Keywords
INTRODUCTION
Implantable cardioverter-defibrillators (ICD) have proven efficacy in the primary and secondary prevention of sudden cardiac death (SCD). The results of several published studies have enabled the main indications for ICD use to be compiled in the clinical guidelines for the management of patients with ventricular arrhythmias or at risk of SCD.1,2 However, the increased use of ICD has raised questions concerning their efficacy outside the context of clinical trials, the appropriate selection of patients for ICD implantation, access to treatment, safety, and cost-effectiveness.3 Health registries may prove very useful in providing information on these issues and the application of the clinical guidelines in nonselected patient populations, given the scarce information in the literature.
The present report brings together data on ICD implantation from the Spanish ICD Registry for 2009. This registry was initiated in 1996 by the Electrophysiology and Arrhythmia Section of the Spanish Society of Cardiology (SEC) and subsequently strengthened following the creation of the Working Group on ICD (WGICD) within this section of the SEC, and which has been publishing the data from this registry every year since 2002.4-8
The main objective of the registry is to determine how ICDs are currently used in Spain regarding indications, clinical characteristics of the patients, implantation parameters, types of device and their programming, and procedural complications.
METHODS
The registry data were obtained via a data collection form available at the SEC web page (http://www.secardiologia.es/ images/stories/file/ arritmias/registro-nacional-dai2010.pdf). The form was completed directly and voluntarily by each implantation team in collaboration with staff from the ICD manufacturer, during or after ICD implantation, and was sent by fax or e-mail to the SEC.
The SEC staff input the information into the Spanish ICD Registry database. Data cleaning was performed by a SEC computer specialist and a member of the WGICD. The authors of this article were responsible for data analysis and manuscript preparation.
The population data used to calculate rates per million population for the country as a whole and by autonomous community and province were obtained from the estimates reported for the period up to January 1, 2009 by the Spanish National Institute of Statistics.9
To estimate the representativeness of the registry, we calculated the proportion of implantations and replacement procedures reported in relation to the total number of implantations and replacement procedures performed in Spain in 2008. The total number was based on data provided that year by the device manufacturers to the European Medical Technology Industry Association (EUCOMED).10
In case different medical conditions or clinical arrhythmias were reported for the same patient, only the most severe condition was included for analysis.
The percentages for every variable analyzed were calculated according to the total number of implantations for which information on that variable was available.
Statistical Analysis
The numerical results are expressed as mean ± standard deviation. Continuous quantitative variables were calculated using ANOVA or the Kruskal-Wallis test. Qualitative variables were compared using the χ2 test. The relationship between the number of implantations and implantation centers per million population and between the total number of implantations and the number of implantations for primary prevention in each center were assessed using linear regression analysis. The statistical significance of the trend towards use of ICDs in primary versus secondary prevention was assessed using the Mantel-Haenszel c2 test. A P value of <.05 was used as a cutoff for statistical significance. The statistical analysis was performed using the SPSS statistical software package, version 18.0.
RESULTS
The response rates for different fields in the data collection form ranged from 54.75% (use in primary or secondary prevention) to 99.46% (name of implantation center), although the response rate was in general higher than 80%.
Implantation Centers
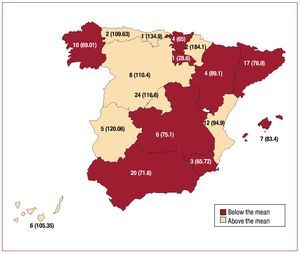
In total, 134 centers performed ICD implantation and provided data to the registry (29 more than in 2008) (Table 1). Of these, 80 were public hospitals (1 more than in 2008). Figure 1 shows the total number of centers and the number of implantations per million population in centers in each autonomous community that provided data to the registry in 2009.
Figure 1. Number of implantation centers (rate per million population) by autonomous community in 2009.
Total Number of Implantations
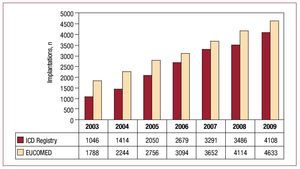
In total, 4108 implantations (first implantations and replacements) were included in the registry for 2009. Based on a total of 4633 implantations performed that year (according to EUCOMED data), this represents 84.7% of all ICD implantations performed in Spain. Figure 2 shows the total number of implantations reported to the registry and estimated by EUCOMED in the last 7 years.
Figure 2. Total number of implantations reported to the registry and estimated by the European Medical Technology Industry Association (EUCOMED) from 2003 to 2009. ICD, implantable cardioverterdefibrillator.
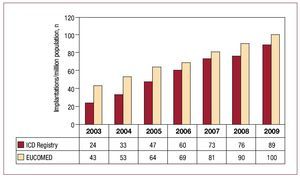
The total number of implantations per million population reported to the registry was 89. The total number of implantations per million population according to EUCOMED data was 100. Figure 3 shows the increase in the number of implantations per million population reported to the registry and that estimated by the EUCOMED for the last 7 years. Table 1 shows the number of implantations reported to the registry by each implantation center. Figure 4 shows the number of implants performed in each autonomous community and reported to the registry in 2009. Table 2 shows the number of implants reported to the registry by the province and autonomous community in which the patient resided and the number per million population. Most of the implantations reported were performed in public hospitals (3866), which represents 94.0% of the reports included in the registry for which data on the implantation center were available.
Figure 3. Total number of implantations per million population reported to the registry and estimated by the European Medical Technology Industry Association (EUCOMED) from 2003 to 2009. ICD indicates implantable cardioverterdefibrillator.
Figure 4. Implantations reported to the registry in 2009 by autonomous community.
First Implantations Versus Replacements
This information was available in 3880 of the forms provided (94.4%). The number of first implantations was 2930, which represents 75.5% of all implantations reported. In total, 63.4 first implantations per million population were reported to the registry. The number of replacements was 950 (24.4%).
Age< and Sex
The mean (standard deviation) (range) age of the patients who underwent first ICD or replacements was 62.19 (13.99) (1-86) years. The mean (SD) was 61.66 (13.57) years at first implantation. Most implantations were performed in men, who accounted for 81.7% of all implantations and 81.8% of first implantations.
Underlying Heart Disease, Left Ventricular Ejection Fraction, Functional Class, and Baseline Rhythms
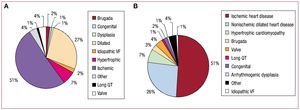
The percentages of patients with different underlying heart diseases were very similar in patients who underwent first implantations and in the group as a whole (Figure 5B). The most common condition was ischemic heart disease, followed by dilated cardiomyopathy, hypertrophic cardiomyopathy, and primary conduction abnormalities (Brugada syndrome, idiopathic ventricular fibrillation, and long QT syndrome). These were followed in frequency by valvular heart disease and arrhythmogenic right ventricular cardiomyopathy.
Figure 5. Heart disease reported to the registry. A, first implantations. B, total implantations. VF, ventricular fibrillation.
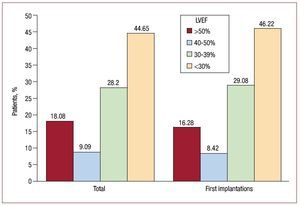
Regarding ventricular systolic function, 46.22% of patients who received a first ICD had a left ventricular ejection fraction (LVEF) <30%. In total, 29.08% had an LVEF between 30% and 39%. The smallest group of patients was formed by those with mild dysfunction, with an LVEF between 40% and 49%. Similar proportions were found for the total number of implantations (Figure 6).
Figure 6. Left ventricular ejection fraction (LVEF) of the patients in the registry (first implantations and total implantations).
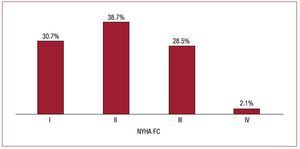
Regarding New York Heart Association functional class (FC), most patients were in FC II (38.7%). These were followed by the groups of patients in FC III and I (28.5% and 30.7%, respectively), whereas there were very few patients in FC IV (Figure 7).
Figure 7. New York Heart Association functional class (NYHA FC) of the patients in the registry.
Regarding baseline rhythm, data on 765 patients was not available. The majority of patients for whom data were available were in sinus rhythm (76.67%), 16.27% had atrial fibrillation, 4.3% had pacemaker rhythm, and the remainder presented other rhythms (atrial flutter or other atrial arrhythmias).
Clinical Arrhythmia Requiring ICD Implantation, Form of Presentation, and Laboratory-Induced Arrhythmia
This information was available in 74.4% of the forms provided. The most common group among patients undergoing first implantation was that of patients without documented clinical arrhythmia (47.6%). These were followed in frequency by those with sustained monomorphic ventricular tachycardia (SMVT) and nonsustained ventricular tachycardia (23.4% and 16.8%, respectively). In the overall implantation group, 41.4% of patients had no documented arrhythmia, whereas the proportion of patients with sustained arrhythmias was greater. The differences in the type of clinical arrhythmia in the first implantation group compared to the overall group were statistically significant (P<.001) (Figure 8).
Figure 8. Clinical arrhythmia in patients in the registry (first implantations and total implantations). Abbreviations: VF/ MVT, ventricular fibrillation/monomorphic ventricular tachycardia; SMVT, sustained monomorphic ventricular tachycardia; NSVT, nonsustained ventricular tachycardia.
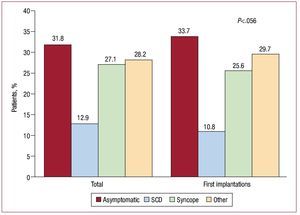
The most common form of clinical presentation, in both the overall group and first implantation group, was a lack of symptoms, followed by syncope and "other symptoms". There were no statistically significant differences (P=.056) in the form of clinical presentation between the first implantation group and the overall group (Figure 9).
Figure 9. Clinical presentation of arrhythmia in patients in the registry (first implantations and total implantations). SCD, sudden cardiac death.
Information on electrophysiological studies was available on 2129 patients undergoing first implantation (72.6%). This was performed in 363 patients (17.05% for which this information was reported). In most cases this was performed in patients with previous infarction or dilated cardiomyopathy and SMVT, and in patients with previous infarction and syncope; SMVT was the most commonly induced arrhythmia (54.62%). Sustained arrhythmia was not induced in 24.6% of cases.
Indications
In 55.9% of first implantations, the indication for ICD was primary prevention. There has been an increasing trend in ICD implantation for primary prevention since the beginning of the second phase of the registry, increasing from 20.7% of the indications reported to the registry in 2003 to 55.9% in 2009. The steady increase in their use for primary prevention and the gradual decrease in their use for secondary prevention between 2003 and 2009 was statistically significant (P<.001) (Table 4). However, between 2008 and 2009 there was a slight decrease that was not statistically significant when the results were compared individually (from 57% to 55.9%; P=.08).
The largest group was formed by patients with ischemic heart disease. In this group, primary prevention accounted for almost half of all indications (49.3%), which was a clear increase compared to the previous year (49.3%). In 31.77% of implantations for primary prevention, ICD implantation involved a device with CRT capability (ICD-CRT).
The next most frequent indication was for primary prevention in patients with dilated cardiomyopathy (69.4% of implantations in patients with this type of heart disease were for primary prevention, which was also more than in 2008 [58.3%]). Of these, 56.2% of the cases involved ICD-CRT implantation.
In patients with hypertrophic cardiomyopathy, Brugada syndrome, long QT syndrome or congenital heart disease, more than 50% of implantations were for primary prevention. On the other hand, in patients with valve disease and arrhythmogenic right ventricular cardiomyopathy, ICD implantation was more commonly performed for secondary prevention.
There was a statistically significant correlation between the total number of first implantations in a center and those performed for primary prevention (r2=0.72; P<.001).
Table 3 shows the changes in indications related to the principal heart diseases during the last 4 years (those with the greatest representation in the registry).
Implantation Center and Specialists
Data on the center and specialist were available for 95.12% and 92.3%, respectively, of the implantations reported to the registry. In total, 67% of implantations were performed in a electrophysiology laboratory and 33% in the operating theater. No implantations were performed elsewhere.
The intervention was performed by electrophysiologists in 72.7% of the cases, by a heart surgeon in 19.57%, and by another specialist in 7.6%.
Generator Position
In most cases, the generator was implanted in a subcutaneous pectoral position (91.2% of all implants and 88.3% of first implants). Submuscular pectoral placement was used in 8.3% of all implants and in 5.6% of first implants. Abdominal placement was used in 3 first implants and 13 replacements (0.1% of first implants and 0.4% of all implants).
Device Type
When all the implants (first implants and replacements) were analyzed, the percentages of single-chamber ICDs, dual-chamber ICDs, and ICD-CRT devices were 52.1%, 21.34%, and 26.52%, respectively. When only primary implants were evaluated, these percentages were 55.6%, 19.1% and 25.2%, respectively. According to the data provided by the EUCOMED, in 2009, the percentages of single-chamber or dual-chamber devices and ICDCRT devices implanted were 69.5% and 30.2%, respectively.
Reasons for Replacements. Substitution of Electrodes in Replacement Generators and Use of Additional Electrodes
Of the reported replacements, information on the reason for replacement was available in 80% of cases. Of these, 85% were due to battery depletion and the remainder were due to complications. In total, 14.6% of the 114 replacements due to complications were performed within the first 6 months following implantation.
In total, 14.1% of the original electrodes were nonfunctioning. Of these, 55.75% were explanted.
Implantable Cardioverter-Defibrillator Programming
The most commonly employed antibradycardia pacing was VVI mode (52.7%). The VVIR mode was used in 9.7% of the cases, DDD mode in 25.16%, DDDR mode in 8.4% and other pacing modes in 3.9% (generally modes aimed at reducing the percentage of ventricular pacing in dual-chamber devices).
The device was programmed for ventricular antitachycardia pacing in 86% of cases and for a combination of ventricular and atrial pacing in 4.4%. Antitachycardia pacing was not programmed in 9.2%.
Both ventricular and atrial defibrillation or cardioversion therapies were programmed in 6.4% of cases.
Complications
Five deaths during implantation were reported (0.12%). In total, 18 complications during implantation were reported: 1 case of tamponade, 4 of pneumothorax and 13 unspecified.
DISCUSSION
The 2009 ICD registry continues to maintain acceptable representativeness (the number of implantations reported increased to 88.6%, compared to the 84% obtained in the previous 4 years). The data provide a good reflection of the current situation regarding the number of implantations, indications, clinical characteristics of the patients, types of device used, programming, and complications, and are a good indicator of daily clinical practice in Spain.
Comparison With Previous Years
When compared to the 2008 registry, a standstill was observed in the number of ICD implantations for primary prevention but without statistically significance differences between the 2 years. Compared to other years, the increase in ICD for primary prevention was maintained. Ischemic heart disease was the most frequent condition, with 56.4% of implantations, followed by dilated cardiomyopathy, which increased from 58.3% in 2008 to 69.4% in 2009, representing more than half of the ICD+TRC implantations for this substrate.
Significant quantitative jumps in primary prevention have occurred in the last 8 years. The first occurred between 2002 and 2003 and was probably related to the publication in 2002 of the Multicenter Automatic Defibrillator Implantation Trial II (MADIT II).11 The second occurred in 2005 and 2006, mainly related to the results of the Comparison of Medical Therapy, Pacing and Defibrillation in Heart Failure (COMPANION)12 and Sudden Cardiac Death in Heart Failure Trial (SCDHeFT) studies.13 The third occurred in 2008, but is not related to the publication of a new trial. Although the results of the Multicenter Automatic Defibrillator Implantation Trial-Cardiac Resynchronization Therapy (MADIT-CRT)14 were known in 2009, we doubt that these would have influenced the increase in the use of cardiac resynchronization, whose effect will probably be more evident in 2010. The total number of implantations in absolute terms and per million population has continued to increase due to the increased number of total implantations. The number of implantations reported increased to 88.6%, whereas this was 84.7% in 2008, in contrast to 90% in 2007 according to EUCOMED data.
The number of centers has continued to increase, with 17 new centers in 2009. However, in 48 centers, the majority of them private, the number of implantations per year was less than 5 and only 47 centers implanted more than 25 defibrillators per year. Their use for primary prevention was more common in centers performing more implantations.
There have been no significant changes in the epidemiological characteristics of the patients, which remained similar regarding age and the predominance of men. Neither were there changes regarding the type heart disease motivating ICD implantation. Patients with severe ventricular dysfunction and FC II-III remained in the majority, although there was a slight increase in FC I compared to 2008.
Regarding the type of device, the proportion of single-chamber ICD, dual-chamber ICD or ICD+TRC remained similar compared to 2008. There was no notable change in programmed pacing mode and antitachycardia pacing functions.
There were no changes in the implantation setting or the percentage of implantations performed by electrophysiologists compared to 2008.
Comparison With Other Countries
EUCOMED data for 2009 include ICD implantations for Austria, Belgium+Luxembourg, the Czech Republic, Denmark, Finland, France, Germany, Greece, Ireland, Italy, the Netherlands, Norway, Portugal, Spain, Sweden, Switzerland and the United Kingdom. The mean number of ICD and ICD+TRC implantations per million population was 234, ranging from 102 in Spain and 413 in Germany. In addition to Germany, above average rates were found for Italy (329), the Netherlands (316), Denmark (269), the Czech Republic (237) and Austria (235). Below average rates were found for Spain (102), Portugal (115), Greece (132) Norway (132), Finland (133), the United Kingdom (139), Sweden (146), France (154), Switzerland (175), Belgium+Luxembourg (187) and Ireland (192). The mean number of ICD+TRC implantations per million was 85. Countries above this mean were Italy (150), Germany (127), the Czech Republic (108), and the Netherlands (108), whereas those below this mean were Finland (30), Spain (32), Norway (34), and Portugal (41). The mean percentage of ICD+TRC compared to total ICD was 27.5%. In Spain the percentage was 30.5%, and ranged between 45.5% in Italy and 22.5% in Finland.
In September of 2008, the second report of the United States National ICD Registry was published, covering the period from April 2006 to June 200815; the implantation rate for 2009 is also known.16 Despite the decrease in the implantation rate in 2009, the number of implantations per million in the United States is more than double the European average.
The implantation rate per million in 2009 in Spain is less than half the European average, and among the countries participating in EUCOMED Spain is currently placed last for single-chamber and dual-chamber implantations and second to last for ICD+TRC implantations.
The enormous variations between continents and between countries sharing the same environment cannot be explained only by differences in income between them; other aspects probably have a far greater influence, such as the type of health care structure and the nature of the culture within the health care community. Italy has similar incomes to those in Spain and also shares the same Mediterranean environment; yet it has one of the highest rates of ICD+TRC implantations in Europe, 150 per million, and holds second place for the total number of implantations performed in European countries. The Italian registry results were published in September 2009.17 The implantation rate for prevention primary was 55.7%, similar to that for Spanish woman. The underlying disease was ischemic heart disease in 37.7%, dilated cardiomyopathy in 35.5%, myocardial hypertrophy in 2.6% and valvular disease in 1.6%. The percentage of patients with ischemic heart disease was lower than in the Spanish and US registries. Regarding pacing mode, there was a greater percentage of ICD+TRC and dual-chamber implantations than in Spain.
Differences Between Autonomous Communities
As in all previous registries, there are large geographical differences in the implantation rate per million in Spain. In 2009, the following communities were above the national average of implantations: Navarre (184), Cantabria (132), Extremadura (120), Madrid (116), Castile and Leon (110), Asturias (109), the Canary Islands (105), and the Community of Valencia (94). The following communities were below the national average: the Region of Murcia (65), the Basque Country (65), Galicia (69), Andalusia (71), Castile-La Mancha (75), Catalonia (76), the Balearic islands (83), and Aragon (89). These large differences are also found in relation to the use of other cardiovascular technologies.18 The Spanish Cardiac Catheterization Hemodynamics Registry19 reports similar variations for coronary intervention.
There are probably many factors involved in these large differences between autonomous communities, not all of which are well understood. One of them is associated with the number of implantation centers. Countries with greater numbers of implantations, such as Italy,17 have twice as many centers as Spain, and although most of the centers have low implantation rates, they have around 50 centers with an average of >50 implantations per year. The results of the Spanish registry for 2009 suggest that there is no statistically significant correlation between the number of centers and the implantation rate per million in each autonomous community (r2=.009; P=.721).
The number of arrhythmia units in each autonomous community, access to them, and overload could explain the variations between them. Other possible causes could differences in clinical presentation and the prevalence of cardiovascular diseases,18 although, against this argument, some communities have a higher than average prevalence of cardiovascular disease that is not associated with higher rates of implantation.
Direct and indirect economic causes could explain the low implantation rate in some communities, although again there is no association with the income level in each community.
The degree of acceptance and adherence to the clinical practice guidelines, especially regarding primary prevention, may explain differences between countries and also between the different Spanish autonomous communities. Data is available on variations between hospitals in ICD implantation in patients with heart failure in the United States.20 ICDs were implanted in 20% of patients, but there was great variation between hospitals (between tertiles of 1% and 35%). The hospitals with the highest numbers of ICD implantations performed a greater number of percutaneous or surgical coronary revascularization procedures, reported more extensive use of beta blockers, had more hospital beds, and had facilities for heart transplantation.
Limitations
The number of implantations reported to the registry constitutes 88.6% of the implantations performed in Spain, according to data provided by EUCOMED. This figure is higher than that reached in the 2008 registry, although it can be considered representative of the true situation in Spain.
The data collection form was not fully completed, and some information, such as the use of ICD for primary or secondary prevention, was only reported in little more than half of the forms received, which may limit the validity of the results.
The low rate of complications referred to above is due to the fact that this information is provided at the time of the implantation procedure, thus underestimating the number of complications, the great majority of which occur subsequently, such as pneumothorax, electrode displacement, heart failure, infection, etc.
Future Prospects for the Spanish ICD Registry
The correct completion of the forms and prospective reporting are a future aim that can be achieved via the Web. In addition, the design should be changed, as well as the questions, to better reflect the true situation.
The Ontario registry,21 and to a lesser extent those of the United States and the United Kingdom,22 include basic information on patient follow-up. Although including basic questions on follow-up (such as mortality or the number of treatments), would involve extra effort, nevertheless such information could prove very useful.
CONCLUSIONS
The 2009 Spanish ICD Registry recorded 88.6% of the ICD implantations performed and the registry is representative of the situation in Spain. The number of implantations continues to increase and is currently 89 per million. The number of implantations for primary prevention has not increased compared to 2008, although there was an increase compared to other years. The implantation rate in Spain continues to be below the mean of countries within the European Union and the difference seems to be increasing. There continue to be striking differences in the implantation rate between the different autonomous communities.
ACKNOWLEDGMENTS
We would like to thank all the health care professionals involved in performing ICD implantations in Spain who have voluntarily and generously reported data to the registry.
We are also grateful to the individuals from the ICD manufacturers (Medtronic, Boston Scientific, St. Jude, Biotronik, and Sorin Group), for their collaboration in the data collection and returning data to the SEC.
We would also like to thank the SEC and, in particular, Gonzalo Justes and José María Naranjo, for their invaluable work to input data and maintain the registry database, without whose collaboration this registry would not have been possible.
ABBREVIATIONS
FC: functional class
ICD: implantable cardioverter-defibrillator
LVEF: left ventricular ejection fraction
WGICD: Working Group on Implantable Cardoverter-Defibrillators
SCD: sudden cardiac death
CRT: cardiac resynchronization therapy
SMVT: sustained monomorphic ventricular tachycardia
Correspondence: Dr. J. Alzueta.
Unidad de Arritmias. Servicio de Cardiología. Hospital Universitario Virgen de la Victoria. Campus de Teatinos, s/n. 29010 Málaga. Spain.
E-mail: jalzueta@telefonica.net