The recently updated guidelines regarding treatment for patients with non-ST-segment elevation acute coronary syndrome (NSTEACS) recommend initial systematic coronary angiography followed by coronary revascularization, if anatomically feasible, in the management of these patients.1,2 These recommendations were based on the results of different randomized studies3-7 demonstrating that an invasive strategy provided a benefit in the reduction of ischemic events when compared to a conservative strategy where coronary angiography and revascularization were only indicated when spontaneous or inducible ischemia was present. However, the main limitations of randomized studies include how representative the included population are when compared to actual daily clinical practice, whether the results obtained in the participating centers are reproducible in other settings and whether the conclusions of these studies can be suitably applied in daily clinical practice.
In the present issue of Revista Española de Cardiología, Bodí et al8 contribute valuable information on the daily treatment of patients with NSTEACS. In a nonrandomized observational cohort study, the authors compare 2 series of patients admitted with a diagnosis of NSTEACS. In the first series, the patients were evaluated via a more conservative strategy where the use of coronary angiography was based on detecting spontaneous or induced ischemia in the non-invasive tests, whereas in the second series, carried out immediately after the first series, the patients were managed with an initial systematic intention to treat invasively. The coronary angiography (61% vs 73%) and predischarge revascularization rates (33% vs 48%; the most frequent being angioplasty, 21% vs 35%) although statistically significant did not greatly differ between the 2 groups of patients. Although no significant differences were found in the incidence of major ischemic events, the patients who underwent a more invasive initial strategy had fewer postdischarge readmissions, with less need for additional revascularization procedures during follow-up. Furthermore, in the multivariate analysis, the initial invasive treatment was an independent protective predictor of the appearance of minor ischemic events or any of the events analyzed, with an adjusted risk reduction of 50%. An interesting and intriguing aspect is the divergent trajectories the events followed during follow-up in both series.
The study by Bodí et al may more realistically reflect daily clinical practice regarding treating patients with NSTEACS than the random studies. Although the inclusion criteria were similar to those of the random studies (depressed ST segment and positive markers of myocardial injury), a greater number of patients in the study by Bodí et al were diabetic and the elevation rates of the troponin I values were much higher than those presented by the patients included in 2 of the random studies,5,6 suggesting the inclusion of high-risk patients. Furthermore, the differences between the coronary angiography and revascularization rates during hospitalization between the 2 cohorts are much lower than the differences documented in the different randomized studies. This aspect may explain why the incidence of major events in the 2 series in the present study did not reach significant difference. This reflects procedures which are much more clinically oriented (semi-conservative in contrast to semi-invasive) and far from the large differences in the number of invasive procedures which, for research purposes, were carried out in the 2 arms (conservative and invasive) of the different randomized studies. However, the data of Bodí et al can be interpreted in practical terms. A more invasive management in 100 consecutive patients with high-risk NSTEACS would avoid the implementation of 23 exercise stress tests due to doing 12 catheterizations, 12 angioplasties, and 1 extra coronary surgery, by which 3 deaths, 7 readmissions, and 5 new revascularizations would be prevented during follow-up.
Mortality in the present study was much higher than that found in the randomized studies mentioned. It should be borne in mind that this concerns a group of nonselected high-risk patients reflecting actual daily clinical practice. Such mortality is similar to that found in recent Spanish registries.9,10 The older age of the included patients, the high prevalence of diabetic patients (35%) and the positive troponin rates corroborate the high risk in the patients in Bodí et al's study. Furthermore, the coronary angiography rate in the group treated with a conservative strategy was 63%, which reflects the high frequency of detectable residual ischemia in the non-invasive tests. Although there were differences in the absolute values of mortality between the 2 series (9% in the most conservative series vs 6% in the most invasive), it would be necessary to include a greater number of patients to detect significant changes.
It is important to mention some of the limitations of the present study. The administration of glycoprotein IIb/IIIa receptor inhibitors remained almost exclusively restricted to the time of carrying out percutaneous coronary intervention, after several days of hospitalization. Glycoprotein IIb/IIIa inhibitors were not used at admission. This fact may have reduced the benefits in the patients subject to the most invasive strategy. One of the situations where glycoprotein IIb/IIIa inhibitors have demonstrated their greatest reduction in the incidence of ischemic events is in the patients with NSTEACS who, being under treatment with these drugs, are subsequently submitted to percutaneous revascularization.11 There were no differences in the time elapsed up to coronary angiography nor in the number of in-hospital days between the 2 groups of patients, which possibly reflects some of the special features of our health system.
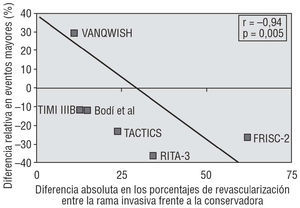
Two important conclusions can be drawn from Bodí et al's study: first, coronary angiography and coronary revascularization in a series of patients in which a routine initial invasive strategy was planned remained limited to 73% and 48% of the patients, respectively. These rates possibly reflect the actual daily clinical practice of an invasive initial strategy with a nonselected series of patients admitted with a diagnosis of NSTEACS. Second, even though the differences in the invasive procedure implementation rates were not very marked between the 2 series, the incidence of ischemic events indicate that even discrete changes in the strategy (from semi-conservative management to semi-invasive management) can have prognostic clinical meaning. In the patients diagnosed with NSTEACS, a benefit gradient seems to exist between the revascularization rates and the consequent prognostic advantages. A greater difference between revascularization rates with a conservative strategy and a more invasive one is correlated with a greater reduction in the incidence of ischemic events (Figure).
Figure. Relationship between differences in revascularization in the invasive arm versus the conservative arm and the reduction in major cardiac events (death or non-fatal infarction).
In conclusion, this study corroborates the fact that in daily clinical practice the management of patients admitted for non-ST-segment elevation acute coronary syndrome (with signs of ischemia in the electrocardiogram or elevated markers of myocardial injury) a routine initial invasive strategy with coronary angiography followed by revascularization offers prognostic advantages over a strategy guided by symptoms or by induced ischemia.
Correspondence: Dr. J.A. Gómez-Hospital.
Unidad de Hemodinámica y Cardiología Intervencionista.
Hospital Universitari de Bellvitge.
Feixa Llarga, s/n. L'Hospitalet del Llobregat. 08970 Barcelona. España.
E-mail: 26587jgh@comb.es