Keywords
INTRODUCTION
Cardiovascular diseases (CVD) are the leading cause of death in Spain,1 with the most important of these being ischemic heart disease (IHD) and cerebrovascular disease (CD).2,3 Although mortality from certain CVD has tended to fall in developed countries, including Spain, where this trend has been confirmed, its prevalence has nevertheless increased over recent years. Reasons for this include the rise in life expectancy of the general population and the improvements in the treatment and management of these diseases.2,4
The origin of CVD is multifactorial, though cardiovascular risk factors (CVRF) are dominant5 and are relatively well studied in Spain.6 The epidemiology of CVD should include both the prevalence, as CVD are chronic diseases, and the incidence, which is particularly important given the improvements in primary prevention, such as control of CVRF,7 in order to confirm whether the incidence is decreasing as well as the mortality.2,4
However, prospective studies on the incidence of CVD in Spain are few. In addition, none of them have fully examined the main CVD, and they have mainly studied the incidence of IHD, as in the Manresa study,8 undertaken in men aged 30-59 years, and the study by Marín et al,9 in persons older than 25 years of age. Nonetheless, a large part of the cardiovascular risk corresponds to other CVD, such as CD or peripheral arterial disease (PAD) of the lower limbs.10 In the case of heart failure, its epidemiology is even less well known and its incidence is increasing11 as a result of the greater life expectancy and improved prognosis of IHD.
The aim of this study was to examine the incidence of IHD, CD, PAD, and heart failure by studying a population-based cohort at 2 health centers in the city of Barcelona, Spain.
METHODS
Study Type and Patient Selection
We undertook a prospective cohort study that was based on a cross-sectional descriptive study of the prevalence of CVRF and CVD,12 which was used as the starting point for the cohort study. The study was carried out in 2 primary care health centers in Barcelona, Spain, covering a heterogeneous population with respect to socioeconomic status, with a high level of attendance and 35 275 clinical histories at the start of the study. The local Ethics Committee (Fundación Jordi Gol i Gurina) approved the study.
The participants were selected by simple random sampling of the population covered, which is the preferred method in the primary care setting.13 The participants, aged 35 to 84 years from the 2 health centers (target population), were all free of any CVD and were willing to take part in the study. Persons were excluded if they had advanced tumors, dementia or any disease involving a life expectancy of less than 1 year.
Data Collection
After first performing a pilot study with 20 different protocols in order to detect possible errors in design and to train the study physicians, the data were collected with a standardized protocol, which remained unchanged throughout the study. The physicians involved were not necessarily those the patients were assigned to. Concordance between the surveyors and a reference pattern (consensual review) was checked by reviewing 120 protocols with a completed follow-up. The study period was between June 1998 and June 2008. The information collected was based on the initial descriptive study,12 biannual review of the clinical history (on paper until 2003 and then computerized as of that year), and review of hospital discharge reports, diagnostic tests (electrocardiograms, exercise stress tests, catheterizations, ankle-brachial index, echo-Doppler, magnetic resonance imaging, computerized tomography, and other imaging tests), blood tests, and regular medication. The physicians responsible for the patients were all contacted, and any participant who had not attended the health center during the previous 12 months was contacted by telephone. For the participants who died during the follow-up, the data were checked against the Catalan Registry of Deaths when the cause of death was not clearly established.
Baseline Variables at the Start of the Follow-up
The following variables were studied: age (years); sex; smoking, coded as smoker, non smoker and ex smoker14; total cholesterol and high density lipoprotein cholesterol (HDL-C) (mg/dL); diagnosis of hypercholesterolemia, coded dichotomously (cut point, 250 mg/dL)15; drug therapy for hypercholesterolemia; systolic and diastolic blood pressures (mmHg); hypertension, classifying the patients as hypertense (including in this category those patients who were taking antihypertensive drugs) or not hypertense15; drug therapy for hypertension; diabetes mellitus, using the American Diabetes Association criteria adopted by the Spanish Society of Family and Community Medicine16 (patients were also included as diabetics if they were being treated with insulin or oral antidiabetic agents); glycated hemoglobin (%); drug therapy for diabetes mellitus; body mass index, calculated by dividing the weight in kilograms (measured with a previously calibrated scale and the patient without shoes) by the square of the height in meters, measured in the same conditions using a stadiometer; and obesity (body mass index ≥30).14
Cardiovascular Diseases During the Follow-up
Only the first episode was considered of any of the following CVD:
1. Acute myocardial infarction, fatal of nonfatal if recorded on the hospital discharge report with markers of necrosis, autopsy report, or ICD-9 codes 410-414, 429.9 and 798 and ICD-10 codes I20-I25, I46.1 and R96 on the death certificate.17
2. Angina, if the history was compatible, with or without electrocardiographic changes during the episode, plus a positive exercise stress test, scintigraphy or coronary arteriogram.
3. Stroke, fatal or nonfatal in the form of a compatible clinical history (focal deficit) with confirmatory computerized tomography or magnetic resonance imaging, an autopsy report or ICD-9 codes 430-434 and 436-438 (excluding 437.4-437.8) and ICD-10 codes I60-I64, I67, I688 and I690-I698 on the death certificate.18
4. Transient ischemic attack if the patient had a reversible focal ischemic episode lasting <24 h, with no permanent neurological deficit afterwards, and with computerized tomography or magnetic resonance imaging that ruled out cerebral infarction,18 and with the neurologist's evaluation on the hospital discharge report.
5. Peripheral arterial disease in any of the following 3 situations9: clinically compatible intermittent claudication (pain in the lower limbs while walking that improved with rest) plus a diagnostic arteriogram or echo-Doppler and an ankle-brachial index <0.9; pain at rest in the lower limbs not attributable to other causes plus a diagnostic arteriogram or echo-Doppler and an ankle-brachial index <0.9; amputation of the lower limbs or any part of the leg or foot, ischemic ulcers or gangrene of any part of the leg or foot or attributable to an ischemic deficit.
6. Heart failure, when the patient had a history of dyspnea, fatigue or ankle swelling, objective evidence of cardiac worsening on an electrocardiogram or compatible chest radiograph,20 and an echocardiogram with ventricular dysfunction or ejection fraction <40%.
Statistical Analysis
The statistical analysis was done with SPSS, EPIDAT and CIA. The concordance between the surveyors and the reference pattern was studied with the kappa statistic and the intraclass correlation coefficient (values >0.8 were considered to represent good concordance). The means were compared with the Student-Fisher t test and the proportions with the χ2 test, using the corresponding tests if their conditions for application were not fulfilled. The difference by sex in the incidence of the CVD was studied by the log-rank test. As measures of incidence, calculations were made of the crude incidence rates for each 100 000 persons per year of observation (stratified by age and sex) and the standardized rates, by the direct method, using the European population21 and the world population as a reference,22 with the age strata of 35-49, 50-64, and 65-84 years. Likewise, the baseline cardiovascular risk was calculated for the patients aged 35-74 years using the Framingham-Wilson equations23 and calibrated with the REGICOR (Registre GIroní del COR).24 The level of significance was α<.05 in all cases.
RESULTS
Of the 2248 persons in the initial descriptive study, 702 were excluded as they were outside the age range and 132 as they already had CVD. Of the remaining 1414, 349 lacked complete baseline data on CVRF, 58 refused to participate in the study follow-up, and 76 were lost to follow-up (with no significant differences in age or sex as compared to those who completed the follow-up). Thus, 931 persons completed the study. The concordance study produced values >0.8 for the kappa statistic and the intraclass correlation coefficient in all the study variables.
Table 1 shows the characteristics of the study population. Significant differences were found according to sex: in the men there were higher proportions of smokers, ex smokers and diabetics. The women had a greater prevalence of hypercholesterolemia, hypertension, drug-treated hypertension and obesity. Quantitatively, the women had higher total cholesterol and HDL-C values. Differences were also seen in the categories of total cholesterol, HDL-C and hypertension (Table 1).
During the follow-up, 126 persons had a CVD, with a cumulative incidence of 13.5% (95% confidence interval [CI], 11.3-15.7). The most common CVD was IHD, with a cumulative incidence of 6.1% (95% CI, 4.7-7.9), followed by CD (4.3%; 95% CI, 3.4-6.2), heart failure (3%; 95% CI, 2-4.3) and PAD (1.9%; 95% CI, 1.2-3).
The baseline cardiovascular risk for IHD at 10 years was 14.4% using the Framingham-Wilson equation and 6.2% according to the REGICOR. Considering the true proportion of IHD (6.1%), the Framingham-Wilson equation significantly overestimated this risk (P<.001), whereas the REGICOR calculation showed no significant difference (P>.05).
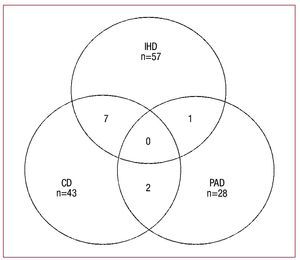
The figure shows the overlapping of the CVD studied, with notable overlapping of CVD caused by IHD and CD.
Figure 1. Overlapping of ischemic heart disease (IHD), cerebrovascular disease (CD), and peripheral arterial disease of the lower limbs (PAD).
Tables 2 to 5 detail the crude and adjusted incidence rates for each 100,000 inhabitants per year in the CVD studied, stratified by age, sex and total participants.
For IHD (Table 2), the total cumulative incidence of all cases was slightly higher in acute myocardial infarction as compared with angina, increasing with age, particularly in the case of angina. Those older than 65 years of age accounted for 54.4% of all cases of IHD (cumulative incidence, 9.6%), though a greater proportion of these concerned angina (68%). By sex, there was a higher incidence of acute myocardial infarction in men (5 times greater; log-rank test, P<.0001), but no difference according to sex for angina (log-rank test, P=.6494).
For CD (Table 3), the cumulative incidence was greater for stroke than for transient ischemic attack. Stroke tended to increase with age, both in men and in women, but this was not so obvious for transient ischemic attack. CD mainly affected patients aged ≥65 years, who accounted for 67.4% of all cases (cumulative incidence, 8.9%), particularly at the expense of stroke (74.2%). The women had a higher incidence of stroke, though the difference was not significant (log-rank test, P=.2015); results for transient ischemic attack were similar for men and women (log-rank test, P=.9121).
For PAD (Table 4), the cumulative incidence rose with age, reaching 55.6% in those aged ≥65 years (cumulative incidence, 3.1%), though this trend was not so marked for women. No differences in the incidence of PAD were found according to sex (log-rank test, P=.9309).
Finally, for heart failure (Table 5), the pattern was similar to that of PAD: an increase in the incidence with age (53.6% of cases in patients aged ≥65 years, with a cumulative incidence of 4.6%), a lower tendency for this increase in women, and similar incidence in both sexes (log-rank test, P=.9597).
DISCUSSION
The results of this study show that the incidence of CVD goes beyond just IHD. The incidence of CD, though lower than that of IHD, still accounts for an important proportion of all CVD. Of particular note was the incidence of heart failure, the third leading cause of CVD, the impact of which may well increase over the coming decades. The greatest incidence was found in those aged over 65 years, particularly in the case of CD. By sex, significant differences were only seen for acute myocardial infarction. In general, the incidence of the CVD studied was confirmed to be lower as compared with other developed countries.
Comparison With Other Studies
Ischemic heart disease continues to predominate in men, though mainly as a result of acute myocardial infarction, since the incidence of angina was similar in both men and women. In the study by Tomàs i Abadal et al,8 in men aged 30-59 years the crude incidence rate of acute myocardial infarction for each 100 000 inhabitants per year was 499; in the same age range for our study the corresponding figure would be 457 per 100 000 inhabitants per year, similar to that of Tomàs i Abadal and lower than that in other countries.25 The study by Marín et al,9 which did not review death certificates, showed crude incidence rates for each 100,000 inhabitants per year (population aged, 35-84 years) of 402 in men and 125 in women for acute myocardial infarction; and 402 in men and 345 in women for angina, again lower than those in other countries.23 In our study the incidence of acute myocardial infarction was slightly higher in men and similar in women, whilst for angina the figures were higher in both sexes in the study by Marín et al.9 The REGICOR group studied the trends for acute myocardial infarction in the province of Girona,26 and found crude rates for each 100 000 inhabitants per year, adjusted for the world population aged 35-64 years, of 200 in men and 31 in women, exceptionally low incidences, particularly in women.
Concerning the incidence of CD in Spain, the study by Caicoya et al27 examined the incidence of CD in patients with no history of transient ischemic attacks, and found lower incidence rates than we did (132 and 61 cases per 100 000 inhabitants per year in men and women, respectively). López-Pousa et al28 studied a rural population from Girona and found a crude rate per 100,000 inhabitants per year of 174 for stroke and 64 for transient ischemic attack. The study by Alzamora et al29 found adjusted incidence rates (European population) for ischemic stroke in men and women of 165 and 115 per 100 000 inhabitants per year, respectively, somewhat lower than the rates seen in our study and with a greater incidence in men. A recent multicenter study30 high lights the variability between different European countries, with adjusted rates (European population) in Menorca of 116 and 66 cases per 100,000 inhabitants per year in men and women, respectively. However, in these studies26-30 no review was made of death certificates, which could explain why our figures were slightly higher.
With regard to the incidence of PAD, we are unaware of any other studies in Spain, though a few population-based prevalence studies have been carried out.31-33 The incidence was rather higher in women, though the low number of cases of PAD in each sex necessitates caution when interpreting these results. Nevertheless, it was notable that cases of silent PAD, as diagnosed by an ankle-brachial index <0.9, were much more common than the symptomatic forms of the disease.32-33 The incidence of symptomatic forms of PAD appears to be lower than the incidence of IHD and CD, coinciding with the prevalence figures.12
A few studies are available about the prevalence of heart failure,34,35 but with no data on incidence. The most recent study34 indicated a prevalence of 6%-8% in persons aged over 45 years, thus placing heart failure as the third leading CVD. The increase in life expectancy, the greater survival of patients with IHD and the growing prevalence of hypertension, obesity and diabetes mellitus will all lead to heart failure becoming a public health problem of the first order,36 as these latter conditions are a very frequent reason for hospital admission in persons older than 65 years of age.37
The importance of CVD has occurred mainly due to IHD and CD. The relative importance due to heart failure has not been studied because it is often caused by IHD itself. Given that IHD and CD are the most frequent CVD and have the greatest relative importance, it seems reasonable to base the approach to cardiovascular risk on these CVD, which, in addition, also share CVRF. Future cardiovascular risk equations should be developed bearing in mind these CVD.38
Characteristics and Limitations of the Study
This study was carried out at 2 teaching health centers, well established over more than 10 years. The majority of the population will very probably have been seen at some point during this time, and their corresponding clinical history collected. In fact, according to the population census over 80% of users visit the health center to which they are assigned at least once during the course of a year.39 Nevertheless, selection bias may have occurred, even though the large population covered and the random selection tended to minimize this bias. However, the results cannot be directly extrapolated to the general Spanish population, as the geographical area covered was limited. As is common, the participation of women was greater, 7,9,32-34 due to the higher proportion of women in the age range of 35-84 years, and possibly too because of their increased availability or motivation to participate. For this reason the incidence rates were calculated by sex.
To avoid information bias, a pilot test was carried out in which the surveyors were trained and the concordance of the data was verified, with excellent results. Additionally, strict criteria were used concerning the cut points for the quantitative variables and the definition of the variables, and losses of information were minimized by means of contact with the physician and patients. The incidence of CVD may be underestimated, particularly that of transient ischemic attack and, to a lesser extent, angina, PAD and heart failure, owing to the fact that the patients may not report to their health center and also to the diagnostic difficulty involved. Nor were any socioeconomic indicators available, though they may have an important role in the epidemiology of CVD. The gathering of information was satisfactory, although one limitation concerns the lack of personal interviews during the follow-up. Losses to follow-up were few, given patient-proximity and the wide coverage of the health centers. The low incidence found in some of the CVD studied led to wide confidence intervals in the rates, although the precision of the estimation was good (<2%) in the case of the cumulative incidences.
CONCLUSIONS
The results of this study show that CVD represent a public health problem with an important incidence. The cardiovascular risk was confirmed to extend beyond just IHD and consideration should be given to other CVD, such as CD and PAD, as well as to heart failure, the incidence of which is not only worrying but will increase given greater life expectancy and improved survival after an infarction.2
Cardiovascular diseases mainly affect older persons, which makes it more difficult to calculate the cardiovascular risk, as the relevant equations38 only extend up to the age of 74 years (Framingham and calibrated REGICOR equations) or up to 65 years (SCORE). This latter is even more worrying, given that most cases of IHD, and particularly of CD (whose associated mortality is included in SCORE) occurred in persons aged over 65 years. In fact, our study confirms the validity of the calibrated REGICOR equation in IHD, as the figure predicted by the equation (6.2% of cases of IHD at 10 years) did not differ significantly from what was actually found (6.1%).
An integrated strategy for the prevention of CVD is required. This necessitates first dealing with the prevention, control and treatment of CVRF to reduce the incidence of CVD. Secondly, the correct assessment of the cardiovascular risk of the patients should be made by using the equations that have been validated in our setting.38 And thirdly, suitable, early, intensive treatment of the CVD should be given as soon as they appear.38
ACKNOWLEDGMENTS
To all the medical residents of the Family and Community Medicine service who collaborated in this study.
ABBREVIATIONS
CD: cerebrovascular disease
CVD: cardiovascular diseases
CVRF: cardiovascular risk factors
IHD: ischemic heart disease
PAD: peripheral arterial disease in the lower limbs
Correspondence: Dr. J.M. Baena Díez.
Institut Municipal d'Investigació Mèdica (IMIM). Dr. Aiguader, 88. 08003 Barcelona. Spain
E-mail: jbaena@imim.es
Received December 24, 2009.
Accepted for publication May 6, 2010.