Mortality from acute coronary syndrome has fallen but a substantial number of chronic patients remain symptomatic. The present study was designed to determine the clinical characteristics and therapeutic treatment of patients with stable angina and its impact on their quality of life.
MethodsA cross-sectional, multicenter, observational study of 2039 patients with stable angina attended in outpatient clinics was performed. Data were collected on clinical variables and on the subjective perception of the severity of angina and the resulting limitations. Patients completed questionnaires on their perception of severity and quality of life.
ResultsWe analyzed data on 2024 patients; 73% were men (mean age 68 [10] years). Some 50.3% were asymptomatic (<1 angina attack per week in the previous 4 weeks), 39.2% reported 1-3 attacks per week and 10.5% reported >3 attacks per week; 66% had previously undergone revascularization, and 59% of these developed recurrent angina. Patients rated the severity of their condition higher than did their physicians (4.5 [2.5] vs 4.3 [2.3]; P=.002). Physicians’ and patients’ perceptions of the repercussions of angina showed little concordance (kappa<0.3). The patients believed their condition was much more severe, more debilitating, and had a greater negative impact on their quality of life.
ConclusionsA high proportion of patients with stable angina remains symptomatic and their quality of life is impaired. Their perception of the condition is worse than that of their physicians.
Keywords
.
IntroductionThe early recognition of acute coronary syndrome and prompt reperfusion techniques have reduced in-hospital and short-term mortality.1 There have also been changes in chronic ischemic heart disease: more patients undergo revascularization, medical treatment and control of cardiovascular risk factors (CVRF) have been intensified, and new treatments have appeared on the market. Nonetheless, in Spain, angina pectoris has not disappeared. The prevalence of angina is estimated to be 2%-4% in most European countries, with an annual mortality of 0.9%-1.4% and an incidence of nonfatal myocardial infarction of 0.5%-2.6%.2, 3 A significant number of patients with angina pectoris cannot be efficiently controlled; these patients have disabilities and their quality of life deteriorates, as shown in the RITA-24 and COURAGE5 studies. The Euro Heart Survey reports that, at diagnosis, 60% of patients with angina are moderately/severely limited in their daily activities.6 Angina pectoris frequently causes permanent disability and patients’ quality of life deteriorates markedly at a younger age than in patients with heart failure.7, 8 The World Health Organization considers ischemic heart disease to be the second cause of disability-adjusted life years lost9 after depression.
In Spain, knowledge of patients with stable angina is scarce. Subjectively, the issue appears to be of little relevance given improvements in the treatment of acute coronary syndrome. We consider it important to learn about standard cardiologic practice in patients with stable angina and to study physicians’ and patients’ perceptions of its impact on quality of life and of the general efficacy of treatment.
MethodsWe designed a cross-sectional, multicenter, observational study based on unrestricted, noninfluenced, single routine visits to clinical cardiologists in Spain. Given the difficulty of conducting a nationwide randomized study with measurement of quality of life, we decided to substantially increase the number of researchers—distributed proportionately throughout Spain's autonomous regions—and to limit the number of patients to 5 per researcher so as to avoid any individual selection bias that might affect the series.
Our principle objective was to determine the clinical characteristics of patients with stable angina and the treatment they receive. Furthermore, we designed the study to identify how patients and cardiologists perceive the condition and to determine its impact on patients’ quality of life.
Our inclusion criterion was “patient with a previous diagnosis of angina pectoris secondary to chronic ischemic heart disease attending a routine follow-up visit” at an outpatient cardiology clinic. Specifically, a confirmed clinical diagnosis of stable chronic angina (previous diagnoses of acute coronary syndrome, myocardial infarction or unstable angina) or chest pain with positive exercise testing were required. Patients aged <18 years, those included in clinical trials, and those who did not give their informed consent to the construction of the registry were excluded. The cardiologists recorded demographic, clinical and treatment variables. Using a questionnaire and a linear scale, they also reported subjective impressions of the severity of the disease and its resulting limitations.
After giving written consent and in the absence of the researcher, patients reported their perception of their condition in terms of its severity and their degree of disability. They completed two questionnaires: the Seattle Angina Questionnaire (SAQ),10 specifically about angina pectoris and validated in Spanish, and the SF-12 (12-Item Short-Form Health Survey),11 short form general quality of life questionnaire.
Justification of Sample Size and Method of Selecting ResearchersThe sample size was calculated assuming maximal indifference (p=q=0.5) in relation to the therapeutic management of patients and, to achieve a data precision of 2.3% (normal 95% 2-tailed distribution), a sample of 1800 valid patients was calculated. Assuming a 20% loss to follow-up, we began with an initial sample of 2250 patients. To avoid individual selection bias or systematic errors, we set the number of patients per physician at 5. The pre-established number of cardiologists was 450, distributed proportionately in relation to the Spanish population. The study's scientific committee used the Spanish Society of Cardiology Clinical Cardiology Section census to select 50 coordinators from different centers, chosen in proportion to their distribution across the country. After special training, the 50 coordinators each recruited 8 cardiologists working in general cardiology outpatient clinics in their area. The 450 cardiologists selected were instructed that the data collection period was strictly limited and that patients had to be consecutive or—if this was not possible—chosen using random criteria such as being the first patient of the morning diagnosed with stable angina or a similar disorder, to avoid any selection bias toward young or cooperative patients.
The study was approved by the principal researcher's clinical trial committee and, later, in each participating center.
The protocol and inclusion variables were developed by the scientific committee. A company independent of the project management and researchers was responsible for designing and producing the data collection folder, guaranteeing researcher anonymity, and conducting the preliminary analysis of the results.
Statistical AnalysisCategorical variables are described as frequencies and percentages; continuous variables as mean (standard deviation) or median [interquartile range], according to the distribution. Categorical variables were compared with Fisher's exact test; dichotomous continuous variables with the Student t-test, and variables with >2 categories with ANOVA. If assumptions of applicability were not met, we used the nonparametric Mann-Whitney U or Kruskal-Wallis tests. Correlations between variables were studied with the Pearson or Spearman correlation coefficients if parametric applicability was not met. Researcher-patient concordance in the subjective perception of severity of angina and the degree of its associated disability was measured with the kappa statistic. Statistical significance was set at a two-tailed 5%. Data were analyzed with SAS 9.1.3 (SAS Institute Inc., Cary, North Carolina, United States).
ResultsA total of 419 cardiologists participated in the study and 2039 patients were enrolled; 15 failed to meet the inclusion/exclusion criteria and were excluded, leaving 2024. All patients were attended in cardiology outpatient clinics; 68% of these were in-hospital and 32% in the corresponding specialist centers. Patients were enrolled between November 2009 and March 2010.
The distribution of patients and researchers by autonomous region is shown in Table 1. Differences in the percentage population of each region were ≤1%, indicating that the sample was representative. General patient characteristics are shown in Table 2.
Table 1. Distribution of Patients and Researchers by Autonomous Region (Spanish National Institute of Statistics’ Census 2010)
| Autonomous region | Cardiologists, no.(%) | Patients, no.(%) | Inhabitants, no.(%) |
| Andalusia | 72 (17.18) | 355 (17.54) | 8 370 975 (17.80) |
| Aragon | 9 (2.15) | 45 (2.22) | 1 347 095 (2.86) |
| Principality of Asturias | 11 (2.63) | 55 (2.72) | 1 084 341 (2.31) |
| Balearic Islands | 9 (2.15) | 43 (2.12) | 1 106 049 (2.35) |
| Canary Islands | 17 (4.06) | 72 (3.56) | 2 118 519 (4.51) |
| Cantabria | 5 (1.19) | 20 (0.99) | 592 250 (1.26) |
| Castile-La Mancha | 21 (5.01) | 101 (4.99) | 2 098 373 (4.46) |
| Castile and León | 20 (4.77) | 99 (4.89) | 2 559 515 (5.44) |
| Catalonia | 68 (16.23) | 323 (15.96) | 7 512 381 (15.98) |
| Extremadura | 13 (3.10) | 65 (3.21) | 1 107 220 (2.35) |
| Galicia | 24 (5.73) | 119 (5.88) | 2 797 653 (5.95) |
| Community of Madrid | 53 (12.65) | 260 (12.85) | 6 458 684 (13.74) |
| Region of Murcia | 14 (3.34) | 70 (3.46) | 1 461 979 (3.11) |
| Chartered Community of Navarre | 10 (2.39) | 50 (2.47) | 636 924 (1.35) |
| Basque Country | 23 (5.49) | 109 (5.39) | 2 178 339 (4.63) |
| La Rioja | 1 (0.24) | 5 (0.25) | 322 415 (0.69) |
| Valencian Community | 49 (11.69) | 233 (11.51) | 5 111 706 (10.87) |
| Total | 419 (100) | 2024 (100) | 46 864 418 (100) |
Table 2. General Characteristics of the Population Studied (n=2024)
| Men | 73.1 |
| Age, years | 67.8±10.4 |
| BMI | 28.6±4.2 |
| Abdominal obesity, % | 50.1 |
| SBP, mmHg | 135.3±17.7 |
| DBP, mmHg | 76.3±10.4 |
| HR, bpm | 66.6±11.1 |
| High blood pressure | 73.6 |
| Dyslipidemia | 75.7 |
| Diabetes mellitus | 33.8 |
| Current tobacco use | 8.5 |
| Kidney failure | 10.8 |
| PAD | 10.8 |
| History of stroke | 7 |
| Previous myocardial infarction | 49.9 |
| Heart failure | 13.2 |
BMI, body mass index; DBP, diastolic blood pressure; HR, heart rate; PAD, peripheral arterial disease; SBP, systolic blood pressure.
Data are expressed as no.(%) or mean±standard deviation.
Half the patients (50.3%) reported <1 angina attack per week within the previous 4 weeks (asymptomatic); 39.2% reported 1-3 attacks (oligosymptomatic), and the remaining 10.5% reported >3 (symptomatic).
Revascularization had been performed in 66% of the patients via coronary surgery (11.4%), percutaneous intervention (47.9%), or both (6.1%). Following revascularization, 59% of the patients developed recurrent angina. The median postrevascularization angina-free period was 8 [3-20] months.
Medical TreatmentWe studied antianginal drugs and CVRF drug treatments. The antianginal drugs administered were beta blockers (BB) in 77.6% of the patients, prolonged action nitrates in 53.1%, calcium antagonists in 40.4%, ivabradine in 10.9%, and trimetazidine in 7.3%. BBs were not administered to 22.4% of the patients, due to contraindications in 13.4% and intolerance in 6.5%. In 2.5%, the use of BBs was not considered.
In CVRF treatment, 96.3% received antiplatelet treatment (63.8% received acetylsalicylic acid only; other antiplatelet, 7.6%; 28.6% with dual antiplatelet therapy) 93.1% received a statin, 41.1% an angiotensin converting enzyme (ACE) inhibitor, and 32.5% angiotensin receptor antagonists (ARB). Anticoagulation therapy was administered to 10.1%.
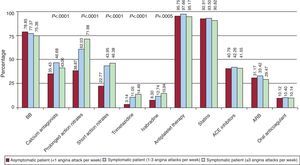
Antianginal treatment was more intensive in the more symptomatic patients but CVRF treatment was equally intensive in patients who were symptomatic, asymptomatic or had few symptoms (Figure 1). Treatment was considered optimal if a patient received an antiplatelet drug, a BB, a statin, and an ACE inhibitor or an. All four drugs were administered to 52% of patients, with no statistically significant differences as a function of the seriousness of the symptoms.
Figure 1. Medical treatment according to symptom intensity. Significant differences were found in the treatment of angina; more symptomatic patients received more antianginal treatment. There were no differences in treatment with beta blockers or in cardiovascular risk factors. ACE, angiotensin converting enzyme; ARB, angiotensin receptor blockers; BB, beta blockers.
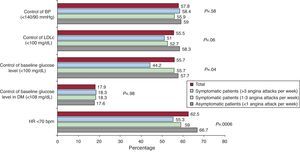
Control of CVRF was moderately effective (Figure 2). Differences in CVRF control levels were similar as a function of the presence of symptoms except heart rate. The percentage of patients with a heart rate<70 bpm was lower among those who were symptomatic (66.7% of asymptomatic, 59% of oligosymptomatic, and 55.3% of symptomatic patients; P<.001).
Figure 2. Percentage fulfillment of cardiovascular risk factor control objectives in the total number of patients and as a function of their symptoms. Cardiovascular risk factor control tended to be worse in the more symptomatic patients. This finding was statistically significant in baseline glucose level control in non-diabetic patients, and in attaining a <70 bpm baseline heart rate. BP, blood pressure; DM, diabetes mellitus; HR, heart rate; LDLc, low-density lipoprotein cholesterol.
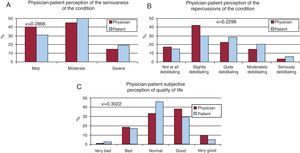
Perceptions of the ConditionIndependently of the seriousness of the angina, patients scored the severity of their condition higher than did their physicians (4.5 [2.5] vs 4.3 [2.3]; P=.002). When physicians’ and patients’ subjective perceptions of the repercussions of angina pectoris were compared, concordance was poor with κ≤0.3. Patients reported that their condition was more severe and more debilitating and that it detracted substantially from their quality of life more than did physicians (Figure 3).
Figure 3. Comparison of physicians’ and patients’ subjective perceptions of the repercussions of angina pectoris in relation to their subjective view of the seriousness of the condition (A), its repercussions on the patient (B) and physicians’ and patients’ subjective estimation of quality of life (C). The degree of concordance of between physicians’ and patients’ perceptions was low.
Table 3 shows the SAQ scores. Patients generally scored low, indicating that their condition caused them limitations, especially in terms of physical activity. The frequency of attacks and satisfaction with treatment were acceptable. The SF-12 general quality of life questionnaire tested different topics. In most of these, scores were very similar to those of the general population (50 points) but quality of life scores were low for physical exercise (37.9) and general health (36.4). This finding was interpreted as a loss of quality of life due to feeling ill, which negatively affected the capacity for physical exercise (Table 4).
Table 3. Seattle Angina Questionnaire Scores
| Overall description of Seattle Angina Questionnaire dimensions | |
| Physical limitations | 54.95±21.02 (53.98-55.91) |
| Stability of angina | 66.80±30.58 (65.42-68.17) |
| Frequency of angina | 83.24±20.69 (82.31-84.18) |
| Satisfaction with treatment | 75.47±15.71 (74.76-76.18) |
| Perceptions of the condition | 59.33±23.20 (58.28-60.38) |
0=maximum effect; 100=no repercussions.
Data are expressed mean±standard deviation (mean confidence interval).
Table 4. SF-12 Quality of Life Questionnaire Scores
| Overall description of standardized dimensions of SF-12 (v. 2) | |
| Standardized physical activity | 37.91±11.41 (37.39-38.44) |
| Standardized physical condition | 43.15±10.53 (42.67-43.63) |
| Standardized body pain | 46.22±12.13 (45.67-46.77) |
| Standardized general health | 36.46±10.32 (35.99-36.93) |
| Standardized vitality | 48.50±11.36 (47.97-49.02) |
| Standardized social function | 46.13±10.57 (45.65-46.61) |
| Standardized emotional aspects | 44.04±11.28 (43.52-44.55) |
| Standardized mental health | 49.16±10.23 (48.69-49.63) |
SF-12, 12-Item Short-Form Health Survey.
General population=50. Data are expressed as mean±standard deviation (mean confidence interval).
The AVANCE study follows a tradition of Spanish Society of Cardiology ischemic heart disease registries. After the PANES study,12 which contributed important epidemiologic data, and TRECE study,13 which contributed data on the treatment of these patients, AVANCE brings the demographic characteristics and treatments of patients with chronic stable angina in Spain up to date. Furthermore, this is the first study to show patients’ perceptions of their condition in comparison with those of their physicians, with measures obtained from a validated questionnaire on quality of life in patients with angina.
The baseline demographic characteristics of the AVANCE population (Table 2) are similar to those reported by TRECE, showing an increase in CVRF over the PANES sample (which reported only 31.1% with high blood pressure, 24.2% with dyslipidemia, 14.3% with diabetes and 34.6% smokers). We found a high prevalence of CVRF and a mean interval of 5.7 years since diagnosis of ischemic heart disease. Baseline treatments showed a higher percentage of drug use than in TRECE (conducted 5 years earlier) and other previous studies (Table 5),14, 15, 16, 17, 18, 19 and CVRF were better controlled (Figure 2).
Table 5. Progress of Stable Angina Treatment Over Time
| PREVESE I | EUROASPIRE I | Programa 3C | PREVESE II | EUROASPIRE II | EUROASPIRE III | TRECE | AVANCE | |
| Year | 1994 | 1995 | 1998 | 1998 | 1999 | 2006 | 2006 | 2010 |
| Patients, no. | 1329 | 4863 | 3074 | 2054 | 5556 | 8966 | 2897 | 2024 |
| BB, % | 33.3 | 34.7 | 37.4 | 45.1 | 47 | 80 | 64.5 | 77.6 |
| ACE inhibitors or ARB, % | 32.5 | 29.5 | 27 | 50.4 | 22 | 71 | 51.5 | 73.5 |
| Antiplatelet drugs, % | 89.7 | 81.2 | 84.1 | 87.8 | 86 | 91 | 84 | 96.3 |
| Statins, % | 6.7 | 32 | 27.5 | 29.4 | 60 | 78 | 75 | 93.1 |
ACE, angiotensin converting enzyme; ARB, angiotensin receptor blockers; BB, beta blockers.
Despite the increased use of drug treatments, high revascularization rate, and CVRF control, nearly half the patients in the registry were symptomatic and 10.5% had >3 angina attacks per week. At 8 months after revascularization, ≤60% of the patients had experienced symptoms of angina again. These data are similar to those in the COURAGE study, which compared optimal medical treatment with percutaneous revascularization in patients with chronic ischemic heart disease. The COURAGE researchers found that >30% of patients in both treatment branches were again symptomatic at 1 year of follow-up. In our study, medical treatment of symptomatic and asymptomatic patients was similar in the administration of drugs with a prognostic influence (ACE inhibitors/ARB, antiplatelet drugs, statins, BB, anticoagulation therapy), but symptomatic patients received more treatments to control symptoms (calcium antagonists, nitrates, trimetazidine, ivabradine) and were administered double antiplatelet therapy more frequently.
Perception of the Condition and Quality of LifeThe AVANCE study supports the findings of earlier publications showing that the limitations reported by patients are fundamentally physical, not mental, underscoring the appropriacy of our decision to study aspects of quality of life.
A total of 49.9% of patients rated their condition as moderately severe, >58% as little-to-somewhat debilitating and >75% described their quality of life as normal/good. On a visual analogic scale from 0 (absence of the condition) to 10 (maximum severity), patients recorded a mean of 4.34 (2.39) points. The SAQ produced results similar to those of the CADENCE study,20 conducted in patients with ischemic heart disease attended in primary care. In CADENCE, most patients had few symptoms of angina, with Canadian Cardiovascular Society (CCS) class I in 61% of the patients, CCS II in 29%, CCS III in 8%, and and CCS IV in 2% (in AVANCE these percentages were 35.6%, 50.7%, 13.1% and 0.7% respectively). Questionnaire scores on the stability and frequency of angina were similar but quality of life scores were lower in AVANCE, probably because our patients were more often symptomatic. However, our results for quality of life are similar to those of other studies in primary care,21, 22 in which ≤30% had ≥2 angina attacks per week, and studies in outpatient cardiology clinics,23 in which 40.9% had 1 attack per week. In all these studies, the proportion of patients with intensive symptoms is similar (CCS III-IV in around 10%-15%) despite their having been published over the last decade and, therefore, having incorporated advances in medical treatment and percutaneous and surgical revascularization.
The present study shows that patients perceive their condition as being more serious than do their physicians, independently of symptom intensity. Statistical concordance between physicians and patients was low. In the literature, we have found no study that supports this finding and therefore believe it should be corroborated through new research. However, we consider it an important warning not to underestimate patients’ perception of their angina.
This lack of statistical significance also appeared in the concordance between physicians’ and patients’ perceptions of the efficacy of medical treatment (Figure 4) and the physicians were again found to underestimate their patients’ condition. Treatment efficacy was rated higher by asymptomatic patients and fell as the number of angina attacks per week increased. The general SAQ score for “satisfaction with the treatment” was 75.5 points, 7 points lower than that obtained in a study published 9 years ago, in which treatment satisfaction achieved a score of 82 points (maximum satisfaction, 100; minimum, 0), indicating that patients’ perception of angina treatment has changed little in the last decade.
Figure 4. Comparison of physicians’ and patients’ perceptions of the efficiency of treatment for symptoms associated with the condition. A: asymptomatic patients (<1 angina attack per week). B: patients with few symptoms (1-3 angina attacks per week). C: symptomatic patients (>3 angina attacks per week). General concordance was not good, but was much worse in symptomatic patients, who believed themselves to be much more debilitated than did their physicians.
LimitationsThe quality of the diagnosis of angina was not validated with a standard questionnaire. However, as diagnosis took place in a context with easy access to cardiology tests to detect ischemia and with high percentages of patients with previous infarction and revascularization who were symptomatic, we believe the number of false positives should be quite small. Precisely because of this, the percentage of symptomatic patients could have increased over earlier primary care series, such as CADENCE, in which 39% were symptomatic. Another potential limitation is the nonrandomization of participating physicians. However, as explained in “Methods”, we tried to minimize selection bias by increasing the number of participating physicians and limiting the number of patients per physician to a maximum of 5.
ConclusionsTreatment of stable ischemic heart disease has progressed over the last decade. Cardiovascular risk factors are better controlled, more coronary revascularization procedures are performed, and new medication has appeared. Nonetheless, a high proportion of symptomatic patients remains. Patients’ and physicians’ perceptions of the condition differ. In general, physicians perceive the disease as less severe and less debilitating than do the patients. Moreover, patient satisfaction with antianginal treatment remains similar to that reported 9 years ago.
FundingThis project was conducted with an unconditional research grant from Laboratorios Menarini S.A.
Conflicts of interestNone declared.
Appendix A. AVANCE study researchers (in alphabetical order)S. Aban Alique, A.C. Abecia Ozcariz, P. Aguiar Souto, R. Aikurdi Raggub, J.A. Alarcon Duque, C. Albarran Martin, M. Alvarez Sanchez, H.M. Alviso de Vargas, C. Amador Gil, V. Amaro Arroyo, I.J. Amat Santos, C. Amo Fernandez, C. Amoros Galito, R. Andion Perez, R. Andrea Riba, J. Andres Novales, G.F. Angulo, F.J. Antona Makoshi, C. Aracil Espi, J.C. Arias Castaño, A. Arias Recalde, X. Armengol Castells, M.A. Arnau Vives, F. Aros Borau, V.I. Arrarte Esteban, A. Arribas Jimenez, J. Arrobas Vacas, M.C.E. Avila Escribano, P. Awamleh Garcia, M. Azcarate Pascual, J.R. Balaguer Malfagon, L. Banchs Galtes, M. Baquero Alonso, G. Baron Esquivias, A. Barragan Acea, V. Barriales Alvarez, J. Bassaganyas Vilarrasa, A. Batalla Cleorio, V. Bazan Gelizo, N. Bellera Gotarda, J. Benezet Mazuecos, E. Bernal Labrador, M.T. Beunza Puyol, D. Bierge Valero, R. Bilbao Quesada, M.J. Bosch Campos, V. Brossa Loidi, H. Brufau Redondo, J. Caballero Güeto, J. Cabezon Gutierrez, F. Cabrera Bueno, F.A. Cacace, O. Caldes Llull, F. Calvo Iglesias, R. Campo Perez, J.V. Campos Perez, J.V. Campos Peris, M. Camprudi Potau, M.D. Cano Albaladejo, L. Cano Calabria, J. Caparros Valderrama, J.F. Carretero Ruiz, P.J. Casas Gimenez, M.S. Cascon Bueno, J.M. Castaños del Molino, A. Castilla Nuñez, J.E. Castillo Lueña, M. Castillo Orive, D. Cervantes Chavez, C.I. Chamorro Fernandez, P.A. Chinchurreta Capote, J.M. Chopo Alcubilla, V. Climent Paya, J.L. Colomer Marti, C. Corona Barrio, J.F. Corral Fernandez, R. Cortes Sanchez, G. Cortez Quiroga, R. Cortina Rodriguez, J. Cosin Sales, D. Cremer Luengos, A.J. Criado Millan, J.M. Cuesta Cosgaya, G. Cuevas Tascon, C. Culebras Caceres, A. Curcio Ruigomez, S. Darnes Soler, T. Datino Romaniega, E. Davila Davila, C. de Ancos Aracil, R. de Castro Aritainoiz, J.M. de la Hera Galarza, S. del Castillo Suarez, I. Diaz Buschmann, E. Diaz Caraballo, O. Diaz Castro, M. Diaz Escofet, I. Diez Gonzalez, S. Diez-Aja Lopez, C. Dorta Macia, J.M. Enjuto Olabera, F. Ereño Beroiz, C. Escobar Cervantes, L. Escosa Royo, J. Ezkurdia Sasieta, F. Fabra Utrai, L. Facila Rubio, A. Fajardo Pinedo, C. Falces Salvador, P. Federico Zaragoza, C. Feliu Zamora, A. Feria Herrera, M.A. Fernandez Fernandez, L.A. Fernandez Lazaro, L.C. Fernandez Leoz, G. Fernandez Mora, R. Fernandez Pantoja, J. Fernandez Pastor, J. Fernandez-Dueñas Fernandez, M. Fernandez-Valls Gomez, B. Ferreiro Rodriguez, A. Flores Pedauye, J.M. Forcada Sainz, A. Francino Batlle, J.L. Francisco Matias, J.M. Franco Zapata, J. Freire Corzo, J.M. Frigola Marcet, B. Frutos Perez, J. Fuentes Alonso, J. Furundarena Zubiria, D. Gaitan Roman, E. Galindo Nogueras, J.M. Gallego Garcia, E. Galve Basilio, J.M. Gamez Martinez, J.M. Garcia Acuña, F.J. Garcia Almagro, M. Garcia Alvarez, C. Garcia Garcia, F. Garcia Gonzalez, A. Garcia Honrubia, M. Garcia Martinez, M. Garcia Navarro, C. Garcia Palomar, J.M. Garcia Pinilla, E. Garcia Porrero, A. Garcia Quintana, L. Garcia Riesco, F.J. Garcia Solar, J.M. Garcia de Andoain Rays, M. Garcia de la Borbolla Fernandez, B. Garcia de La Villa Redondo, X. Garcia-Moll Marimon, M. Garrido Uriarte, C. Garrote Coloma, F. Garza Benito, D.I. Gentille Lorente, H. Gervas Pabon, I. Gil Ortega, J.J. Gomez Barrado, S. Gomez Moreno, I. Gomez Otero, M. Gomez Perez, H. Gonzalez Gutierrez, O. Gonzalez Lorenzo, I. Gonzalez Maqueda, P. Gonzalez Perez, C. Gonzalez Rios, M. Gonzalez-Valdayo Lopez, A.E. Gordillo Higuero, M. Gracia Aznarez, G. Grau Jornet, A. Guisado Rasco, O. Guri Baiget, B. Gutierrez Escalada, E. Gutierrez Ibañes, F. Gutierrez Rosch, J. Hernandez Alfonso, M. Hernandez Martinez, J.M. Hernandez Riesco, D. Herrera Fernandez, J.S. Hevia Nava, A.I. Huelmos Rodrigo, R. Huerta Blanco, C. Iborra Cuevas, G. Iglesias Cubero, I. Iglesias Garriz, E. Iglesias. Rio, R. Issa Khozouz, B. Jimenez Araque, J. Jimenez Bello, A. Jimenez Elorza, J.J. Jimenez Nacher, J. Julia Gibergans, C. Kallmeyer Martin, E. Kaplinsky, J.M. Lacal Peña, J. Lacalzada Almeida, C. Lafuente Gormaz, J.A. Lastra Galan, I. Laynez Cerdeña, J.R. Lopez Salguero, F.A. Lopez Sanchez, I. Lozano Martinez-Luengas, J. Lujan Martinez, J.A. Madrigal Vilata, L. Mainar Latorre, H. Marrero Santiago, S.C. Marti Linares, A. Martin de la Higuera, J. Martin Moreiras, J. Martin Pastor, R. Martin Reyes, J.F. Martinez Rivero, M.D. Martinez Ruiz, F. Martínez Garcia, E.J. Martinez de Morentin Laurenz, M. Martinez-Selles D’Oliveira-Soares, F. Martos Ferres, M. Mateos Garcia, P. Mazon Ramos, A. Megias Saez, A. Melero Pita, I. Mendez Santos, O. Meroño Dueñas, R. Miguel Montero, F. Milone Prado, G. Miñana Escriva, S. Mirabet Perez, I. Molina Avila, I.C. Möller Bustinza, V. Montagud Balaguer, M.A. Montero Gaspar, A Montiel Trujillo, A.M. Montijano Cabrera, J. Mora Robles, M. Morales Fornos, R. Morales Perez, L. Morcillo Hidalgo, J.M. Moreno Salcedo, N. Moreno Sanchez, A. Morillas Fernandez, J.L. Moriñigo Muñoz, P. Mota Gomez, A. Munarriz Arizcuren, J.J. Muñoz Gil, M. Muñoz Robles, N. Murga Eizagaechevarria, F. Narro García, E. Nasarre Lorite, L.F. Navarro del Amo, C. Navas Navas, A.M. Nieto Rodriguez, R. Numancia Andreu, D. Nuñez Pernas, J. Nuñez Villoja, C. Olalla Gomez, F. Olaz Preciado, L.C. Olivan Sayrol, A. Ordoñez España, M. Orejas Orejas, M.C. Orive Martinez, J. Orruño Aguado, V.M. Ortiz Martinez, J.T. Ortiz Perez, I. Otaegui Irurueta, E. Otero Chulian, M. Padilla Perez, C. Palanco Vázquez, P. Palau Sampio, O. Palazon Molina, S. Palomar Garcia, V. Pardo Guirera, E. Paredes Galan, F.J. Pascual Garcia, P. Pazos Lopez, J.M. Pazos Mareque, M. Pedreira Perez, M.J. Pellicer Bañuls, R. Peñafiel Burkhardt, J. Perez Asenjo, P. Perez Berbel, A.I. Perez Careza, H. Perez Hernandez, S. Perez Ibiricu, M.A. Perez Martinez, C. Perez Muñoz, E. Peris Domingo, A.M. Peset Cubero, R. Piedra Ozcariz, E. Pinar Bermudez, J. Pinar Sopena, C. Pindado Rodriguez, A. Piñero Lozano, F. Planas Ayma, F. Planas Comes, J. Plaza Carrera, M.T. Poblet Farres, F.J. Polo Romero, J.C. Ponce de Leon Vaccarino, F. Pons Sole, Y. Porras Ramos, J.C. Porro Fernandez, H. Pousibet Sanfeliu, E. Prieto Moriche, B. Puente Rodero, M. Puig Cid, E. Pujol Iglesias, J. Quintana Figueroa, R. Ramirez Rodriguez, F. Ramos Latorre, I. Rayo Llerena, E. Recalde del Vigo, L. Recasens Gracia, A. Revello Bustos, M. Ribas Garau, M. Ribas Sitjas, F. Ridocci Soriano, T. Ripoll Vera, A. Rius Davi, M. Rizzo, J. Robledo Carmona, P. Robles Velasco, L.J. Rodriguez Collado, A. Rodriguez Fernandez, J.A. Rodriguez Fernandez, J.A. Rodriguez Hernandez, J.A. Rodriguez Ortega, I. Rodriguez Sanchez, D. Roldan Conesa, I. Roldan Rabadan, P. Rollan Garcia, D. Romero Alvira, R. Romero Garrido, E. Romo Peñas, M. Roque Moreno, J.A. Rubio Caballero, J.M. Rubio Campal, R. Rubio Paton, A.M. Rubio Perez, E. Rueda Calle, J. Rueda Soriano, M. Ruiz Borrell, S. Ruiz Bustillo, S. Ruiz Leria, M. Ruiz Ortiz, J.A. Ruiz Ros, J. Ruiz de Castroviejo del Campo, P.M. Rull Murillo, O.R. Saavedra Garcia, F. Sabatel Lopez, I. Sagasti Aboitiz, F. Sagues Gabarro, I. Sainz Hidalgo, A. Sainz Viard, J. Sala Montero, A. Salas Lobato, P. Salinas Sanguino, A. Salvador Sanz, J.A. San Roman Calvar, L. San Vicente Urondo, P. Sanchez Chamero, J. Sanchez Quiñones, R.M. Sanchez Soriano, J. Sanchez Torrijos, J.L. Sanchez-Puerta Vera, M. Sanmartin Fernandez, E. Santas Olmeda, B. Santos Gonzalez, M.L. Sanz Rodriguez, R. Sanz Ruiz, M. Sanz Sanchez, F. Sarnago Cebada, I. Secura Laborda, M. Sedano Varela, F. Segura Villalobos, B. Seldelberger, V. Serra Garcia, P. Serrano Aisa, S. Serrano Garcia, A. Serrano Romero, J.R. Siles Rubio, J.C. Soriano Gimenez, A.J. Sualis Abadal, P.L. Talavera Calle, A.V. Tapia Tirado, A. Tarabini-Castellani Rizzo, A. Tello Valero, P. Toledo Frias, J.M. Tolosana Viu, A. Toral Noguera, F. Torres Calvo, J. Torres Marques, F. Trujillo Berraquero, M.A. Ulecia Martinez, J. Umaran Sanchez, I.M. Ureña Montilla, E. Uribe Echeverria Martinez, O.A. Vaccari, R. Valdivia Gutierrez, E. Valles Gras, A. Varela Roman, C. Vaticon Herreros, A. Vazquez Garcia, J. Vega Fernández, C. Vehi Gasol, E. Velasco Espejo-Saavedra, A. Velasco Vitrian, B. Vidal Hagemeijer, R.C. Vidal Perez, M. Vila Perales, M. Vilar Freire, M.A. Villanueva Terrazas, C. Villar Mariscal, L. Wu Amen, J.C. Yañez Wonenburguer, M.S. Yravedra Bosque, M.J. Zarauza Navarro.
Received 7 November 2011
Accepted 4 March 2012
Corresponding author: Servicio de Cardiología, Hospital de la Santa Creu i Sant Pau, Sant Antoni Maria Claret 167, 08025 Barcelona, Spain. xborras@santpau.cat