We are fortunate to have the RECALCAR registry, which is an essential tool for understanding and improving the state of cardiology care in Spain. In addition to providing a representative sample of a large number of cardiology units—a sample that has remained exceptionally stable for a decade—the registry is combined with the minimum data set (MDS) of the clinical and administrative databases of the Spanish National Health System. The astute comments and timely discussion of cardiovascular care in Spain made by Cequier et al.1 in an article recently published in Revista Española de Cardiología are excellent in all respects.
We would like to add several comments on the data to help define the future direction of cardiovascular care in Spain and share a few thoughts. Increasing the number of cardiologists—a desirable goal per se—requires a reconsideration of their health care responsibilities. This is because the scope of cardiovascular care far exceeds cardiologists’ current capacity and includes a vast range of tasks, such as health promotion and prevention strategies, heart failure care, etc. The analysis by Cequier et al.1 does not discuss the collaboration or integration of cardiology care with other healthcare providers, which is essential. For example, not all highly prevalent diseases, such as hypertension and chronic coronary disease, need to be regularly followed-up by cardiology departments in the public system. However, treatment of these large cohorts elsewhere has a huge impact on health indicators for the population as a whole. Although obvious, it is crucial to remember that RECALCAR represents only some of the cardiovascular care actually provided in Spain.
The increase in the number of on-duty cardiology shifts, however small, is certainly a welcome change. Any incremental benefit provided by cardiologists to the care of patients with cardiovascular disease is maximized if applied to the entire care process, including hospital-based round-the-clock care. It is in specific circumstances, such as acute conditions and critical situations, that cardiologists play a key role in patient prognosis.2
The presence of cardiologists 24 hours a day, 7 days a week, plus the effects of care networks (most clearly seen in the use of the infarction code), help reduce inpatient mortality due to myocardial infarction and should be stressed.3
Furthermore, organizing round-the-clock cardiology care as a one-stop service greatly enhances the efficiency of the system compared with traditional models that refer all patients not showing imminent risk—the majority—for outpatient assessment. In our experience, this approach not only confers a clinical benefit and immediately reassures the patient, but also shortens the time taken in providing health care, classifying the patient's health problem, and referring the patient to the most appropriate service, thus avoiding redundant efforts and freeing up resources.
In the case of diagnostic imaging studies, the number of scans performed seems to be an increasingly poor indicator for evaluating echocardiography activity and has risen only slightly. Because of the value of echocardiography in every cardiology consultation and the availability of portable equipment, its use is no longer confined to traditional cardiology clinics. Consequently, its impact is hard to measure, particularly in view of the growing use of intracardiac echocardiography by other medical specialists not included in the registry. In tandem, the greater complexity of certain imaging tests (eg, support for procedures or specialized units) has only a slight impact on the numbers, despite very high levels of resource use, and requires the expertise of imaging cardiologists, who should be freed from performing straightforward studies that could be assigned to other specialists. Therefore, more precise information would be helpful when including this activity in the registry.
Thus, in the current health care panorama, RECALCAR should include data from areas it currently underrepresents, such as care provided outside the publicly-funded health care system in Spain, and activities coordinated, shared, or assigned to other specialties, the role of advanced nursing practice, and the rising levels of care provided by day hospital units that minimize the need for conventional hospitalizations.
The relatively low incidence and prevalence of coronary disease in Spain, compared with those in similar European countries, and the decrease in cardiovascular mortality should serve as an incentive to strive even harder.3,4 The favorable results could lead to complacency and encourage health authorities to view the treatment of these diseases as merely routine, which should be avoided.
The publication and dissemination of specific indices by autonomous communities, health areas, and even specific facilities could serve as a stimulus, as well as help to enhance health care equity.
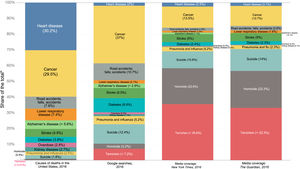
An important issue is how to interpret the activity increases reported in the article by Cecquer.1 The growth seems so slight as to be almost at a complete standstill. Interventions able to capture the attention of the public and its representatives are probably crucial5 because, without competing with the undeniable relevance of oncology and neurosciences, attention should not shift from cardiovascular disease, which would lead public interest to dwindle (figure 1).6
The 4 columns represent the most common causes of death in the United States in 2016, Google searches on this topic, and media coverage in the New York Times and The Guardian, respectively. Heart disease (in the upper band of each column) accounts for very different percentages. Figure taken from Ritchie et al.6.
Enhancing awareness of the therapeutic importance of present-day cardiology requires greater acknowledgement of all types of cardiovascular procedures (coronary, structural-valvular, and arrhythmic) that goes beyond areas of clinical excellence currently being implemented. At present, it is hard to explain to well-informed citizens that while there is a commitment not to exceed surgical waiting list targets, the same is not true for other procedures, some of which are designed to resolve the same conditions as surgery, and whose waiting lists will undoubtedly increase. Indeed, any productivity indicators should be analyzed in relation to the demand for these procedures and adjusted to meet strict criteria limiting any distorted or biased interpretations.
The scope of cardiovascular care has expanded beyond its main historical focus to include new areas.
Remote care (eg, e-visits, phone consultations, remote follow-up and monitoring) currently has proven benefits for management and clinical outcomes.7–9 However, a precise, standardized definition of the various subcategories of remote care is needed for this type of registry.
Outpatient clinics are a crucial part of the system, as they are one of the access points for specialized care and play a key role in the transition from an inpatient-based to an outpatient-based system to promote system sustainability and patient convenience.
These visits should be considered in detail, distinguishing among entities, and integrated with programs or units attending specific health problems. A welcome example is provided by heart failure units. However, progress is needed to avoid grouping distinct entities in an excessively broad category and to create focused clinical pathways requiring specific approaches. A good example is valve disease, which is increasingly acknowledged.10
Unlike the treatment of highly prevalent diseases such as coronary disease and heart failure, some procedures help only a few patients but involve heavy resource use. A quintessential example is cardiogenic shock, which requires a combination of health care networks for early identification and resource allocation plus well-endowed dedicated centers with a high level of expertise.10,11
One of the missions of RECALCAR is to convey to the cardiology community the importance of using data as the basis for analysis before decision-making. This applies to the field as a whole and to hospitals, allowing individual results to be compared with averages.
The lack of interconnectedness between electronic medical record systems in Spain, as well as the multiple and distinct collections of “standard terminology” included in each interface for recording the information, is disconcerting to health care staff, who justifiably crave the structured information that can be provided by these systems. The information could be adapted for direct extraction, allowing it to be entered into RECALCAR. The AVACAR12 dictionary is an indispensable step in the right direction to standardize reports and, thereby, health care activity records, thus increasing accuracy and facilitating comparison as an essential tool for improvement, apart from any additional uses.
Other areas that might warrant inclusion in the registry are structured, controlled, and homogenous data from the patient's perspective and information that would allow cost-effectiveness comparisons. As the information recorded in RECALCAR becomes more significant over time, internal and external data audit systems should be considered, given the inherent limitations of this model of information collection.
This approach leads us to something that the society rightfully demands: reporting results to the general population should be a goal of health care providers at all levels.
Consequently, we believe it would be advisable to adapt the activity registry with a view to linking activities to health outcomes. The framework proposed by Porter13 is eminently applicable to our setting. At present, it is unrealistic to use the RECALCAR activity data to establish causality for MDS-estimated health outcomes.
In summary, the 10 years of RECALCAR should be considered an undeniable success. The registry lays the groundwork for advances in comparative analyses of health care performance and for linking all steps taken to improve health outcomes, the ultimate aim of health care. As often seen in other successful projects, one of the best ways to achieve sustained results is ongoing development. We encourage RECALCAR to follow along the same lines.
FUNDINGThis editorial has received no funding.
CONFLICTS OF INTERESTThere are no potential conflicts of interest.