Keywords
INTRODUCTION
The mechanical properties of the arteries are of fundamental importance in the functions they perform as part of the cardiovascular system. Knowledge of these properties is vital if we are to understand the physiology of the circulatory apparatus and to design therapies and techniques for repairing cardiovascular lesions and defects. Since the arteries are physiological conduits subject to internal pressure,1 their mechanical properties are involved in the outcome of the vast majority of treatments for these vessels (the repair of arterial ruptures or dissections, endarterectomy, angioplasty, stents, by-passes, etc).
The thermomechanical response of human arteries remains little understood despite the increasing importance given to temperature in clinical procedures in recent years. Some types of heart surgery or surgical procedures involving the major arteries (aortic dissection, heart transplant, coronary artery surgery, valve surgery, repair of congenital heart defects, etc) are performed using systemic hypothermia; sometimes even profound hypothermia is induced (18-20oC) with extracorporeal circulation.2 The liquids used for the preservation of organs for transplantation, and in conventional surgery, are usually used at a temperature of 4-18oC. Other therapies involve hyperthermal conditions, such as perfusion with warm solutions for the treatment of soft tissue tumors in the arms and legs, and in the sealing of coronary dissections with radiofrequency-heated balloons.3-5
The studies performed to date,6-8 however, have not adequately taken into account the thermomechanical behavior of artery walls, which is very complex9,10 (non-linear viscoelasticity, incompressibility, anisotropy, etc) and difficult to describe with simples indices. Although different variables have been proposed that explain certain arterial properties with differing degrees of success, all have their limitations. In addition, to simplify matters, they do not usually take into account the influence of thermal effects. Moreover, many of the experimental data available on the mechanical properties of arteries have been obtained in tests performed under physiological conditions (37oC, 120-60 mm Hg). While such tests provide information within the context of the normal working environment, the small mechanical and thermal ranges involved allow no laws or models to be produced that predict what will happen in other situations. Numerical models have been shown useful in cardiovascular medicine for predicting the behavior of tissues and for the optimization of treatments.9 However, to develop models of arterial thermomechanical behavior that can be applied to clinical situations, experimental data obtained under a wide range of conditions are required; such tests would also allow the responses of diseased vessels to be examined. To date, information of this type has been very scant, especially with respect to human vessels. The aim of the present work was therefore to examine the thermomechanical behavior of the human carotid artery and aorta over a wide range of pressures (0-200 mm Hg) and temperatures (17-42oC) in order to predict repercussions at the clinical level. The study subjects had no apparent vascular disease and were middle aged (aorta donors) or of advanced age (carotid donors); the present comparisons should therefore be read with caution, and certainly, the results should not be used as absolute references. All work was performed at the Dept. of Materials Science of the Universidad Politécnica de Madrid, with the collaboration of the Cardiac Pathology Units of the Puerta de Hierro and Clínico San Carlos de Madrid hospitals.
METHODS
The Studied Arteries: the Aorta and Carotid Artery
The arteries studied were the human aorta and carotid artery. Carotid arteries (11 complete vessels) were obtained from eight individuals who had died of non-atherosclerotic causes. None had been smokers, and none had any history of high blood pressure, diabetes or hypercholesterolemia. The mean age of these donors was 81 (7) years. The donated arteries were therefore theoretically free of vascular disease, but generally came from patients of advanced age.
Four segments of ascending aorta were obtained from four cadavers, all heart donors (mean age 49 [10] years). Given this origin, all were considered theoretically healthy. The longest lengths of vessel possible were extracted in order to facilitate their use in pressurization tests. All vessel samples were obtained after acquiring the permissions required by current legislation.
The carotid artery segments analyzed were 55 (11) mm long and 9.3 mm in diameter; the ascending aorta segments were 63 (12) mm long and 20 (2) mm in diameter. Before extraction of the vessels, all were measured in order to proportionally reproduce their natural state of axial elongation during pressurization tests.
All samples were preserved at a temperature of 4-8oC in cardioplegic solution11-13 (mannitol 60 mmol/L, lactobionic acid 80 mmol/L, glutamic acid 20 mmol/L, sodium hydroxide 100 mmol/L, calcium chloride-2H2O 0.25 mmol/L, potassium chloride 30 mmol/L, magnesium chloride-6H2O 13 mmol/L, histidine 30 mmol/L, glutathione 3 mmol/L; osmolarity 345 mOsmol/kg). All tests were performed within 48 h of vessel extraction.
Histological Analysis
All samples were subjected to histological analysis in order to study the composition and structure of the mid-layer (the layer largely responsible for their mechanical behavior). The distribution of the elastic and muscular fibers were recorded, and the position of any possible atherosclerotic lesions noted. This analysis required the removal of a section from each sample vessel, which was immediately fixed in buffered formol and later stained with hematoxylin and eosin plus orcein. The ratio of elastic/muscular fibers was recorded. Atherosclerotic lesions were graded according to the criteria of the International Committee of the American Heart Association.14,15
Pressurization Tests
The mechanical properties of the vessels were investigated using a pressurization test, and the internal pressure/external diameter curve at different temperatures plotted for each. The aim of this test was to reproduce in vitro the kinds of mechanical stress that might be experienced by the vessels in the living organism under different conditions. Figure 1 shows the apparatus used. All tests were performed inside a transparent, polymethacrylate cell; this allowed the test vessel to be seen at all times and permitted its dimensions to be recorded optically. The external diameter was measured at the center of the segment using a Keyence LS-7500 optical extensometer (precision 0.001 mm). During the test the vessels were submerged in PBS, the tem
perature of which was maintained within ±1oC by an Unitronic 6320200 thermostatically controlled water bath. The temperature of the vessel was measured using a type K thermocouple positioned at a distance of 5 mm.
The arteries were held in the clamps of an Instron 5866 mechanical test apparatus; this was used to obtain the proportional axial elongation recorded before removal. The precision of this axial extension was 0.0001 mm (measured using the transducer incorporated into the apparatus). The lower clamp allowed for the internal pressurization of the vessel with PBS (monitored using a Druck PMP 4000 transducer [precision 0.15 mm Hg]).
All tests were performed with the vessels in a passive state, ie, with no electrical or chemical activation of the vascular wall cells. The tests were performed at 17, 27, 37, and 42oC, and the internal pressure/external diameter ratio determined in each case.
The vessels were attached to the clamps by mechanical and chemical (cyanocrylate) means and first submerged in PBS at 17oC for 10 min. After thermal equilibration, axial elongation was performed so that their proportional length matched that of their in vivo state. The vessels were then conditioned to pressure changes by putting them through 10 cycles of pressurization of between 0 and 200 mm Hg (increasing by 2 mm Hg/s) in order to obtain a stable behavior pattern and repeatable results. A new cycle following the same pattern was then undertaken and the internal pressure/external diameter ratio continuously monitored. At the end of this test phase the PBS was warmed to 27oC (and successively to 37oC and 42oC) and the same steps repeated. The mean duration of a complete test (ie, covering all four temperatures) was 3 h. At the end of the test, a piece of each artery was fixed in formol for histological analysis (see above).
Thermomechanical Analysis
The internal pressure/external diameter curves for the different temperatures were used to determine the thermomechanical behavior of the arteries. This was characterized by the use of two indices: the coefficient of thermal expansion (α), and the Hayashi stiffness parameter (β).16 Together, these provide an adequate idea of the influence of temperature on the behavior of the artery wall. The former provides information on the change in the dimensions of the artery with temperature, while the latter reflects the influence of temperature on arterial rigidity.
The coefficient of thermal expansion measures the change in dimensions experienced by a material with a change in temperature, and is defined as the relative variation of the diameter (ΔD/D) divided by the increase in temperature (ΔT)
α=(ΔD/D)/ΔT(1)
The integration of this equation provides:
D=DRefeα(T-TRef)(2)
where DRef is the diameter at temperature TRef. Equation (2) can then be transformed to provide:
D=D*eαT(3)
where D*=DRefeαTRef. The coefficient of thermal expansion can therefore be obtained simply by fitting experimental data into equation (3).
The rigidity of the walls of the studied arteries was characterized by the Hayashi stiffness parameter. Hayashi et al,16 proposed an exponential equation for describing the relationship between arterial pressure and diameter (p-D):
ln (p/ps)=β(D/Ds1)
where ps is a reference pressure (normally 100 mm Hg)8 and Ds is the diameter of the artery at pressure ps (ln indicates naperian logarithm).
RESULTS
Histological Analysis
The ascending aorta and the carotid arteries are close to the heart; both are elastic arteries.17-19 These become distended during the contraction of the ventricles, transforming the pulsating blood flow produced by the heart beat into a continuous capillary flow; their elastic fiber content is therefore high. The mid-layer of both these arteries is formed by concentric laminas of elastin alternating with smooth muscle and collagen fibers. The differences between the aorta and carotid arteries lie in the dimensions of this mid-layer and the percentage of elastic fibers. The histological analysis showed the aorta to have a significantly thicker mid-layer than the carotid artery (1.47 [0.04] mm compared to 0.22 [0.03] mm). In addition, the aorta was found to have a higher percentage of elastic fibers (50% compared to <35%); these values agree with those typically reported in the literature.17-19
No atherosclerotic lesions were detected. However, given the age of the donors (especially those who donated carotid arteries), age-related alterations were seen, characterized by a profound thickening of the intima associated with an increased number of smooth muscle cells surrounded by variable quantities of connective tissue (type IV lesions according to the American Heart Association). Type IV lesions are degenerative arterial lesions that appear with age14,15; this classification differentiates them from more complicated lesions associated with pathological processes such as fibroatheromas, calcifications, hemorrhages, and thromboses. Some 78% of the carotid arteries examined and 56% of the aortas were thus affected.
Pressurization Test
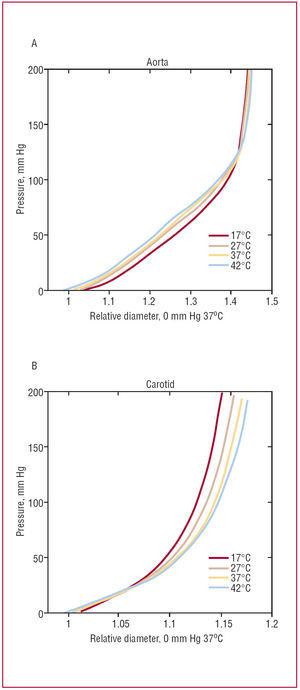
Figure 2 shows the internal pressure/external diameter curves for the two types of artery studied. These curves reflect the variation of the external diameter of the vessels with respect to the pressure exerted on their walls at different temperatures. The mean values for each type of artery are shown. Relative diameters were calculated by dividing the absolute diameter results by the reference diameter (37oC and 0 mm Hg) for each type of artery. This allowed comparisons to be made between the two vessels.
Figure 2. Internal pressure/external diameter curves for different temperatures: (A) aorta, (B) carotid artery. The reference diameter for each vessel was taken as that at 0 mm Hg and 37oC.
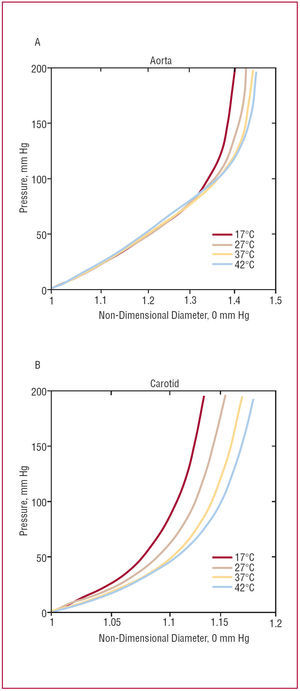
The effect of temperature on arterial behavior is more easily seen, however, when each recorded diameter is divided by a reference diameter for each temperature (at 0 mm Hg). Figure 3 shows the result of this treatment, in which all the curves pass through the origin. The figure shows that the change in relative diameter of the vessels increases with temperature.
Figure 3. Non-dimensional internal pressure/external diameter curves for different temperatures: (A) aorta, (B) carotid artery. The reference diameter for each vessel was taken as that at 0 mm Hg at each temperature.
Thermomechanical Analysis
Coefficient of Thermal Expansion
Figure 4 shows the mean coefficient of thermal expansion for each artery, calculated by fitting the temperature-diameter (T, D) data pairs to equation (3) at each test pressure. In both vessels, the coefficient of thermal expansion is negative at low pressure but becomes positive above a certain thresholdapproximately 20 mm Hg for the carotid artery and 150 mm Hg for the aorta.
Figure 4. Variation of the coefficient of thermal expansion with internal pressure. Bars are standard errors of the mean.
The value of the coefficient of thermal expansion increases progressively with pressure, although the progressive decline in the slope of the curves in Figure 4 would appear to indicate the existence of a saturation point.
Although the trend of the curves was similar, the coefficient of thermal expansion of the aorta was always smaller than that of the carotid artery, and did not become positive until a higher pressure was reached.
The Hayashi Stiffness Parameter
The Hayashi stiffness parameter was obtained for each type of vessel by treating the internal pressure/external diameter curves with equation (4); Figure 5 shows the means and errors for both the aorta and carotid artery. For both vessels the value of the stiffness parameter decreased with temperature, although no significant differences were seen even between the two temperature extremes (17oC and 42oC). Figure 5 shows that the carotid arteries are more rigid than the aorta.
Figure 5. Variation of the Hayashi stiffness parameter with the temperature. Bars are standard errors of the mean.
DISCUSSION
The first study in the literature on the effect of temperature on human blood vessels was that of Roy,20 which was published in 1880. This author, who performed experiments on the arteries of humans, cows and sheep over the 16-54oC interval, reported arterial walls to show the peculiar behavior of contracting when heated and expanding when cooled, ie, they have a negative coefficient of thermal expansion. In 1954, Lawton21 obtained similar results with dog arteries. However, other authors report conflicting results. Dobrin et al22 found no significant influence of temperature on dog arteries, Kang et al4 reported the same for sheep arteries, and Herrera et al23 obtained contradictory results for the coefficients of expansion of rat and pig arteries. Thus, the literature contains little information on the influence of temperature on the behavior of arteries, and what there is inconclusive, and sometimes even contradictory. This confusion may be due to cross-over effects produced by the combined action of the state of mechanical tension (largely a consequence of the internal pressure of the vessel), the temperature, and the state of muscular activation of the vessels examined.
The present work analyzes the effect of temperature on two human arteries (the aorta and the carotid artery) without muscular activation, and the results show that it has an important influence on their behavior.
Increasing temperature led to the arteries becoming more deformable as temperature increased (Figure 3). Although the effect was similar in both types of artery, their mechanical behavior was somewhat different. In absolute terms, the diameter of the aorta grew more than that of the carotid (note the difference in the scales of Figures 2A and B), and showed a more notable initial elastic phase; this is due mainly to the presence of the elastic fibers, which are found in greater proportion in the aorta than in the carotid artery. The greater stiffness seen for the carotid arteries may also be due to the age of their donors; arteries may become more rigid with age.6,8
Figure 5 shows the Hayashi stiffness parameters for both arteries. Higher values indicate lower deformability; as might be expected from the above, the values for the carotid arteries were much higher. In agreement with that shown by the internal pressure/external diameter curves, the rigidity of the vessels decreased with increasing temperature. However, the differences were not statistically significant.
The two arteries behaved similarly in the pressurization test. When the pressure applied was low, the largest diameters were obtained at lower temperatures in both vessels (Figure 2). This confirms their possession of a negative coefficient of thermal expansion when not under load. However, when the pressure was increased to physiological levels the diameter of the vessels increased with temperature. Figure 4 shows the variation in the coefficient of thermal expansion with internal pressure for both types of artery. Despite the dispersion of the results, it is clear that for both vessels the coefficient of thermal expansion is negative at low pressures, gradually rising with pressure until it becomes positive.
This finding of a negative coefficient of thermal expansion at low temperature agrees with the results of Roy20 for the human aorta. Curiously, the value deduced from his work (approximately 7×104oC1) is similar to those shown in Figure 4. Lawton21 obtained similar results in mammalian arteries under no pressure, and explained this in terms of the enthropic origin of the elastic behavior of the artery wall (similar to that of elastomers), which is directly related to the elastic fiber content.
Recently, Herrera et al23 have reported results for pig renal arteries and rat aortas. While the former dilated as temperature increased, the latter contracted. The authors suggest the explanation for these different behaviors to lie in the characteristics of the arteries studied. They postulate that the elastic fibers were behind the contraction seen in the aorta, and that the muscular component of the wall and the state of activation masked their effect in the more muscular renal arteries.
The ascending aorta and carotid artery are both elastic arteries and in the present work were studied without muscular activation. In agreement with that expressed above, it might be expected that they should both show a negative coefficient of thermal expansion. However, and despite the fact that Figure 4 shows the most negative values to be seen in the aorta (which is much more elastic than the carotid artery), the coefficient of thermal expansion depends on their internal pressure. This dependency is complex and needs to be further studied. Recently, we have shown24 that the axial lengthening to which arteries are subjected also affects their thermomechanical behavior; it should therefore be taken into account along with the effect of internal pressure.
Given that the coefficients of thermal expansion shown by the studied aortas and carotid arteries were very different (differences of more than 103oC1 were recorded), variation might also be expected between vessels of other origin, when they come from donors of different age, or when subject to different pathological processes. This might become a problem when vessels with different coefficients of expansion are in contact, eg, at anastamoses, or at the point of contact between an atherosclerotic plaque and the arterial wall. Changes in temperature could lead to high mechanical tensions developing that could result in the deterioration of the points of union, perhaps even to rupturing. In such situations a detailed study of the thermomechanical properties of the elements in contact is required.
CONCLUSIONS
This work is the first to provide experimental data on the thermomechanical behavior of the human aorta and carotid artery, and shows that the combined effect of internal pressure and temperature on the response of the artery is notable. The present tests were performed in vitro and over a wide range of pressures (0-200 mm Hg) and temperatures (17-42oC). The results extend our knowledge of the mechanical properties of arteries and their physiology, and could be of use in the construction and testing of numerical models.
The rigidity of the vessels, reflected in the slope of the internal pressure/external diameter curves, decreases with increasing temperature. However, the differences (measured by the Hayashi stiffness parameter) were not significant. The greater stiffness of the carotid arteries is due to their lower content of elastic fibers.
Both types of vessel have a coefficient of thermal expansion dependent on the internal pressure to which they are subjected. This coefficient is negative (the vessels contract as the temperature increases) when the internal pressure is sufficiently low. However, after a threshold, it becomes positive, and reaches a saturation point at pressures higher than those experienced physiologically.
The thermomechanical behavior of arteries should be borne in mind when confronted with clinical situations in which, for example, different types are in contact (ie, at anastamoses), and in which changes in temperature could induce undesirable mechanical stress at the point of union. The intensity of this effect will depend upon the exact tissues/materials in contact; experimental data are therefore needed to characterize the behavior of those of clinical interest.
This work was funded by the Spanish Ministry of Science and Technology via project MAT 2005-6320, and by the Madrid Regional Government via the ESTRUMAT-CM program (reference MAT/77).
Correspondence: Dr. J.M. Atienza.
Departamento de Ciencia de Materiales. Escuela Técnica Superior
de Ingenieros de Caminos. Universidad Politécnica de Madrid.
Profesor Aranguren, s/n. 28040 Madrid. España.
E-mail: jmatienza@mater.upm.es
Received May 3, 2006.
Accepted for publication November 2, 2006.