Although mortality from coronary heart disease (CHD) has constantly declined, this disease group remains among the highest in incidence, prevalence and mortality rate across Europe and throughout the world. According to the American Heart Association (AHA), the risk factors that significantly increase the likelihood of coronary heart disease, cardiovascular disease and adverse coronary outcomes, identified by years of medical research, include increasing age, male sex, strong family history, smoking, high blood cholesterol, high blood pressure, physical inactivity, obesity and diabetes mellitus.1 Advances in health care also contribute to reducing the risk of coronary mortality, both by primary prevention to reduce these risk factors and by secondary prevention of adverse coronary events among persons with established coronary heart disease. Some researchers have estimated that at present approximately half of coronary mortality among those younger than 75 years could be prevented through these health care interventions.2,3
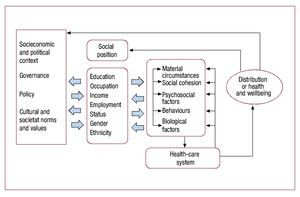
One of the most widely studied contributing factors associated with an increased risk of cardiovascular disease and not included in the AHA list is low socioeconomic status, indicated by income, occupational status, education, or other resources. This factor has also repeatedly been shown to associate with other established medical risk factors that contribute to further increase cardiovascular risk. One of the most widely studied contributing factors associated with an increased risk of cardiovascular disease and not included in the AHA list is low socioeconomic status, indicated by income, occupational status, education, or other resources that contribute to further increase cardiovascular risk. More generally, unfavourable financial situation, poor education, low occupational status and poor labour market situation have been shown to be a health risk in all Western societies. The association between the social position of an individual and his or her health is very complex and multilayered (Figure).4,5 Socioeconomic status reflects the broader socioeconomic and political context of the society, i.e., the structural, cultural, and functional aspects of the social system which impact the patterns of social stratification in the society. These include macroeconomic, social, health and other relevant policies, governance, and cultural and societal values. The individual's socioeconomic position, in turn, affects material circumstances such as housing, consumption potential and physical environment, as well as social and psychological circumstances such as psychosocial stressors, stressful living situations, and level of social support. Behavioural and biological factors include smoking, diet and other behaviours that have an effect on the health of the individual. The role of the health care system in socioeconomic health differences is especially connected to issues of access to and quality of care.
Figure. A theoretical framework for analysing the contribution of social determinants to health. Modified from Solar et al.5
The socioeconomic position of the individual is multidimensional, and the dimensions most relevant to health differences are considered to be education, occupational social class and income. Although measures of the same concept are interwoven, the different dimensions of socioeconomic position highlight specific aspects of it.6 Educational level is strongly determined by parental socioeconomic position, which in turn contributes to a person's social class, income, and knowledge, all of which is interwoven with other non-material resources that are likely to have an impact on health. Occupational social class reflects material working conditions, work environment, and is linked to status and power in the society; individual or family income captures material resources and purchasing power. Both also have a connection to labour market position, especially employment status, which is partly dependent on social class and affects income level. Furthermore, socioeconomic conditions in childhood have an impact on subsequent life-chances, education and occupation. The dimensions of socioeconomic status can mainly be organised chronologically and their significance to individual health can vary in time, across the life-course and between countries. Gender and ethnicity are also important social determinants of an individual's health.
Various explanations for the graded relationship between socioeconomic status and cardiovascular disease incidence, with higher risk corresponding to lower socioeconomic status, have been suggested and constantly debated for decades.7-10 Two main hypotheses or explanations have been presented for the socioeconomic status-health gradient. According to the social causation hypothesis, socioeconomic health differences are explained through the experience of adversity and stressors in low social status groups in comparison to more favourable experiences in higher social groups.11 These experiences can be related to material or psychosocial factors or both. According to the health selection hypothesis, an individual's health status is one of the factors influencing the chance of upward or downward social mobility. Individuals in good health are more likely to move up in the social hierarchy and those in poor health to move down.12,13
Based on the current evidence, several processes of both causation and selection are likely to be at work and their relative importance may vary between developmental stages and from one country and condition or health indicator to another. Some of the mechanisms operate more distantly and others more closely to health outcomes; they may vary across the life-course and may accumulate. It is also likely that the mechanisms, their timing and effects vary across different diseases. The findings of Griselda González-Zobl et al,14 published in the current issue of Revista Española de Cardiología, concerning the association between socioeconomic status and first acute myocardial infarction add to this literature and offer support for the causation hypothesis. The article is based on a case control study examining persons admitted to a Girona hospital due to acute myocardial infarction and comparing them to population controls matched by gender, age and year of recruitment. It examines the association of 2 aspects of socioeconomic status, occupational social class and level of education, to acute myocardial infarction risk and analyses whether this risk is independent of cardiovascular risk factors, including smoking, body mass index, hypertension, diabetes and dyslipidaemia. As is the case in earlier research on the subject, the results presented by González-Zobl et al show that use of several indicators of social position gives a more nuanced picture of the differences between members of different socioeconomic groups. Additionally, the study results highlight the need for more nuanced further studies concerning the association of socioeconomic status and risk of adverse coronary outcomes.
The evidence to date on different mechanisms mediating the complex association between socioeconomic status and cardiovascular disease is not conclusive. If classical behavioural risk factors do not exhaust the association, what are the other mechanisms involved in the process? Are further theoretical and methodological steps needed? If so, what would be the evident next steps? In order to better understand this graded relationship, we propose a non-exclusive and non-exhaustive list of ways for further studies to increase the evidence base:
1. Develop studies with life-course perspective. In order for us to better understand the links between exposures and coronary outcomes we need to recognise the importance of time and timing both in terms of individual life course and across generations. Two different strands of this approach have been identified, one of which concentrates on critical periods for exposures to have longstanding consequences while the other suggests that risks may accumulate over time.5
2. Develop conceptual frameworks and indicators for alternative explanatory mechanisms. The alternative mechanisms are also likely to vary across the life-course of the individual and across different disease outcomes. One candidate for mediating mechanisms in coronary heart disease is psychosocial factors such as working conditions, social relations, social support and experienced stress. Many of these are self-reported, and therefore more sophisticated indicators, repeated measurements of psychosocial stressors and ways of analysing long-term exposure need to be developed in future research.
3. Develop new study designs and methods. Testing the theoretical models of potential mechanisms is highly dependent on the quality of study design and the data that results. New epidemiological methods have been developed to overcome or evaluate some of these problems. One serious problem with the existing longitudinal studies is non-random attrition caused, for instance, by health selection. Longitudinal prospective data—with baseline from early years, repeated measures of exposure and outcome, using multi-methods and independent measures and wide variety of measures—are needed to overcome the most obvious shortcomings. Instrumental analyses, propensity score methods, use of longitudinal register data, pooling large existing data sets, combining self-reported and physiological measures and advanced attrition analyses are available and should be used on a larger scale in future studies.
4. Develop measures of socioeconomic status. More fine-graded measures of different aspects of socioeconomic positioning during the life-course are needed and multiple measures should be used simultaneously in future studies. Attention also must focus on changes in the distribution of socioeconomic groups and the possible changes in their cultural meaning.
In sum, earlier studies concerning the association between socioeconomic status and cardiovascular disease have increased our understanding of the true complexity of this association. Nevertheless, further research is needed to determine what are the mechanisms through which this association could work and what would form the basis for the most effective policy interventions and actions.
SEE EDITORIAL ON PAGES. 1045-53
Full English text available from: www.revespcardiol.org
Correspondence: Dr. K. Manderbacka,
Service System Research Unit. National Institute for Health and Welfare, P.O.Box 30. FIN-00271 Helsinki. Finland
E-mail: kristiina.manderbacka@thl.fi