Keywords
INTRODUCTION
The compilation of registries of activities involving different techniques, especially the more modern techniques or those which are evolving faster in consonance with technological development, not only enables the relevant indications to be kept up to date, but also allows the scientific community to know what is being done. For the third consecutive year we present the results of the Spanish Catheter Ablation Registry, this time with the data for 2003 drawn up by the Working Group on Electrophysiology and Arrhythmias of the Spanish Society of Cardiology.
MATERIAL AND METHODS
Data were collected in 2 different ways, prospectively and retrospectively. Each center was free to choose the method, though the registry-coordinating center recommended the prospective data collection. Retrospective data were obtained with a standard questionnaire, similar to that used in previous years,1,2 and which was sent by postal or electronic mail to all the laboratories. Briefly, the first part of the questionnaire gathered information about the hospital and the main human and material resources available to the electrophysiology laboratory.3,4 The second part concerned the number of procedures and the outcomes according to the substrate or arrhythmic mechanism targeted. Seven different substrates were considered: atrioventricular nodal reentrant tachycardia (AVNRT), accessory pathways (AP), atrial flutter, ventricular tachycardia (VT), atrioventricular node ablation (AVN), atrial fibrillation (AF), and focal atrial tachycardia (FAT). Data were collected for each substrate-mechanism on the total number of procedures and patients treated, the number of successful procedures and successfully treated patients, the number of procedures performed with different types of catheters, and the number and type of complications.
Prospective data were obtained from a computerized database created by the coordinators and sent to all the centers by electronic mail before the end of 2002. The database consisted of 2 different questionnaires. The first, which was similar to the prospective questionnaire, was designed to collect general information about the hospital, and the characteristics of the laboratory and the electrophysiology equipment. The second questionnaire was to be completed after each ablation procedure, with general data (age, sex, history of heart disease, prior procedures, sedation used, anticoagulation during the study, type of catheter, approach, substrate, result, and type of complications if present) and other specific data depending on the type of substrate treated.
Once completed, the retrospective questionnaires and the databases of the prospective registries were sent to the secretariat of the Working Group on Electrophysiology and Arrhythmias, where administrative staff assigned them a number (center code) and removed the center identification, which was filed separately to ensure the confidentiality of the information provided. The rest of the questionnaire or database was forwarded to the coordinators of the registry for analysis.
Statistical Analysis
Numerical results were expressed as mean ± standard deviation (SD). Qualitative variables and proportions were analyzed using the χ² test and Fisher's test if necessary. A P-value <.05 was considered statistically significant. The statistical analysis was performed with the SPSS 11.0 program.
RESULTS
Thirty-nine centers participated in the registry; 25 (64%) provided prospective data on the ablation procedures and 14 completed the questionnaire retrospectively. The participating centers and their geographical distribution are shown in Annex 1. All the centers were included in the final analysis as they all completed the questionnaires correctly, except for 1 center which failed to complete the data concerning general information. The section concerning infrastructure and resources was therefore analyzed for 38 centers.
Infrastructure and Resources
The general characteristics of the participating centers are shown in Table 1. Regarding the technical equipment available to the electrophysiology laboratory, 13 centers (34%) had a digital x-ray machine in the room where the ablation procedures were carried out. The average number of days dedicated to electrophysiology by the group was 3.29 (range, 1-5 days), with the room used exclusively for electrophysiology procedures in 27 centers (71%). Besides ablation procedures, 24 centers (63%) also used the room for implantation of pacemakers or automated implantable defibrillators (AID), 1 for the implantation of biventricular stimulation devices, 7 for the implantation of a Holter, and 5 also used the room for tilt table tests. Fifteen centers (39%) undertook external electric cardioversion in the electrophysiology laboratory, 10 (26%) both external and internal cardioversion, and 5 (13%) just internal cardioversion. No electric cardioversion was undertaken in the electrophysiology laboratory of 8 centers.
Regarding the technical equipment available for ablation procedures, 35 centers (92%) had a digital polygraph system. Moreover, 17 centers (44%) also had nonfluoroscopic intracardiac navigation systems: 4 centers used the CARTO® system, 9 the Localisa®system, 1 the RPM® system, 1 CARTO® and Localisa®, 1 CARTO® and RPM®, and 1 CARTO®, Localisa® and RPM®. Two centers failed to answer this question. Nine centers (23%) also used intracardiac echocardiograms as a tool to aid ablation and 2 centers used cryoablation as an alternative energy source to radiofrequency.
Table 2 shows the human resources available at each center. Data for the 33 publicly funded centers included the following: the number of physicians dedicated to electrophysiology ranged from 1-4 (mean and median of 2), whereas the mean number of full-time physicians was 1.4. Four centers (12%) had no full-time physician available for this task. Ninety percent of the centers had fellows (1.2 residents per year) and 36% (n=12) had grant holder physicians (0.57 holders per year). Two or more registered nurses were working in 18 centers (54%) and 5 centers (15%) had a radiological technical assistant in the electrophysiology laboratory.
Twenty-four centers performed transseptal catheterization as the approach to different arrhythmogenic substrates. In 11 centers (45%) this procedure was performed exclusively by electrophysiologists, in 7 (29%) by interventional cardiologists, and in 6 (25%) by both. The prospective registry provided the opportunity to specify what types of ablation had been done with the transseptal approach or via a patent foramen ovale. Transseptal puncture was performed in 78 AF ablations, in 22 AP, in 13 FAT, in 9 atrial flutter and in 1 VT, whilst a patent foramen ovale was used for ablation of 10 AF, 11 AP, 1 left atrial flutter, 1 VT and 2 AVNRT.
Overall Results
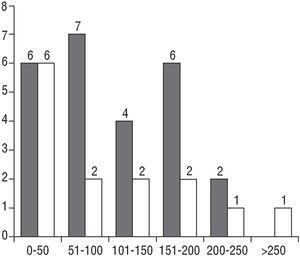
The total number of ablations recorded was 4354, of which 2723 (62.5%) were in the prospective registry and 1631 (37.4%) in the retrospective registry, giving a mean of 111±81.3 (range, 7-410) ablations per center. Figure 1 shows the distribution of the number of procedures per center. The overall percentage success rate per procedure was 91%, the rate of major complications was 1.7% (n=75) and the perioperative mortality rate was 0.11% (n=5).
Fig. 1. Number of centers according to the number of catheter ablation procedures performed in 2003. Prospective registry in gray bars and retrospective registry in white bars.
The result of the ablation was analyzed separately in both types of registry. The overall success rate of the retrospective registry was 91.8% (1496 effective procedures, 132 non-effective and 3 failed to answer). The overall effectiveness of the prospective registry was 89% (2420 effective procedures, 279 non-effective, and 24 failed to answer), which was statistically significant (P=.018).
The prospective registry also provided certain demographic characteristics about the patients, such as their median age, which was 50 years (range, 0-89 years) and 54% of the patients who underwent ablation were male. The prospective registry also revealed that 20% of the patients had heart disease associated with arrhythmia and that 2% had an AID.
The 2723 ablations in the prospective registry were performed in 2558 patients. In 55 of these patients (2%) 2 different substrates were treated in the same procedure and 110 (4%) underwent more than 1 procedure during 2003. Also, 143 patients (6%) had undergone some prior procedure before 2003. The reason for the new ablation was relapse after an effective procedure in 41% of the cases, lack of efficacy of the prior procedure in 25%, a different substrate in 15%, and other reasons in 8% (no answer was provided for 10% of those who had a prior procedure). Of the patients with a prior procedure, 275 had just one, 44 had undergone 2, 6 had undergone 3, and 4 had undergone 4 previous ablations. The most frequently targeted substrate was VT (18%), followed by AP, FAT and AF (12%), atrial flutter (10%), and, lastly, AVN and AVNRT (4%). Sixty-nine patients (2.5%) from the prospective registry had the ablation procedure under general anesthesia, with sedation being used in 1396 (51.2%) patients.
Results by Substrate
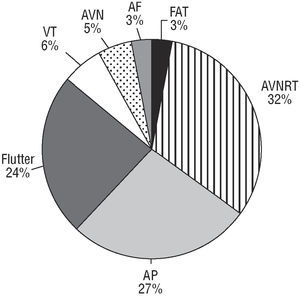
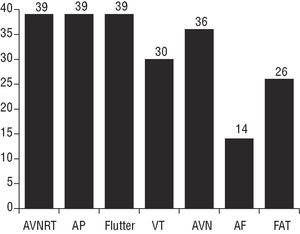
Of the 7 different substrates studied (Figure 2 and Table 3), the most frequently targeted was AVNRT, with 1377 ablations (31.6% of the total). The second most frequent substrate was AP, with 1149 procedures (27%), followed by atrial flutter with 1035 procedures (24%). Fewer procedures were carried out for VT (258 procedures, 6%), AVN (243 procedures, 5%), AF (151 procedures, 3%), and FAT (141 procedures, 3%). Of the 39 centers included, 15 (38%) performed ablation of all 7 substrates included in the registry, 9 (23%) centers performed ablation of 6 substrates, 8 centers performed ablation of 5 substrates, 6 centers performed ablation of 4 substrates and 1 center performed ablation of 3 different substrates. As can be seen in Figure 3, all the centers performed ablation of the AVNRT, AP and atrial flutter, whereas ablation of the AF was performed only in 14 centers (35%).
Fig. 2.Relative frequency of the different substrates treated by catheter ablation during 2003. AVNRT indicates atrioventricular nodal reentry tachycardia; AP, accessory pathways; VT, ventricular tachycardia; AVN, atrioventricular node ablation; AF, atrial fibrillation; FAT, focal atrial tachycardia.
Fig. 3. Number of electrophysiology laboratories targeting the different substrates. AVNRT indicates atrioventricular nodal reentry tachycardia; AP, accessory pathways; VT, ventricular tachycardia; AVN, atrioventricular node ablation; AF, atrial fibrillation; FAT, focal atrial tachycardia.
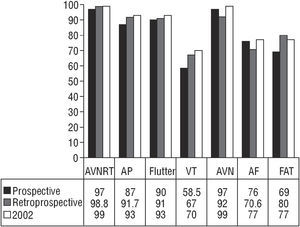
Certain specific characteristics of each substrate treated are given below. The general data come from the combination of both registries, with certain specific information taken mainly from the prospective registry. The overall results by substrate in each type of registry and comparison of the results with those of 2002 are summarized in Figure 4.
Fig. 4. Percentage succes rate of catheter ablation by substrate, comparing the results of the 2002 registry (white bars) with those of the prospective (black bars) and retrospective (gray bars) registries of 2003. AVNRT indicates atrioventricular nodal reentry tachycardia; AP, accessory pathways; VT, ventricular tachycardia; AVN, atrioventricular node ablation; AF, atrial fibrillation; FAT, focal atrial tachycardia.
Atrioventricular Nodal Reentry Tachycardia
Once again, the most frequently targeted arrhythmogenic substrate was AVNRT, with a total of 1377 ablations (35.3±25.58 procedures per center; range, 2-129). The success rate per procedure was 98.8% in the retrospective registry and 97% in the prospective registry (P=NS). The mean age of the patients who underwent ablation for AVNRT in the prospective registry was 49 years (range, 9-86) and 70% were women. The intranodal ablation procedures failed to induce tachycardia during the procedure in 6% (n=47) of the cases, in spite of which ablation was still performed. Isoproterenol was used in 62% of the procedures and intravenous atropine in 4%; in the remaining 34% no type of facilitating drug was used. Ablation of the fast pathway was undertaken in just 4 cases. Complications were recorded in 12 (0.8%) procedures, 2 (0.1%) complete atrioventricular (AV) blocks which required the implantation of a permanent pacemaker, 4 transitory AV blocks which did not require pacemakers, 1 arterial complication, 1 pericardial effusion which resolved without the need for puncture and 4 minor complications.
Accessory pathways
The AP were targeted in 1149 ablations (30.23±22.1 per center; range, 4-102). The overall success rate was 91.7% in the retrospective registry and 87% in the prospective registry (P=.02). Of the 725 AP ablations in the prospective registry, 12% of the patients had already had a prior ablation procedure. The mean age of the patients was 39 years (range, 9-78) and 56% were men. In those cases where the accessory pathway was patent, the most frequent site was the left, around the mitral ring, involving 57% of the cases (43% free wall and 14% inferior septal), with the remaining 43% located in the right side of the heart (7% free wall, 24% inferior septal, and 12% around the bundle of His). In those cases in which the AP had just one hidden conduction, the rate of left wall locations rose to 78% of the cases (68% free wall and 10% inferior septal), compared with 22% of cases of right wall locations (2% free wall, 12% inferior septal, and 8% around the bundle of His). No variation in the overall success rate was seen according to whether the pathway was hidden or patent (87.2% vs 86.9%, respectively), whereas a right or left location affected the result significantly (80.1% vs 91.2% , respectively; odds ratio [OR] =3.39 [range, 2.06-5.62]; P<.01). The efficacy of the procedure was also different, depending on whether the site was the free wall, inferior septal or the area around the bundle of His (91.6% vs 83.1% vs 72.8%, respectively; P=.05). Most of the ablations of the left AP (307 ablations, 72%) were performed with the empiric use of heparin sodium, 17 (4%) with heparin sodium according to the activated partial thromboplastin time (APTT), 10 (2%) with low molecular weight heparin and in 91 (21%) no anticoagulation was used. In 688 of the 722 cases specified, the catheter used initially had a 4 mm tip (in 13 of these it was necessary to change to an 8 mm tip catheter, in 19 to an irrigated tip catheter and in 2 a cryoablation catheter). Ablation was started in 5 cases with an 8 mm tip catheter, in 15 with an irrigated tip catheter and in 14 with a cryoablation catheter. Complications arose in 23 procedures (2%). Four patients (0.3%) suffered a complete AV block which required the implantation of a permanent pacemaker, and 2 had transitory block which did not require a pacemaker. There were also 8 arterial complications, 1 stroke and 8 minor complications.
Macroreentrant Atrial Tachycardia/Atrial Flutter
A total of 1035 ablations were performed in this substrate (26.52±23.3 per center; range, 1-104). The success rate was similar in both types of registry (91% and 90%) (P=NS). Data concerning the 644 ablations targeting this substrate in the prospective registry showed that the mean age of the patients was 61 years (range, 5-89 years) and that 76% were male. Most procedures were undertaken for a typical atrial flutter, with an overall success rate of 92%; 15 ablations were undertaken for scar flutter, with a success rate of 66%; and 10 in the left atrium, with a success rate of 33%. Two procedures were performed for flutter of the inferior vena cava and 3 elsewhere in the right atrium. The most commonly used catheter was the 8-mm tip (78%), followed by the irrigated tip catheter (16%), and the 4-mm tip catheter (5%). No intra-operative anticoagulation was used in 70% of the ablations, the empiric use of heparin sodium or depending on the APTT in 19%, and low-molecular weight heparin in the remaining 10%. Complications were reported in 18 (1.8%) procedures, with 2 deaths after ablation of this substrate. Two patients required the implantation of a permanent pacemaker because of complete AV block, 1 had a transitory AV block, 3 had pericardial effusion, 1 had an arterial complication, 2 had a cerebrovascular event, and 9 had minor complications.
Ventricular Tachycardia
A total of 258 ablations were performed for VT (8.6±7.4 per center which treated this substrate; range, 1-33). The success rate per procedure was 58.5% in the prospective registry and 67% in the retrospective registry (P=NS). The mean age of the patients who underwent the 181 ablations in the prospective registry was 56 years (range, 0-89) and 74% were male. The aim of the ablation in most procedures was to suppress clinical VT (63.8%); 8% of procedures were targeted to suppress a non clinical VT, 9% an incessant VT, 7% to make ablation lines in the ventricle or suppress post-infarction scars and, finally, 14% were to suppress ventricular extrasystole. Regarding the underlying heart disease, 45% of the patients had ischemic heart disease, 9% dilated cardiomyopathy, 2% dysplasia of the right ventricle (RV), and 36% had no obvious organic heart disease. The most frequently targeted idiopathic VT, in which evaluation of the efficacy of the ablation is more objective, was that originating in the outflow tract of the RV (59% of all the idiopathic VT), with an efficacy rate of 73%. Eight percent originated in the outflow tract of the left ventricle (50% success rate) and 17% in the posteroinferior fascicle of the left bundle branch (84% success rate). Ablation was performed with a 4-mm tip catheter in 75% of the cases, with the remaining procedures employing an 8-mm tip catheter or an irrigated catheter (11% and 12%, respectively). A total of 13 (5%) patients had complications, with 2 deaths. Two patients had complete AV block which required implantation of a pacemaker, 1 had a transitory AV block, 3 had arterial complications, 5 had pericardial effusion or tamponade, 1 had a cerebrovascular event, and 1 had decompensation of heart failure.
Atrioventricular Node Ablation
A total of 243 AVN ablations were performed (6.75±4.9 per center in those which targeted this substrate; range, 1-19). The efficacy was 97% in the prospective registry and 92% in the retrospective registry (P=NS). The patients who underwent the 164 ablations in the prospective registry had the highest mean age for all the substrates, at 65 years (range,
35-84) and 57% were women. The aim of the ablation was modulation of the AVN in 7 cases (4.2%). The underlying arrhythmia in 53% of cases was chronic AF, in 25% paroxystic AF, in 17% atypical atrial flutter, and in 4% atrial tachycardia. A left (arterial) approach was made in 4.8% of the cases. The procedures were performed with a 4-mm tip catheter in 83% of the ablations, an 8-mm tip catheter in 15% and catheter cryoablation in 1%. Four complications (1.6%) and 1 death were reported. Three of the complications were secondary to pericardial effusion or tamponade and 1 was a minor complication.
Focal Atrial Tachycardia
A total of 141 ablation procedures were performed on this substrate (5.03±4.3 per center which targeted this substrate; range, 1-22). The success rate was 69% in the prospective registry and 80% in the retrospective registry (P=NS). The mean age of the patients who underwent the 76 ablations in the prospective registry was 49 years (range, 10-85) and 62% were female. The right atrium was the site of origin in 63% of cases, with a success rate of 80%; the area around the bundle of His was the site of origin in 11% (66% success rate) and the left atrium in 23% (73% of these in a pulmonary vein, with a 40% success rate). Only 1 minor complication was reported (0.7%).
Atrial Fibrillation
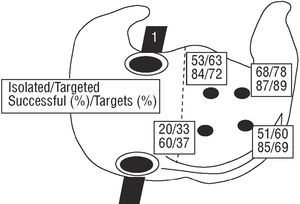
A total of 151 ablations were undertaken for AF (10.78±9.7 per center which undertook AF ablation; range, 1-36). The procedure was considered effective in 76% of the ablations in the prospective registry and in 70.6% of the ablations in the retrospective registry (P=NS). The mean age of the patients who underwent the 93 ablations in the prospective registry was 50 years (range, 28-80) and 54% were male. The aim of the ablation was electric isolation of the pulmonary veins in 89% of the procedures. Figure 5 shows the number of times and percentage that each pulmonary vein was targeted and isolated successfully in the 87 ablations in which this information was provided. The left upper, right upper, and left lower pulmonary veins were targeted most frequently (89%, 72%, and 69%, respectively). Only in 15 procedures was complete isolation of 3 veins (17%) achieved, while all 4 veins were isolated in 19 cases (21%). The catheter most often used was the irrigated catheter (50%), followed by the 4-mm tip catheter (46%), the 8-mm tip catheter (2%), and a cryoablation catheter (1%). A nonfluoroscopic navigation system was used in 78% of the cases. Anticoagulation with the empiric use of heparin sodium was used during the procedure in 54% of cases, with heparin according to the APTT in 41% of cases. No anticoagulation was used during the procedure in just 4% of cases. Four complications (2.6%) were reported: 1 pericardial effusion-tamponade because of perforation of the left leaflet, 1 suprarenal hemorrhage and 2 minor complications.
Fig. 5. Number of times each pulmonary vein was targeted and isolated in atrial fibrillation ablation, as well as the percentage of overall targets and successful isolation. Data from the prospective registry (n=87 procedures).
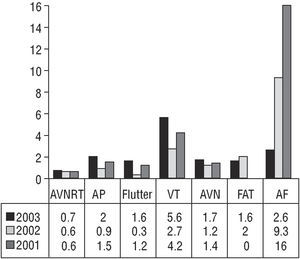
Complications
A total of 75 complications (1.7%) were reported, 15 (0.9%) in the retrospective registry and 60 (2.2%) in the prospective registry (P<.002). Of note among the most important complications was complete AV block in 10 patients who required the implantation of a pacemaker (2 in AVNRT, 4 in AP, 2 in atrial flutter, and 2 in VT). Eight patients had a transitory or minor AV block and no permanent pacemaker was required. In addition, 13 pericardial effusion or tamponade (1 in AVNRT, 3 in AVN, 3 in atrial flutter, 1 in AF, and 5 in VT), 4 cerebrovascular events (1 in AP, 2 in atrial flutter, and 1 in VT), 13 severe arterial complications (8 in AP, 1 in AVNRT, 1 in atrial flutter, and 3 in VT), 1 suprarenal hemorrhage (AF), and 24 various other complications, generally of a minor entity, were reported. Complications expressed as a percentage per substrate (Figure 6) showed that VT ablation was associated with the highest number of complications (5.6%), followed by AF (2.6%), AP (2%), AVN (1.7%), atrial flutter (1.6%), FAT (1.6%), and AVNRT (0.7%).
Fig. 6. Comparison of complications according to type of substrate between the 3 registries so far published (2001, 2002, and 2003). AVNRT indicates atrioventricular nodal reentry tachycardia; AP, accessory pathways; VT, ventricular tachycardia; AVN, atrioventricular node ablation; FAT, focal atrial tachycardia; AF, atrial fibrillation.
Periprocedure mortality, defined as death during the procedure or within the subsequent 24 hours, was 0.11% (5 patients, all from the prospective registry). Two patients died due to cardiac tamponade, 1 after VT ablation and another after AVN ablation. Two other patients died after ablation for atrial flutter, 1 due to a massive stroke 24 hours after the procedure despite apparently being adequately anticoagulated, and the other patient 6 hours after the procedure due to probable acute pulmonary edema. Finally, 1 patient died after VT ablation for an arrhythmic storm and cardiogenic shock. Three of these patients (the 2 whose substrate was VT and the patient who died because of acute pulmonary edema) had a history of ischemic heart disease with a depressed left ventricular ejection fraction (<35% in 2 cases and from 35%-50% in 1), which probably contributed to the fatal outcome of the procedure.
DISCUSSION
For the third consecutive year, over 80% of all centers performing ablation procedures in Spain participated in the registry, although this year the number was slightly reduced in comparison with previous years.1,2 The consistency of this very representative information was strengthened this year by the quality provided by the collection of prospective data. The simultaneous acquisition of both retrospective and prospective data enabled further comparative analyses between the 2 sets of data.
Comparison With Other Registries
We are unaware of the publication of any other significantly representative registry of ablation procedures since last years' reported registry. Thus, the reports of the Portuguese Society of Cardiology for 20015 and 20026, of the prospective registry of the NASPE7 in 1998, and of the MERFS8 in 1993 still remain valid. Apart from these, the only other important multicenter registry of ablation procedures is that undertaken by the American Society of Pediatric Electrophysiology.9 This registry reported on 481 patients aged 0-16 years who underwent a first ablation procedure for AVNRT or AP from 1999 to 2003. The high success rate, both for ablation for AVNRT (98%) and AP ablation (95%) was clearly superior to our prospective results, especially for AP. As with our registry, the success rate for left free wall AP ablation (97.8%) was significantly higher than that for lesions of the right free wall (90.8%). The rate of AV block, however, was somewhat higher (1.2%), especially for AVNRT (2.1%) and septal AP (3%) ablation. This fact is important to note because the patients were children.
The centers with the highest procedural success rates were those most likely to publish their results.10 Moreover, these centers usually have a higher volume of procedures than the other centers or more advanced and sophisticated devices. This imbalance creates a bias regarding the true practice, which is probably closer to that published in registries such as ours. To this extent, it is worth mentioning the "surprising" data reported for AP ablation in the prospective registry, not only because of the results but also because of the number of complications and the frequency of the need for a second procedure. Comparison of these data with those of the NASPE registry,7 which was also prospective, shows agreement in the relatively important rate of major complications (1.9%), whereas their overall result for AP ablation was superior (94%) to ours. Comparison of our results with those of other large published series of ablation procedures provides no obvious explanation for the lower success rate seen in our prospective registry, although it may be due to selection bias of the centers in the other registries.
Comparison With Previous Registries
Although the quality of the data received allowed all the registries to be studied this year, the total number of ablations and centers was slightly lower than those of previous years (41 centers and 4374 ablations in 2001 or 42 centers and 4970 ablations in 2002). Despite this lower number, the participation this year enabled the information received to be considered fully representative of what happens in all the groups specializing in cardiac electrophysiology in Spain.
By sections, the general information regarding the participating centers has hardly changed, as was to be expected. The characteristics of the laboratory, the personnel working in it and the equipment involved, even the number of navigation systems used, are all very similar to those of last year. The only notable differences were a greater use of intracardiac echocardiography and cryoablation, and the appearance of the new nonfluoroscopic navigation system RPM®.
By substrate, AVNRT was still the most common arrhythmia targeted, with no changes in its high rate of success and low rate of complications and repetitions. Notably, AVNRT was not inducible during 47 procedures (6%) in the prospective registry, which thus makes this one of the largest series to date with this feature.12 The provocation of AV block requiring implantation of a pacemaker fell very slightly, from 0.3% to 0.1% (P=NS).
The success rate of AP-targeted ablations in the 2002 registry was 93%, similar to that of this year in the retrospective registry (91.7%) but far from the result obtained in the prospective registry (87%). Complications this year, however, were significantly more common (2% vs 0.9%; P=.02).
Ablation for atrial flutter has now become consolidated as the third most commonly treated substrate. Somewhat further down the scale were ablations performed for NAV, VT, and FAT, which hardly changed compared with previous years, either in overall percentage or in the result or complication rate; this latter was again headed by ablation for VT, without doubts due to the high prevalence of organic heart disease in this population (65%).
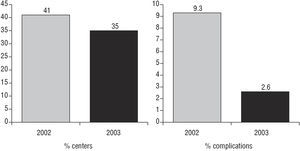
The number of ablations for AF increased slightly compared to last year (10.7% vs 8% of the total), but they were undertaken in a lower number of centers (18 in 2002 [41.8%] vs 14 in 2003 [35.8%]). This concentration of cases in fewer, possibly better prepared centers (Figure 7), as well as progress along the learning curve, could explain the reduction in the number of complications in this type of ablation (9.3% vs 2.6%; P=.05) (Figure 7).
Fig. 7. Percentage of centers which performed ablation for atrial fibrillation in 2002 and 2003 (left) and percentage of complications registered in the treatment of this type of substrate (right).
Comparison of the Prospective and Retrospective Methods
This analysis may well be one of the most notable points in this years' registry. The statistically significant difference in the results and complications between the 2 types of registry reaffirms the quality of the data obtained with the prospective registry. Moreover, the information collected in this type of registr y was much more concrete and much wider. This difference in the result between the 2 types of registry was mainly sustained by the difference in the results of ablation for AP, as mentioned above. The success rates in all the other substrates except AF and AVN were higher in the retrospective registry than the prospective registry, although the differences were not statistically significant (Figure 4). This higher success rate could be partly explained by a possible rounding of the figures in those procedures in which evaluation of the efficacy was difficult immediately after the procedure, as occurs in VT and FAT. Whatever the case, we believe that the lack of a well-defined, homogenous criterion for the efficacy of all the procedures should question the results obtained, which in no case are designed to be either the aim or the main data of this registry. Much more important we believe to be the difference seen in the rate of complications between the 2 types of registry (60 vs 15), although some of the complications can be considered as minor. Complications appearing after the ablation procedure are difficult to register with the procedure itself and may be more easily overlooked in the retrospective registry. Furthermore, to evaluate the true rate of complications, we should remember that our registry lacks an important section concerning information regarding those ablation procedures which were aborted, either due to patient choice (for possible risks) or the choice of the physician (risk/benefit balance), or the appearance of complications before starting the ablation procedure.
In summary, the members of the Working Group on Electrophysiology and Arrhythmias reaffirm their commitment to consolidate an ablation registry with the sufficient quality to act as a reference for the scientific community. Although the changes are still few compared with previous years, catheter ablation has a high rate of efficacy with a low incidence of complications and mortality.
List of Physicians Responsible for Data Management in the Centers Participating in the Spanish Registry of Ablation for 2003
A. Arenal, M.F. Arcocha, A. Barrera, A. Berruezo, A. Bodegas, J. Brugada, E. Castellanos, S. del Castillo, J.J. Esteve, C. Expósito, I. Fernández Lozano, M.L. Fidalgo, H. Fornieles, A. García Alberola, I. García Bolao, D. García Medina, J. Hernández, B. Herreros, M. López Gil, J. Martí, J.G. Martínez, J.L. Martínez Sande, J.L. Merino, A. Moya, J. Osca, A. Pachón, A. Pastor, L. Pérez Álvarez, N. Pérez Castellano, A. Quesada, F.J. Rodríguez Entem, E. Rodríguez Font, G. Rodrigo Trallero, X. Sabaté, L. Tercedor, and P. Torner.
A list is presented at the end of the article with the physicians responsible for data management at each participating center.
Correspondence: Dr. E. Rodríguez Font.
Unidad de Arritmias. Servicio de Cardiología.
Hospital de la Santa Creu i Sant Pau.
Avda. Sant Antoni Maria Claret, 167. 08025 Barcelona. España.
E-mail: erodriguezf@hsp.santpau.es