Keywords
INTRODUCTION
This paper reports the findings from the 2008 Spanish Catheter Ablation Registry. The registry is run by the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias and this is the eighth consecutive year that the findings have been published.1-7 The Registry's objectives are primarily to observe and describe the evolution of the interventional treatment of cardiac arrhythmias in Spain, and to provide reliable information about the activities carried out and the resources available in arrhythmia units.
The Registry covers the whole of Spain and data is collected annually. Participation is voluntary, although most of the arrhythmia units in Spain collaborate. This makes it one of very few existing large-scale observational records of catheter ablations.
METHODS
As in previous years, data were collected in one of two ways, prospectively or retrospectively. In the prospective approach, individual patients were included in a standard database provided by the Registry. In the retrospective approach, a standard questionnaire was sent to all interventional electrophysiology laboratories in January 2009. The questionnaire was also available on the website of the Electrophysiology and Arrhythmias Working Group (www.arritmias.org). All data collected were treated anonymously. Even the Registry coordinators were unaware of data provenance, as the Spanish Society of Cardiology secretariat ensured that participating centers could not be identified.
Information on the technical and human resources available in each participating arrhythmia unit was collected, together with data on procedures performed and patient demographic characteristics. As in previous years, data on human resources was only collected for Spanish National Health Service centers, whilst epidemiological data is only presented for centers where data was collected prospectively.
We analyzed the same 10 arrhythmia substrates collected in previous registries: atrioventricular nodal reentrant tachycardia (ANRT), accessory pathway (AP), atrioventricular node ablation, focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia, ventricular tachycardia with postinfarction scarring (VT-AMI), and ventricular tachycardia associated with non-ischemic heart disease. We analyzed several variables which were common to all substrates, including the number of patients and procedures performed, the success rate, type of ablation catheter used, and the number and type of complications suffered in connection with the procedure, including periprocedural death. We also collected a number of variables which were specific to particular substrates, such as the anatomical location of accessory pathways, the location and mechanism of atrial tachycardias, and the type of ventricular tachycardia.
As in previous years, the success rate refers only to status on completion of the procedure (acute success rate). It was not possible to calculate the rate of recurrence because longer term follow-up was not available. Several therapeutic approaches with differing objectives exist for AF and VTAMI substrates, so criteria for success or failure may differ depending on the technique used. Only complications reported during the post-procedure hospital stay were recorded.
Statistical Analysis
Quantitative variables were expressed as mean (standard deviation). Differences between quantitative variables were assessed using Student t test for dependent or independent samples, as appropriate. The c2 and Fisher exact test were used to analyze differences between categorical variables. A P value less than .05 was considered statistically significant. Statistical analysis was performed using SPSS 15.0.
RESULTS
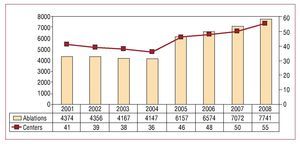
As in previous years, the number of participating centers exceeded that of earlier Registries, with a total of 55 centers submitting data in 2008 (Figure 1). Most of the participating centers were public health system hospitals (84%), with only 9 (16%) being private health care centers.
Figure 1.Change in the number of centers participating and procedures recorded in the Spanish Catheter Ablation Registry.
Again as in previous years, most of the participating centers were tertiary level hospitals (89%) with the cardiology department reporting in 96% of the centers. Three-quarters of the hospitals were university hospitals that provide cardiac surgery (Table 1).
The retrospective data collection method was preferred by most centers, with only 8 centers (15%) sending prospective data.
Epidemiological Characteristics
As in past registries, patient epidemiological characteristics were only analyzed for data sent prospectively. The 8 centers that used this method included a total of 1197 patients.
Patient mean age was 47 (15) years. The youngest patients were those with an AP (38 [12] years) and the oldest were those who underwent atrioventricular node ablation (75 [11] years). With regard to distribution of substrates by gender, ANRT ablation was performed primarily in women (75%), whereas AF ablation and ventricular tachycardias (whether associated or not with structural heart disease) were mainly performed in men (80% and 75%, respectively). As shown, these data are virtually identical to those from the previous registry.
In total, 23% of patients had a history of structural heart disease and left ventricular dysfunction was limited to patients undergoing atrioventricular node ablation and ventricular tachycardia associated with heart disease. The same distribution was observed with respect to patients who received an implantable cardioverter defibrillator.
Infrastructure and Resources
Tables 1 and 2 detail the technical and human resources available in the laboratories participating in the Registry as well as their activities over the year in question.
A total of 42 sites (76%) had at least one dedicated electrophysiology laboratory, although only 42% of those were available 7 days a week (mean days available, 3.6 [1.4]; median, 4). Four centers (7%) had 2 dedicated electrophysiology laboratories. Defibrillators and pacemakers were implanted in 67% of the laboratories. External electric cardioversion was performed in 33 laboratories (60%) and internal cardioversion in 10.
Digital radiology was available at 36 sites (66%) and 51% of the laboratories had a portable fluoroscope. In 42 centers (76%), a nonfluoroscopic navigation system was available, and 16 and 3 centers had 2 and 3 non-fluoroscopic navigation systems, respectively. The proportion of laboratories with intracardiac echocardiography continued to increase (26% in this registry), as did the number of centers with a magnetic navigation system (from 1 to 3). Cryoablation was performed in 17 centers (31%) and none of the centers had ultrasound ablation.
The number of health care staff in electrophysiology laboratories remained largely unchange with 93% of centers having more than one full-time physician. A total of 14 centers (30%) had more than 2 clinicians and 93% of the laboratories had at least 2 full-time university nursing graduates.
Overall Results
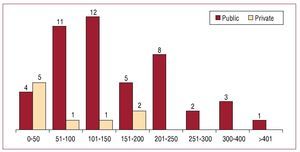
This year saw the highest number of ablation procedures recorded in the Registry's history, with a total of 7741 procedures reported by the 55 participating centers (Figures 1 and 2). This represents a mean of 141 (97) (median, 120; range, 24-503) ablations per center.
Figure 2.Number of electrophysiology laboratories in the National Registry by number of ablation procedures performed during 2008.
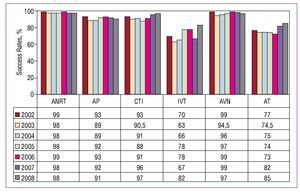
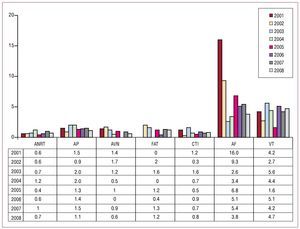
If we exclude AF and VT-AMI, the overall success rate was 93% (6215/6694). A total of 115 complications (1.7%) were reported for all ablation procedures (including AF and VT-AMI). There were 2 deaths (0.03%), one (due to cardiac tamponade) during a MAT ablation and the other after discharge from a FAT ablation. In the latter case, autopsy was unable to establish cause of death, making the relationship with the ablation uncertain. There was one case of pulmonary embolism, which occurred in relation to an ANRT ablation and one case of entrapment of the ablation catheter in a mechanical mitral prosthesis. The latter occurred during a VT-AMI ablation, though information on whether the complication was successfully resolved was not available. Figures 3 and 4 show the success and complication rates in comparison to previous years.
Figure 3.Change in catheter ablation success rates since 2002, by substrate treated. ANRT indicates atrioventricular nodal reentrant tachycardia; AP, accessory pathways; AT, atrial tachycardia; AVN, atrioventricular node; CTI, cavotricuspid isthmus; IVT, idiopathic ventricular tachycardia.
Figure. 4.Percentage of major complications of catheter ablation since 2002, by substrate treated. AF indicates atrial fibrillation; ANRT, atrioventricular nodal reentrant tachycardia; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; VT, ventricular tachycardia.
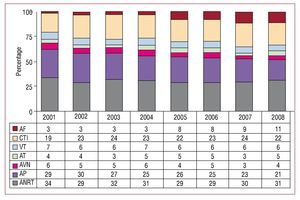
In terms of the frequency of conditions and procedures, ANRT was still the most common with ablation of CTI the second most common procedure, ahead of AP (Figure 5). The percentage of AF ablation procedures also increased and accounted for 10.6% of the total procedures performed. The evolution of the relative frequency of different substrates from 2001 is shown in Figure 6.
Figure 5.Relative frequency of different substrates treated by catheter ablation in Spain during 2008. For each substrate, the percent change from the previous record is shown. AF indicates atrial fibrillation; ANRT, atrioventricular nodal reentrant tachycardia; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia / atypical atrial flutter; VT-AMI, ventricular tachycardia with postinfarction scarring; VT-HD, ventricular tachycardia associated with heart disease.
Figure 6. Change in the relative frequency of the different substrates treated since 2001. AF indicates atrial fibrillation; AT, atrial tachycardia; AVN, atrioventricular node; ANRT, atrioventricular nodal reentrant tachycardia; AP, accessory pathways; CTI, cavotricuspid isthmus; VT, ventricular tachycardia.
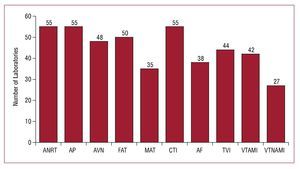
As in the previous Registry, ANRT, AP, and CTI ablations were performed at all sites (Figure 7). The substrate treated in the lowest percentage of sites was ventricular tachycardia not associated with ischemic heart disease (45%). The proportion of centers performing AF ablation increased slightly to 62% (n=34).
Figure 7. Number of electrophysiology laboratories in the National Registry treating each of the different substrates. AF indicates atrial fibrillation; ANRT, atrioventricular nodal reentrant tachycardia; AP, accessory pathways; AVN, atrioventricular node; CTI, cavotricuspid isthmus; FAT, focal atrial tachycardia; IVT, idiopathic ventricular tachycardia; MAT, macroreentrant atrial tachycardia; VT-AMI, ventricular tachycardia with postinfarction scar; VT-C, ventricular tachycardia associated with heart disease; VT-NIHD, ventricular tachycardia associated with nonischemic heart disease.
The following describes the data analyzed according to specific arrhythmias.
Atrioventricular Nodal Reentrant Tachycardia
This substrate was addressed in all centers. A total of 2302 ANRT ablation procedures were performed, with a mean of 42 (28) (range, 6-137) procedures per center. The success rate was 98% (2250/2302); 31 centers (56%) achieved a 100% success rate. There were 15 cases of major complications (0.65%): eight cases (0.35%) of atrioventricular (AV) block (AV) requiring a permanent pacemaker, 6 cases of vascular access complication, and 1 case of pulmonary thromboembolism.
A non-conventional catheter (ie, a catheter other than a radiofrequency catheter with a 4 mm tip) was used in a slightly higher proportion of procedures compared to the previous Registry (4%, or 91 cases, compared to 1.6% last year). This was mostly at the expense of cryoablation catheters. A total of 59 cryoablation catheters were used, 12 with an 8 mm tip, and 20 with an irrigated tip.
Cavotricuspid Isthmus
For the second consecutive year, CTI ablation was the second most common procedure after ANRT ablation. In total, 1720 CTI ablations were performe, giving a mean per center of 31 (26). The procedure was successful in 1660 cases (96.5%). A total of 29 centers reported a 100% success rate for the procedure. There were 13 major complications (0.8%): seven vascular complications, 2 cases of AV block that required implantation of a permanent pacemaker, 3 cases of pericardial effusion, and 1 stroke.
Non-conventional catheters were used in 1582 (92%) procedures: in 915 cases, catheters with an 8 mm tip were used, in 663 cases, an irrigated tip was used, and cryoablation was used in 4 cases.
Accessory Pathways
A total of 1658 accessory pathway ablation procedures were performed (mean, 30 [21]; range, 3-104). The procedure was successful in 1510 (91%) cases; only 8 of the 44 centers which performed over 10 AP ablation procedures in 2008 reported a 100% success rate. There were 18 (1.1%) major complications: 10 vascular complications, 6 pericardial effusions, and 2 strokes. This year there were no deaths or cases of AV block during the AP ablations.
A non-conventional catheter was used in 114 cases (6.9%): in 46 cases, an irrigated tip was used, in 56 cases a cryoablation catheter, and in 12 cases, an 8 mm tip.
The location of the ablated AP was reported in 1461 cases. As in previous registries, the most common sites were the left ventricular free wall (51%) and the inferior paraseptal pathway (28%). This year, again, more ablations were performed in right free wall pathways (12%) than in peri-Hisian or superior paraseptal pathways (9%). The success of the ablation procedure depended on the location of the AP: the success rate was 94.5% (702/743) for ablations in the left free wall, 86% (147/171) in the right free wall, 88% (357/406) in the inferior paraseptal pathway, and 80% (113/141) in peri-Hisian or superior paraseptal pathways.
Atrioventricular Node Ablation
The total number of procedures performed was 334, distributed over 47 centers. The mean per center was higher than in previous years (7 [8]). Success was achieved in 97% of procedures and there were only 2 complications (0.6%), 1 in a vascular access and 1 episode of congestive heart failure. Non-conventional catheters were used in 41 procedures: these were 38 catheters with an 8 mm tip and 3 with an irrigated tip.
Focal Atrial Tachycardia
A total of 254 FAT ablations were performed. The intervention was performed in the right atrium in 43 centers, and in the left atrium in only 21 centers.
The success rate was 84.6% (215/254). The origin of the FAT was reported in 196 cases; success rates were slightly higher for those arrhythmias originating in the right atrium, at 82% (115/141) compared to 78% in the left atrium (43/55). There were a total of 3 complications (1.2%): 1 related to vascular access, 1 AV block that required a permanent pacemaker, and 1 pericardial effusion.
A non-conventional catheter was used in 36 cases: twelve catheters with 8 mm tips, 8 cryoablation catheters, and 16 catheters with irrigated tips.
Macroreentrant Atrial Tachycardia / Atypical Atrial Flutter
This substrate was addressed in 31 centers (56%), with a total of 144 procedures (mean, 4.6 [range, 1-25] procedures per center). The procedure was successful in 102 cases (70.8%). There were 5 complications (3.4%): 1 stroke, 1 femoral pseudoaneurysm, and 3 cardiac tamponade. A patient with complex cyanotic congenital heart disease died after a subsequent tamponade and cardiogenic shock.
In 137 procedures, information on the origin of the MAT was available: 63 procedures were performed in the right atrium compared to 74 in left atrium, with success rates of 79% and 64%, respectively. In 61% of procedures, a catheter tip other than 4 mm was used, mostly irrigated tips.
Atrial Fibrillation
A total of 829 (range, 1-102) AF ablation procedures were performed in 34 of the participating hospitals (62%). This represents a mean of 24 procedures per center, although 13 laboratories performed fewer than 10 procedures.
The technique used was indicated in 610 procedures (73.5%). This was a disconnect with ostial electrical isolation in 34% of cases, off-target circumferential isolation in 56%, and isolation with circumferential reduction potential in the remaining 10%. In 19 procedures, the superior vena cava was also electrically disconnected. The acute success rate was over 90% in all cases, though the actual figure depended on the technique used.
In 85% of these procedures, an irrigated tip was used, in 14.5% an 8 mm tip, and in 0.5% cryoablation was used.
A total of 32 complications (3.8%) were reported: significant pericardial effusion / cardiac tamponade (15), acute coronary syndrome (1), vascular access (7), acute heart failure (2), and stroke (7, although 2 were transient).
Idiopathic Ventricular Tachycardia
A total of 186 ablation procedures for idiopathic ventricular tachycardia were reported from 42 centers (mean, 4.4 [1-16] ablations per site). Success was achieved in 153 procedures (82.2%) and only 4 complications (2%) occurred: 1 tamponade, 1 stroke, 1 complete AV block, and 1 femoral pseudoaneurysm.
The type of VT was known in 153 procedures: 97 occurred in the right ventricle outflow tract, 22 in the left ventricle outflow tract, 19 were fascicular, and 15 were reported as occurring in "another location." Success rates were 75%, 81%, 100%, and 73%, respectively.
In most cases, the ablation catheter tip used was 4 mm.
Ventricular Tachycardia With Post-Infarction Scarring
A total of 40 (73%) centers performed 221 VTAMI ablation procedures (4 [1-38] ablations per site). Complications (n=14, 6.3%) were vascular access (5), cardiac tamponade (5), stroke (1), acute heart failure (1), complete AV block (1), and catheter entrapment in a mitral mechanical prosthesis (1).
The type of ablation was reported in 195 cases: 72 used a "conventional" approach and 123 were substrate specific. In 118 cases, a non-standard catheter tip was used: in 22 cases an 8 mm tip was used and in 96 cases, an irrigated tip.
The success rate reported using the conventional approach (non-inducibility of clinical tachycardia after ablation) was 69.4%. An epicardial approach was used on the VT in 2 cases, without success.
Ventricular Tachycardia Not Associated With Post-Infarction Scarring
Ninety-six ablation procedures were performed for this condition, in 25 laboratories (45%). There was 1 complication: complete AV block.
Success was achieved in 55% of procedures. Types of tachycardia ablated were 16 arrhythmogenic right ventricular dysplasia, 10 branch-branch, 19 with non-ischemic dilated cardiomyopathy, and 6 reported as "other." Success rates were 62%, 100%, 42%, and 33%, respectively.
In 24% of the procedures, a non-standard catheter was used: in 3 cases, an 8 mm catheter tip was used and in 20 cases an irrigated catheter tip was used.
DISCUSSION
As in previous years, 2008 has seen a steady increase in activity in arrhythmia units in Spain. The record participation in this year's Registry, both in terms of the number of participating hospitals (55) and the number of procedures performed (the figure of 7500 procedures was exceeded for the first time), ensures the representativity of the data obtained. However, approximately 10% of the centers only reported the number of procedures performed, without specifying success rates, complications, type of catheter used, or substrate characteristics. Although arrhythmia units are considerably overburdened, the contribution of these data would further increase the Registry's representativeness and reliability.
The increase in the number of ablations this year once again contrasts with the only slight increase in human and technical resources. In 2008, electrophysiology laboratories had virtually the same number of physicians (2.5 [0.7]) as in 2001, when the first Spanish Registry of Catheter Ablation was performed (2.2 [0.6]). This is despite a significant increase in the number and complexity of procedures performed. Furthermore, it should be borne in mind that a significant number of arrhythmia units implant defibrillators or pacemakers, with the additional overload in work which that entails.
In terms of the distribution of substrates in this Registry, 2 aspects warrant mention. On the one hand, the "reinforcement" of CTI ablation as the second substrate addressed, and the stability of the figures for the 3 very common substrates of ANRT, CTI, and AP. On the other hand, the increase in complex arrhythmic conditions treated is also notable. These include ablations for AF, MAT and VT associated with heart disease, which are normally performed with the help of non-fluoroscopic navigation. This year saw more than 800 AF ablation procedures performed, with lower complication rates than in recent years, and the condition represented more than 10% of the total for the first time. Moreover, the published acute success rate, which probably overestimates long-term success rates, was over 90%, indicating that AF ablation is becoming an increasingly safe and effective procedure which is also constantly evolving.8,9 There was also a notable increase in the number of MAT, VT associated with non-ischemic heart disease, and VT ischemic ablation procedures performed, a fact which was probably helped by the regular introduction of navigation systems in daily practice. With respect to the previous year, the increase was 18% for AF, 78% for the MAT, 40% for VT associated with non-ischemic heart disease, and 41% for ischemic substrate ablation. It is also significant, and perhaps surprising, to note the significant increase over previous years in AV node ablation (42% more than in 2007), when ablations of complex arrhythmic substrates are increasing so rapidly. This is likely in part due to a significant number of resynchronization implants in patients with AF, the failure of previous ablation procedures on substrates such as MAT and AF and, finally, the increasing prevalence of AF in elderly patients.
CONCLUSIONS
The National 2008 Registry of Catheter Ablation, as in previous years, includes one of the largest samples published to date in the international literature on ablation procedures, and noticeably exceeds the 7000 ablations performed the year before. The high participation rate, with the collaboration of 55 electrophysiology laboratories, makes the data obtained on the activity and the results of this procedure in Spain extremely reliable. The success rate of ablation procedures in Spain remains high (93%) with low levels of major complications (1.7%) and mortality (0.03%). Ablation of complex arrhythmic substrates, including atrial fibrillation, increased significantly with regard to previous years. For the second consecutive year, CTI ablation for the treatment of typical atrial flutter was the second most frequently treated arrhythmic substrate after ANRT, though there was also a dramatic increase in the number of cases of AV node ablation.
ACKNOWLEDGMENTS
The Registry coordinators would once again like to express their appreciation to all those who participated in the 2008 Ablation Registry, and who voluntarily and selflessly sent data on their procedures. They also thank Cristina Plaza for her excellent and tireless administrative work.
ELECTROPHYSIOLOGY LABORATORY BY AUTONOMOUS COMMUNITIES AND PROVINCES WHO PARTICIPATED IN THE 2008 NATIONAL CATHETER ABLATION REGISTRY (IN PARENTHESES, THE DOCTOR RESPONSIBLE FOR THE REGISTRY)
Andalucía. Cádiz: Hospital Puerta del Mar (Dr. L. Cano); Córdoba: Hospital Reina Sofía (Dr. J. Segura); Granada: Hospital Virgen de las Nieves (Dr. M. Álvarez); Huelva: Hospital Juan Ramón Jiménez (Dr. P. Moriña); Málaga: Hospital Clínico de Málaga (Dr. J. Alzueta); Sevilla: Hospital Virgen Macarena (Dr. E. Díaz-Infante), Hospital Virgen del Rocío (Dr. A. Pedrote), Hospital Virgen de Valme (Dra. D. García Medina).
Aragón. Zaragoza: Hospital Lozano Blesa (Dr. G. Rodrigo), Hospital Miguel Servet (Dr. A. Asso), Clínica Quirón (Dr. A. Asso).
Asturias. Hospital Central de Asturias (Dr. N. Pachón).
Baleares. Mallorca: Policlínica Miramar (Dr. N. Alvarenga), Hospital Son Llàtzer (Dr. X. Fosch), Clínica Palma Planas (Dr. N. Alvarenga), Clínica Rotger (Dr. X. Viñolas).
Canarias. Hospital Nuestra Señora de la Candelaria (Dr. R. Romero), Hospital Dr. Negrín (Dra. E. Arbelo), Hospital Universitario de Canarias (Dr. A. Rodríguez), Hospital Insular (Dr. F. Segura).
Cantabria. Hospital Marqués de Valdecilla (Dr. F.J. Rodríguez).
Castilla-La Mancha. Toledo: Hospital Virgen de la Salud (Dr. E. Castellanos), Hospital Nuestra Sra. del Prado (Dr. Lacorte).
Castilla y León. Burgos: Hospital General Yagüe (Dr. J. García); León: Hospital de León (Dra. M.L. Fidalgo); Salamanca: Hospital Clínico Universitario (Dr. J.L. Moríñigo); Valladolid: Hospital Río Hortega (Dr. B. Herreros).
Cataluña. Barcelona: Hospital de Bellvitge (Dr. X. Sa baté), Hospital del Mar (Dr. J. Martí), Hospital Clínic (Dr. L. Mont), Hospital Vall d'Hebron (Dr. A. Moya), Hospital de la Santa Creu y Sant Pau (Dr. E. Rodríguez Font), Hospital Mútua de Terrassa (Dr. X. Viñolas), Centro Cardiovascular Sant Jordi (Dr. L. Mont), Clínica Sagrada Família (Dr. A. Moya).
Comunidad Valenciana. Alicante: Hospital Universitario de Alicante (Dr. J.G. Martínez); Valencia: Hospital Clínico (Dr. A. Martínez).
Extremadura. Badajoz: Hospital Infanta Cristina (Dr. M. Doblado).
Galicia. La Coruña: Hospital Juan Canalejo (Dra. L. Pérez).
Madrid. Hospital Ramón y Cajal (Dr. R. Matía); Clínica Puerta de Hierro (Dr. I. Fernández Lozano), Hospital 12 de Octubre (Dr. R. Salguero), Hospital Clínico San Carlos (Dr. N. Pérez Castellano), Hospital Gregorio Marañón (Dr. J. Almendral), Hospital de Getafe (Dr. A. Pastor), Hospital Severo Ochoa (Dr. A. Grande), Hospital La Paz (Dr. J.L. Merino), Clínica USP San Camilo (Dr. J.L. Merino), Grupo Hospitales de Madrid (Dr. J. Almendral).
Murcia. Hospital Virgen de la Arrixaca (Dr. A. García Alberola).
Navarra. Clínica Universitaria de Navarra (Dr. A. Macías), Hospital de Navarra (Dra. N. Basterra).
País Vasco. Vizcaya: Hospital de Cruces (Dr. A. Bodegas), Hospital de Basurto (Dra. M.F. Arcocha); Álava: Hospital de Txagorritxu (Dr. J. Pindado).
ABBREVIATIONS
AF: atrial fibrillation
ANRT: atrioventricular nodal reentrant tachycardia
AP: accessory pathway
AV: atrioventricular
CTI: cavotricuspid isthmus
FAT: focal atrial tachycardia
MAT: macroreentrant atrial tachycardia
VT-AMI: ventricular tachycardia with postinfarction scar
VT-NAMI: ventricular tachycardia associated with heart disease without postinfarction scar
A list of centers and clinicians participating in the Spanish Catheter Ablation Registry is provided at the end of the article.
Correspondence: Dr. I. García-Bolao.
Irunlarrea, 13, 8.o-D. 31008 Pamplona. Navarra. España.
E-mail: igarciab@unav.es