as important.
To this end, defining the mechanisms and pathophysiological context underlying functional TR in a given patient prior to procedural planning is necessary but is often neglected in clinical practice. Although interpretation of average values in the present analysis is limited due to the rather small number of patients, it is tempting to speculate which patients were selected by Freixa et al.3 as first candidates for TriClip implantation after market release. On average, left ventricular systolic function was preserved in the present patient sample, as was right ventricular function based on longitudinal function and right ventricular ejection fraction. Nearly one third of patients had previous left-sided valve surgery, but we are not given sufficient information to classify pulmonary hypertension in the present cohort. Despite its prognostic importance,4 right heart catheterization was omitted in almost half of the patients, as echocardiography did not reveal evidence of left heart disease according to the authors. Yet, in those patients who underwent right heart catheterization, invasively measured systolic pulmonary artery pressure argued against severe pulmonary hypertension. From an anatomic point of view, the right atrium was significantly dilated given a median right atrial area of 28cm2 in the patient sample and a reference value of 16.2cm2 (95% confidence interval, 15.8-16.6) according to published data sets in adults.5 In contrast, even though echocardiographic parameters are not indexed by body surface area in the present manuscript, right ventricular dimension were relatively preserved. Assuming a mean body surface area of 1.7 m2 and reference values for right ventricular end-diastolic area as proposed by the European Association of Cardiovascular Imaging,6 right ventricles were, at least on average, not severely dilated. Compared to other reports on edge-to-edge TTVR, the percentage of patients with cardiac implantable electronic devices was low and only 1 patient had a transvalvular lead.
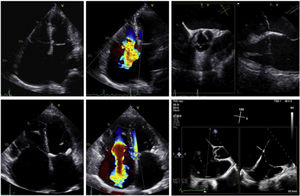
When interpreting these morphologic and functional data, one may conclude that the edge-to-edge TTVR analysis by Freixa et al.3 addressed, at least in part, patients with an atrial functional TR. Atrial functional TR is increasingly being recognized as a separate phenotype of TR, which is distinguished from primary TR and ventricular functional TR by a distinct morphology of the right heart chambers and tricuspid valve apparatus on cardiac imaging (figure 1). The pathophysiological hallmark of atrial functional TR is a loss of leaflet coaptation due to tricuspid annular enlargement in the setting of a significantly dilated right atrium. In contrast to ventricular functional TR, configuration of the right ventricle at its mid and apical portion is normal, whereas its basal portion is mildly dilated even in most patients with atrial functional TR. As a consequence, tricuspid valve leaflet angles are shallow and there is almost no degree of leaflet tethering. Early data on atrial functional TR indicate that this TR phenotype is primarily observed in patients with long-standing atrial fibrillation and heart failure with preserved ejection function,1,7 which seems plausible from a pathophysiologic point of view. An urgent question that arises from this is whether interventional strategies targeting tricuspid annular dilatation are a potential novel therapeutic option in these patients. Clearly, the anatomy in atrial functional TR can be well addressed by direct percutaneous annuloplasty devices, such as the Cardioband. However, the tricuspid valve morphology in atrial functional TR is also suitable for edge-to-edge TTVR, because coaptation gaps are moderate in most patients (as also observed in the manuscript by Freixa et al.3) and shallow tricuspid valve leaflet angles may enable an indirect annuloplasty effect by leaflet approximation.
Phenotypes of secondary (functional) tricuspid regurgitation (TR) on echocardiography. Atrial functional TR (top row) is characterized by tricuspid annular dilatation due to an enlargement/remodeling of the right atrium. Except from a small increase in basal diameters in most patients, the dimensions of the right ventricle (particularly at its mid and apical portions) are within the normal range. In contrast, patients with ventricular functional TR (bottom row) display both tricuspid annular dilatation and marked tricuspid valve leaflet tethering. Parallel to an enlargement of the right atrium, marked remodeling and dilatation of the right ventricle at its basal, mid and apical portions are evident on echocardiography. The latter phenotype is particularly observed in patients with left-sided myocardial or valvular disease, pulmonary disease and right ventricular myocardial diseases.
The advent of transcatheter therapies targeting functional TR expands the role of structural heart interventions in the setting of chronic heart failure remaining symptomatic despite guideline-directed medical therapy. Although we have to await data from randomized clinical trials in this field, transcatheter interventions for functional TR have strong potential to broaden our horizon in patients with chronic right heart failure. Edge-to-edge TTVR and other percutaneous techniques addressing TR not only provide us with a novel therapeutic option in patients in whom we otherwise struggle with current pharmacological management. At the same time, they may improve our understanding of cardiac and extracardiac implications of right heart failure. The journey has just begun. The work be Freixa et al.3 is reassuring as it confirms that we are travelling safe.
FUNDINGNo funding received.
CONFLICTS OF INTERESTP. Lurz has received institutional grants from Abbott Medical, Edwards LiveSciences and ReCor.