Keywords
INTRODUCTION
Cardiovascular disease is still the leading cause of death in Spain.1 Primary prevention, by means of detection and treatment of cardiovascular risk factors (CVRF), is one of the most important preven tive strategies.2
Hypercholesterolemia is one of the main modifiable CVRF,2 together with smoking, diabetes mellitus (DM), and hypertension. Drugs, mainly statins, are available that efficiently reduce plasma cholesterol concentrations and cardiovascular events.3 Their efficacy in secondary prevention is unquestioned and their use in these patients is a priority.3 This efficacy is less in primary prevention, especially relating to the absolute reduction in risk,3 and it has not yet been clearly demonstrated in women4,5 or older persons.4,6,7
The prevalence of hypercholesterolemia is high, with 23% of the Spanish population having figures above 250 mg/dL,8 and the prescription of statins has experienced an important increase over recent years.9 This high prevalence, coupled with the low absolute reduction in risk with statins in primary prevention, has led to their use being encouraged4,10
in patients with hypercholesterolemia and a high cardiovascular risk (CVR), mainly as a result of estimations from functions based on prospective studies.4 Another argument favoring prioritizing the use of statins is that the risk:benefit ratio of lipid-lowering therapy in primary prevention has only been shown in patients with a 10-year coronary risk ≥13%.11
Currently in Spain there exist 3 functions to estimate a high CVR: the Framingham-Wilson function,12 the Framingham-REGICOR calibrated function (Registre Gironí del COR),13 and the SCORE function (Systematic COronary Risk Evaluation).14 The Framingham-REGICOR and the Framingham-Wilson functions are better than SCORE at selecting patients with a high CVR who are candidates for treatment with statins, as they select a higher proportion of patients with hypercholesterolemia,15,16 although other studies17-19 have failed to detect clear differences in this respect. Additionally, no studies have evaluated whether the prescription of statins to patients with hypercholesterolemia and a high CVR estimated according to the above mentioned functions differs from what is done in patients with hypercholesterolemia but no high CVR.
The aim of this study was to determine which of the CVR functions (Framingham-Wilson, Framingham-REGICOR, and SCORE) best classifies patients with a high CVR and hypercholesterolemia who receive treatment with statins and to study the factors related with the prescription of these drugs in primary care.
METHODS
Type of Study
We undertook a descriptive, cross-sectional study within the framework of a study on the prevalence of CVRF.20 This study was carried out in 2 urban health centers in the city of Barcelona, covering a population of 35 275 patients with a medium-low socioeconomic level.
Participant Selection
Participants were selected by simple random sampling among the catchment population. All the participants were aged 35-74 years and had no previous cardiovascular disease (ischemic heart disease, cerebrovas cular disease, or peripheral arterial disease in the lower limbs).
Measurements
The data were collected during the first half of 1998, although the results of this study refer to the cross-section taken after 5 years during the first half of 2003, before the generalized use of cardiovascular risk functions.
The study variables included the following:
1. Age and sex.
2. Prescription of statins if the clinical history recorded the chronic prescription (a minimum of 6 months during the last 12 months) of any of the drugs coded as C10AA in the World Health Organization Anatomical Therapeutic Chemical Clasification.21 Cardiovascular risk was calculated using the last available value of total cholesterol before the start of statin therapy.
3. A high CVR, measured with the following functions:
- Framingham-REGICOR. The patient was considered to have a high CVR if the 10-year risk was ≥10%.
- Framingham-Wilson. A cut-off point of ≥20% at 10 years.
- SCORE. The patient was considered to have a high CVR if the 10-year risk was ≥5%. The SCORE model for low risk countries was used.
4. CVRF. The definition criteria have been given previously,20 and the following were considered: smoking (considering as smokers those persons who smoked any number of cigarettes daily and ex smokers those who had quit within the previous year22); hypertension (classifying the patients as hypertensive if they were taking antihypertensive medication or had 3 consecutive blood pressure measurements ≥140/90 mm Hg,22 and recording the systolic and diastolic blood pressure figures22); confirmed hypercholesterolemia if the patient had 2 measurements ≥250 mg/dL on at least 2 occasions, and recording the values of total cholesterol and high-density lipoprotein cholesterol (HDL-C)22; DM according to the criteria of the American Diabetes Association and the World Health Organization, adopted by the Spanish Society of Family and Community Medicine,23 ie, clinical symptoms together with a random glucose measurement >200 mg/dL, 2 baseline plasma glucose measurements ≥126 mg/dL or a 2-hour oral glucose tolerance test ≥200 mg/dL. Patients already diagnosed with DM or who were receiving treatment with insulin or oral antidiabetic agents were also included.
Statistical Analysis
This analysis was done with SPSS, version 12.0. The proportions were compared using the c2 test and the means with the Student t test or the corresponding tests if the application conditions were not fulfilled. Study of the factors related to statin prescription was done by calculating the odds ratio (OR), accompanied by its 95% confidence interval (CI), considering such factors to be a high CVR with Framingham-REGICOR, Framingham-Wilson and SCORE, age (classified in 2 groups: <65 and ≥65 years), sex, smoking (smokers and non smokers), hypertension, hypercholesterolemia, and DM, also categorized dichotomously. The sample size was calculated using the GRANMO program,24 accepting an alpha error of .05 and a beta error of .75 in a bilateral contrast. At least 204 persons with hypercholesterolemia were required in order to detect a difference of ≥0.13 and assuming an expected proportion of hypercholesterolemia of 0.40.15 The level of rejection of a null hypothesis was alpha <.05 in all cases.
RESULTS
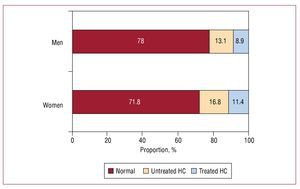
The mean age of the 804 patients included was 56 years, with 59.2% women. Table 1 shows the other main characteristics. Confirmed hypercholesterolemia was diagnosed in 25.6% (95% CI, 22.7-28.8) of the patients, with a greater proportion of women (28.2%) than men (22%), as can be seen in Figure 1 (c2, P=.048). A high CVR was present in 12.4% of the patients according to Framingham-REGICOR, 20.4% with Framingham-Wilson and 20.1% with SCORE (Table 2).
Figure 1. Proportion of patients with treated and untreated hypercholesterolemia (HC) according to sex. Significant differences in the proportion of patients with a diagnosis of HC, treated or untreated (c2, P=.048).
Statins had been prescribed to 83 patients (10.3%; 95% CI, 8.4-12.6). The proportion of patients with hypercholesterolemia treated with statins was therefore 40.3% (95% CI, 33.8-47.1), with no significant differences between sexes (Figure 1).
Table 2 shows that the proportion of patients with definite hypercholesterolemia was greater in the patients with a high CVR according to the Framingham-REGICOR (41%) and Framingham-Wilson (37.8%) functions than in the patients without a high CVR (c2, P<.001). However, with SCORE (31.8%) no differences were found (c2, P=.201). Similar findings (Table 2) can be seen concerning the mean concentrations of total cholesterol: higher figures in the patients with a high CVR with Framingham-REGICOR and Framingham-Wilson (Student t test, P<.001), but no significant differences with SCORE (Student t test, P=.555). As regards HDL-C, all 3 functions selected patients with significantly lower values (Table 2), although Framingham-REGICOR and Framingham-Wilson selected a population with lower HDL-C concentrations (about 12 mg/dL) than SCORE (5 mg/dL).
Table 3 shows the raw OR of the variables associated with the prescription of statins. Prescription was lower in those younger than 65 years of age (OR=0.51; 95% CI, 0.32-0.81). It was also lower in men and in smokers, although the differences were not statistically significant. It was significantly higher in the patients with hypertension (OR=1.89; 95% CI, 1.20-2.99) and hypercholesterolemia (OR=11.01; 95% CI, 6.55-18.53), but not significantly higher in the patients with DM. In the analysis adjusted for the other variables (age <65 years, sex, smoking, hypertension, DM, and hypercholesterolemia), only hypercholesterolemia retained its significance (OR=9.10; 95% CI, 5.48-15.01). Statins were being taken by 16% of the patients with a high CVR according to Framingham-REGICOR, a proportion that was 9.5% in the patients without a high CVR, a significant difference (c2, P=.046; OR=1.81; 95% CI, 1.01-3.27). However, no significant differences were found with the Framingham-Wilson (OR=1.47; 95% CI, 0.87-2.47) and SCORE (OR=1.09; 95% CI, 0.50-2.37) functions.
DISCUSSION
The results of this study confirm that the proportion of patients with hypercholesterolemia and the mean levels of total cholesterol are higher in patients classified as having a high CVR using the Framingham-REGICOR and Framingham-Wilson functions, but not the SCORE function. The prescription of statins was greater in the patients with a high CVR using Framingham-REGICOR as compared with Framingham-Wilson and SCORE. Considering that cardiovascular risk functions are used to prioritize the use of statins4,10 in primary prevention patients, the Framingham-REGICOR function would be more useful to rationalize the use of these drugs.
The proportion of patients with confirmed hypercholesterolemia (cut-off point, 250 mg/dL) was similar to that reported in the review by Medrano et al,8 and it also coincides in the distribution by sex.8 Fewer than half the patients with hypercholesterolemia were receiving statin therapy, a slightly higher proportion of treated patients than in the study by Ramos et al.25 We found no differences between the sexes regarding statin therapy (Figure 1) in the patients with definite hypercholesterolemia, which agrees with the study by Bonet et al,26 although another study did find that the women received more lipid lowering drugs.27 Notwithstanding this, analysis according to sex of statin prescription in all the patients in primary prevention, given that statins can be used with lower levels of cholesterol if there exists a high CVR or more intensive recommendations are followed,4 showed that the prescription was lower (Table 3) in the men than the women, though the difference was not statistically significant. Interestingly in this respect, the efficacy of statins in primary prevention in women has not in fact been demonstrated, despite carrying out meta-analysis techniques.5
Framingham-REGICOR, and to a lesser extent Framingham-Wilson (as expected, since they are very similar functions), were better than SCORE at selecting the population with a high CVR susceptible to statin therapy (Table 2), given that they both included a greater proportion of patients with hypercholesterolemia, with higher concentrations of total cholesterol and lower concentrations of HDL-C. An earlier study15 found that the proportion of patients with hypercholesterolemia was lower with SCORE (24.7%) than with Framingham-REGICOR (40%) and Framingham-Wilson (38.4%), although the values of total cholesterol and HDL-C were not analyzed. The study by Gil-Guillén et al16 analyzed the cases of discrepancy in the high-risk patients between SCORE and Framingham-REGICOR; these authors also found important differences in the above mentioned lipid values. Although the patients with a high CVR according to SCORE had a significantly (Table 2) lower level of HDL cholesterol (similar to Framingham-REGICOR and Framingham-Wilson, but with a much smaller difference), it is important to recall that the SCORE function does not include HDL-C because it fails to improve the predictive capacity of the function.14 Using SCORE instead of Framingham-REGICOR would result in fewer statins being given to the patients who, paradoxically, most need them.
Surprisingly (Table 3), statins were prescribed less in those younger than 65 years of age, which is precisely the age for which most evidence is available.3,4 A similar phenomenon was seen in the men and the smokers, about which similar observations can be made,3,4 though the differences were not statistically significant. The explanation of this paradox might be that the most determining factor in the prescription is the diagnosis of hypercholesterolemia (OR=11.1), with a greater prevalence in women. More coherent are the results in the case of hypertension and DM, although only the former reached statistical significance. After adjusting the effect for the other variables (Table 3), only a diagnosis of confirmed hypercholesterolemia was significantly associated with the prescription of statins.
The patients with a high CVR as estimated with the Framingham-REGICOR function received (Table 3) more statins than those with a high CVR estimated using the other 2 functions. Table 3 does not include the adjusted OR, as the functions studied already included the rest of the risk factors in Table 3, in order to avoid overadjustment. Previous studies using the Framingham function coincide with these results.27,28 With SCORE, however, the proportion of patients treated with statins was very similar for the patients with a high CVR (10.6%) and those without (9.8%).
Study Limitations
The proportion of women was higher than men, which is usual in other population-based studies in our setting.29 The inclusion of patients who were being attended should not be considered a bias, as the center has been in operation for over 10 years and 83.8% of the population were seen during the last year.30 The assigned population and the attended population are methods that are preferable to the censored population in primary care, after a study carried out by the Fundación Jordi Gol y Gurina.31 The calculation of cardiovascular risk with Framingham-REGICOR and SCORE was generalized in 2003,13,14 and it is not therefore likely that the prescription of statins has been influential, as the cross-section cut of the study was done beforehand. Nevertheless, the extrapolation of these results to other populations should be made with caution, as this was not a strict multicenter study, and it may be interesting to carry out similar studies in other populations with different prevalences of CVRF and cardiovascular disorders.
Clinical Implications
Several different autonomous communities in Spain (Catalonia, Basque Country, Balearic Isles, Navarre) have officially adopted the use of the Framingham-REGICOR function. However, the debate still exists as far as the scientific societies are concerned.4 The Program for Preventive Activities and Health Promotion support2 the use of SCORE in spite of the fact that the validation of REGICOR had already been published.32 The Spanish
Interdisciplinary Committee for Cardiovascular Prevention,33 whilst they were in favor of SCORE in 2004, made it clear that decisions should be made according to the local adaptations and validations until such time as their own functions were available.4
CONCLUSIONS
In summary, the Framingham-REGICOR calibrated function is better than the Framingham-Wilson and SCORE functions in patients with a high CVR who receive treatment with statins, for 2 reasons: it categorizes a higher proportion of patients with hypercholesterolemia (in whom statin treatment has been shown to be effective) and of patients who receive treatment in clinical practice. This fact contributes making the case for adopting the Framingham-REGICOR function, wich is also the only function that has been validated in Spain.32
ABBREVIATIONS
CVR: cardiovascular risk
CVRF: cardiovascular risk factors
DM: diabetes mellitus
HDL-C: high-density lipoprotein cholesterol
Correspondence: Dr. J.M. Baena Díez.
Instituto Municipal de Investigación Médica (IMIM). Dr. Aiguader 88. 08003 Barcelona. España.
E-mail: jbaena@imim.es
Received February 3, 2009.
Accepted for publication June 17, 2009.