In recent years, public access defibrillation programs have exponentially increased the availability of automatic external defibrillators (AED) in public spaces but there are no data on their performance in our setting. We conducted a descriptive analysis of the performance of AED since the launch of a public defibrillation program in our region.
MethodsA retrospective analysis was conducted of electrocardiographic tracings and the performance of AED in a public defibrillation program from June 2011 to June 2015 in the province of Girona, Spain.
ResultsThere were 231 AED activations. Full information was available on 188 activations, of which 82% corresponded to mobile devices and 18% to permanent devices. Asystole was the most prevalent rhythm (42%), while ventricular fibrillation accounted for 23%. The specificity of the device in identifying a shockable rhythm was 100%, but there were 8 false negatives (sensitivity 83%). There were 47 shockable rhythms, with a spontaneous circulation recovery rate of 49% (23 cases). There were no accidents related to the use of the device.
ConclusionsNearly half of the recorded rhythms were asystole. The AED analyzed showed excellent safety and specificity, with moderate sensitivity. Half the patients with a shockable rhythm were successfully treated by the AED.
Keywords
Out-of-hospital cardiac arrests (OHCAs) are a public health issue, both due to their frequency (an estimated annual incidence in Spain of 24 000-50 000 cases)1 and their high rates of mortality and sequelae.2,3
When the OHCA is caused by ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT), prompt electrical defibrillation is the only effective treatment, and its timeliness is the most important factor in patient survival.4–6 Automatic external defibrillators (AEDs) can identify and treat ventricular arrhythmias and are safe and effective even in the hands of untrained laypersons.7–9 Accordingly, public access defibrillation programs have deployed AEDs to strategic locations for use by the general public in the event of a cardiac arrest.8,10–13
AEDs use manufacturer-programmed and -verified algorithms to classify the cardiac rhythm and apply a therapy, if possible; nonetheless, these algorithms can make errors in the presence of artifacts related to cardiopulmonary resuscitation (CPR), due to poor positioning of the self-adhesive lead sensor, or when the programming cannot identify the cardiac rhythm.14,15 There is little information on the functioning of these devices in real-world conditions but some analyses have detected significant errors in rhythm detection or treatment.16,17
In addition, shockable rhythms as a proportion of all OHCAs vary according to the series and might be decreasing for various reasons, such as improved treatment of coronary heart disease and more widespread use of implantable defibrillators.18,19
The purpose of this study was to perform a descriptive analysis of rhythms recorded in OHCA and of the functioning of AEDs since their deployment in a public access defibrillation program.
METHODSPatientsWe prospectively recorded all AED activations in the Girona Territori Cardioprotegit program from June 2011 to June 2015.
This project is a public access defibrillation initiative promoted by the Girona City Council (Dipsalut) and began in 2011. The program was enabled by a change in regional law allowing AEDs to be used by any person in the event of an emergency. Although no CPR training was given to the general public, an awareness campaign was launched involving public events attended by more than 10 000 people, as well as specific school courses that reached more than 4000 students.
A total of 747 AEDs were distributed according to population density (1 per 1000 population) in either public places (577 permanent AEDs) or as part of the equipment of police, fire department, and basic life support ambulance crews (170 mobile AEDs). These professionals received an official course on AED use.20 The location of the permanent devices can be consulted on the website of the Girona Territori Cardioprotegit project.21
The AEDs distributed by the program are the PowerHeart AED G3 9300 manufactured by Cardiac Science (Bothell, Washington, United States), authorized for use in Europe by the Medical Device Safety Service. This model delivers a charge that is adapted to the patient's impedance and increases in successive defibrillations, beginning with 126 to 260J and continuing with charges between 170 and 351J.
Electrocardiographic tracings were obtained from the AEDs; we excluded those that were not actually OHCAs or had incomplete or unintelligible information.
Information Obtained From the Automatic External DefibrillatorsThe records extracted from the AEDs were saved in PDF and contain information on the time of device opening, the time of cardiac rhythm detection and interpretation, and the number of shocks administered, as well as the electrocardiographic tracings. Also recorded from each device activation were the type of AED used (mobile or permanent) and information on patients’ vital status after CPR maneuvers. A retrospective descriptive analysis was performed of the data collected.
The initial rhythm recorded by the AED for each patient was used for the descriptive analysis of the arrhythmias underlying the cardiac arrest and the study of the diagnostic accuracy of the algorithms. All recorded arrhythmias were used in the analysis of the therapeutic effectiveness of the device.
DefinitionsThe cardiac rhythms of the electrocardiographic tracings obtained by the activated and used AEDs were classified according to the consensus document of the American Heart Association.14 Accordingly, VT, coarse VF (> 200μV), and fine VF (≤ 200μV) were considered shockable rhythms; sinus rhythm, atrioventricular block, atrial fibrillation, and other supraventricular rhythms were considered nonshockable. An AED shock was considered effective if it managed to reverse the shockable rhythm, regardless of the final rhythm.
The type of AED activation was classified into 3 categories: a) correct, involving a patient with sudden loss of consciousness who failed to respond to commands and who was administered basic CPR maneuvers; b) intermediate, involving a patient with loss of consciousness who quickly recovered and did not thus require CPR or a patient who did not lose consciousness but whose situation was considered serious by possible resuscitators; and c) incorrect, involving antisocial behavior.
CPR performance was indirectly evaluated via the chest compression waves visible on the electrocardiographic tracing. Similar to previous work,22 resuscitation maneuvers were considered to have been performed if this type of wave was visible and were considered adequate if they met the following characteristics: a) the AED instructions were followed; and b) the CPR was consistently performed and at a frequency of > 50 compressions/min.
Statistical AnalysisTo study the sensitivity and specificity of the arrhythmia detection algorithms of the AED, the reference standard was an independent reading of the electrocardiographic tracings by 4 cardiologists. Any disagreements were resolved via joint analysis of the tracing until a consensus was reached. Continuous variables are presented as mean±standard deviation and categorical variables as absolute values and percentages. Categorical variables were compared using the chi-square test and continuous variables using the Student t test. A 2-sided P < .05 was considered statistically significant.
RESULTSActivations of the Public Automatic External DefibrillatorsFrom the initiation of the Girona Territori Cardioprotegit project in June 2011 to June 2015, there were 231 AED activations. The activation involved a mobile AED in 176 cases (76%) and a permanent device in 55 (24%).
Of these 231 activations, 210 (91%) were considered correct uses, 14 (6%) were intermediate, and 7 (3%) were incorrect. No electrocardiographic tracings were obtained from the 21 cases classified as an intermediate or incorrect use. Of the 210 cases classified as a correct use, 20 lacked an electrocardiographic recording and 2 had an unintelligible tracing. Thus, 188 activations could be analyzed (81.4% of the total); 154 were from mobile AEDs (82%) and 34 from permanent AEDs (18%).
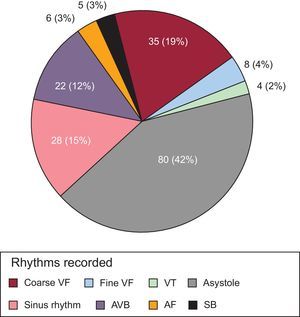
Analysis of the Recorded ArrhythmiasThe rhythms underlying the OHCAs are shown in Figure 1. The rhythm most frequently recorded by the AEDs was asystole, in 80 patients (42.5%). VF was present in 43 patients (22.8%), comprising 35 coarse VFs (18.6%) and 8 fine VFs (4.2%).
Distribution of recorded cardiac rhythms. Values are numbers and percentages of the total. AF, atrial fibrillation; AVB, atrioventricular block; Coarse VF, coarse (> 200mV) ventricular fibrillation; Fine VF, fine (≤ 200mV) ventricular fibrillation; SB, sinus bradycardia; VT, ventricular tachycardia.
The remaining tracings in order of frequency were sinus rhythm (28 patients, 14.9%), second- and third-degree atrioventricular block (22; 11.7%), atrial fibrillation (6; 3.2%), sinus bradycardia (5; 2.6%), and VT (4; 2.1%). Shockable rhythms comprised 25% of all tracings.
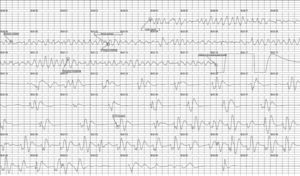
Evaluation of Automatic External Defibrillator FunctioningOf all of the activations analyzed, the AED determined that 39 tracings contained an initial shockable rhythm (20.7%). There were no false positives. A tracing of a successfully treated shockable rhythm is shown in Figure 2.
Example of a successfully treated shockable rhythm. After lead placement, a coarse ventricular fibrillation was detected, which was followed by an effective shock that reversed the abnormal ventricular rhythm. The tracing shows the diagnostic, charging, and shock phases of the device. CPR, cardiopulmonary resuscitation.
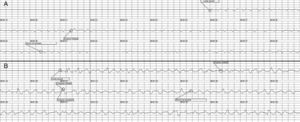
AEDs determined 149 of the tracings (79.2%) to be nonshockable. Eight false negatives were identified (4 fine VFs and 4 coarse VFs) (Figure 3).
Based on these data, the sensitivity of the AED algorithms for detecting shockable rhythms was calculated at 82.9%, with a specificity of 100%. Their sensitivity for the detection of the different types of shockable arrhythmias was 89% for coarse VF, 33% for fine VF, and 100% for VT.
The time required by the AED to identify the rhythm was 7.0±2.0seconds; it was much shorter for shockable rhythms than nonshockable rhythms (4.0±1.0seconds vs 8.0±1.8seconds; P < .001).
In the 39 cases determined by the AED to have an initial shockable rhythm, a therapy was indicated. A total of 98 shocks were administered, with a mean of 2.4 shocks (1-11) per patient. In 85.4% of the administered shocks, the device managed to reverse the arrhythmia.
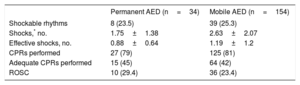
Comparison Between Mobile and Permanent Automatic External DefibrillatorsComparisons between time of device use, percentage of shockable rhythms, number of shocks, number of effective shocks, performance of CPR, and rate of return of spontaneous circulation between permanent and mobile devices are summarized in Table. There were no significant differences between the 2 systems for any of the above variables, except for the number of shocks, which was significantly higher with mobile devices (2.63 vs 1.75; P=.019). Permanent devices had a nonsignificantly higher rate of return of spontaneous circulation (29.4% vs 23.4%; P=.459).
Comparative Analyses of Time, Cardiac Rhythm, and Effectiveness Between Permanent and Mobile Automatic External Defibrillators
| Permanent AED (n=34) | Mobile AED (n=154) | |
|---|---|---|
| Shockable rhythms | 8 (23.5) | 39 (25.3) |
| Shocks,* no. | 1.75±1.38 | 2.63±2.07 |
| Effective shocks, no. | 0.88±0.64 | 1.19±1.2 |
| CPRs performed | 27 (79) | 125 (81) |
| Adequate CPRs performed | 15 (45) | 64 (42) |
| ROSC | 10 (29.4) | 36 (23.4) |
AED, automatic external defibrillator; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
Based on analysis of the waves produced in the tracings by the CPR maneuvers (Figure 4), chest compressions were performed in 152 patients (80.1%), but only 79 (51.9%) were considered adequate according to CPR quality criteria. There were no differences in maneuver performance (79% vs 81%; P=.8) or quality (45% vs 42%; P=.7) between fixed and permanent devices.
Chest compression waves visible in the tracings. The arrows indicate the waves recorded in the tracings that are due to the performance of CPR maneuvers. Two cycles of 30 compressions and 1 pause can be seen, presumably because the standard 30:2 compression-to-ventilation ratio was being followed. CPR, cardiopulmonary resuscitation.
Data were available on the return of spontaneous circulation for 176 of the 188 analyzed patients (94%); 46 (26.1%) survived to resuscitation. In the case of the 47 shockable rhythms, the rate of return of spontaneous circulation was 49% (23 patients), whereas the rate was 18% for the 129 nonshockable rhythms (P < .001). There were no accidents related to device use.
DISCUSSIONThis study represents the first descriptive study of automatic defibrillator functioning in the context of a public access defibrillation program implemented in Spain. Three aspects stand out from the results: the low proportion of shockable rhythms, the suboptimal sensitivity of the detection algorithms of the devices, and room for improvement in the performance of CPR maneuvers.
In our study, analysis of the electrocardiographic tracings of the AEDs revealed that the most frequent rhythm was asystole (in 42.0% of patients), whereas VF was seen in just 22.7% of patients; 24.8% of the rhythms were shockable. These data agree with the progressive decrease in the proportion of VF found in different registries derived from out-of-hospital emergency care systems.18 Thus, for example, in the multicenter CARES registry of 40 274 patients, the proportions of asystole and VF were 45% and 18%, respectively.23
However, the proportion of shockable rhythms in our series contrasts with that of a recent Danish registry based on tracings obtained from AEDs, which found a shockable rhythm proportion of 55%.24 These differences could be explained by the logistical characteristics of the Girona Territori Cardioprotegit project.
Our program shows a considerable geographical dispersion, with an approximate population density of 128 inhabitants/km2 and 1 AED per 1000 population, in contrast to the 663 inhabitants/km2 and 1 AED per 800 population in the Danish registry. The geographical dispersion has meant that the Girona provincial program is largely based on mobile devices, similar to other successful published experiences,8 unlike the Danish registry, which was based on permanent devices.
Thus, a higher population density near the AEDs could have led to a more rapid use of the devices and the higher proportion of shockable rhythms found in the Danish registry. Unfortunately, due to the design of the 2 registries, there was no information on the time from cardiopulmonary arrest to AED use. Nonetheless, the rate of return of spontaneous circulation of 91% in the Danish study vs 49% in our series supports our hypothesis that there was a longer time from cardiopulmonary arrest to AED use in the Girona Territori Cardioprotegit program, probably due to the geographical conditions. A Taiwanese registry of OHCA that analyzed AED tracings containing information on the time from cardiorespiratory arrest to device application found a long interval (9minutes), a 12.6% proportion of shockable rhythms, and a rate of return of spontaneous circulation of 20%.25 The time from collapse to first shock of 2.4±3.6minutes reported in a recent Japanese registry26 that only included shockable rhythms led to a rate of return of spontaneous circulation of 49.6%, similar to that found in our work.
Second, in our series, the device detection algorithms were highly specific for shockable rhythms and were safe, given that no inappropriate shocks were recorded. However, their sensitivity was moderate overall (83%), higher for coarse VF and VT at 89% and 100%, respectively, but only 33% for fine VF. This sensitivity issue has already been reported. In 2001, Macdonald et al.16 analyzed 3448 AED tracings and found a sensitivity of 91.8% for the detection of coarse VFs and of 67.3% for fine VFs, with 99.9% specificity.
In the case of the AEDs used in the present study, the AED classifies rhythms with a baseline-to-peak value ≤ 0.08 mV as asystole and not requiring therapy.27 The tracing voltage is influenced by various factors, including patients’ body type, the presence of hair or sweat, and pad placement precision. Although the sensitivity of the algorithms of the present study are within the levels recommended by the American Heart Association,14 because there are serious consequences when a shockable rhythm is missed, we believe that the algorithms should be optimized to increase the sensitivity for fine VF or that a shock should possibly be applied when the device identifies asystole.
Finally, although the methodology for evaluating the performance of CPR maneuvers is indirect, recent studies have shown that the use of AEDs in CPR substantially increases the performance of maneuvers by witnesses. While still far from the 99.4% performance of maneuvers in a public access defibrillation group of a Japanese registry,26 the 80.1% obtained in the present work is nonetheless markedly higher than the 29% reported in a recent multicenter registry of arrests, almost all witnessed, treated in Catalan cardiac intensive care units.2 Effort should be concentrated on educating the general public to increase the performance of CPR maneuvers by witnesses because CPR has been proven to improve survival.28
LimitationsThe main limitation of our work is that it is solely based on electrocardiographic recordings and the times recorded by the defibrillator. We thus have no information on any other variables crucial to the study of the role of AEDs in the treatment of OHCA, such as mid- and long-term mortality and the presence of neurological sequelae. We also have no data on the time from collapse to AED application or on OHCAs from the province of Girona that were not treated with a device forming part of the Girona Territori Cardioprotegit program. In addition, the information on CPR maneuvers was indirectly obtained via the chest compression waves recorded in the electrocardiographic tracings and should be interpreted with caution.
CONCLUSIONSAnalysis of the AED tracings of the Girona Territori Cardioprotegit program revealed that almost half of the recorded rhythms were asystole. The AEDs analyzed showed excellent safety and specificity and moderate sensitivity. AEDs successfully treated half of all patients with a shockable rhythm. Effort should be concentrated on improving algorithm detection.
CONFLICTS OF INTERESTNone declared.
- –
The widespread use of automatic or semiautomatic external defibrillators improves OHCA prognosis and increasing numbers of public access defibrillation programs have been implemented.
- –
Nonetheless, evidence shows that the percentage of shockable rhythms is decreasing, possibly undermining the effectiveness of this strategy. In addition, some studies indicate that device interpretation errors could affect prognosis, which is why defibrillator effectiveness should be periodically reviewed.
- –
The Girona Territori Cardioprotegit program is the first public access defibrillation program in Spain. The present study provides the first data from Spain on the use, safety, and effectiveness of AEDs and the type of arrhythmia in the context of OHCAs within a public access defibrillation program.
- –
In addition, this work confirms previous findings on the reduction in shockable rhythms and on the suboptimal sensitivity of AEDs in the detection of fine VFs.