Keywords
INTRODUCTION
This article details the findings of the Spanish Catheter Ablation Registry--the official registry of the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias--corresponding to the year 2006. This is the sixth year of continuous activity.1-5
As in previous years, the working group on electrophysiology and arrhythmias, the sponsor of the registry, is responsible for the organization and quality assurance, and for ensuring that the goals of one of its main activities is met. These goals are basically to observe and describe changes in interventional treatment of cardiac arrhythmias and to provide reliable information on the type of activity and the facilities of our catheterization laboratories.
As in previous years, most of the catheterization laboratories in Spain have participated voluntarily in this registry. The results presented can therefore be considered as very representative of catheterization activity in Spain during 2006.
METHODS
Two different data collection systems were used. One was retrospective, and used a questionnaire which was sent to all catheterization laboratories in January 2006. The completed questionnaire was returned to the secretariat of the working group. Subsequently, these forms were forwarded to the coordinators of the registry, ensuring the identity of the laboratory was kept anonymous. The other system of data collection was prospective, by means of a standard database that required patient data to be entered individually. Both data collection methods were similar to those used in previous registries.
The arrhythmogenic substrates analyzed are listed below using the same nomenclature and abbreviations as in previous publications: atrioventricular nodal reentry tachycardia (AVNRT), accessory pathways (AP), atrioventricular node (AVN), focal atrial tachycardia (FAT), cavotricuspid isthmus (CTI), macroreentrant atrial tachycardia (MAT), atrial fibrillation (AF), idiopathic ventricular tachycardia (IVT), ventricular tachycardia related to postmyocardial infarction scarring (VT-AMI), and ventricular tachycardia associated with heart disease and not related to postmyocardial infarction scarring (VT-NAMI). In general, variables common to all substrates and other substrate-specific variables were analyzed. The general variables included number of patients treated and procedures performed, outcomes, type of ablation catheter used, and the number and type of procedural complications. Among the specific variables, of note were the AP location, the type of ventricular tachycardia, and the location and type of atrial tachycardias.
Atrial fibrillation and VT-AMI deserve special mention, as treatment of such arrhythmias may vary according to the catheterization laboratory where the procedure was performed. With regard to AF, there are several different technical approaches with very different goals,6 from segmental pulmonary vein ablation (with or without electrical isolation) to circumferential ablation to eliminate potentials (with or without ablation lines in the posterior wall and mitral isthmus), as well as complex or fragmented electrocardiogram-guided ablation. In addition, some groups systematically isolate the superior vena cava, the coronary sinus, and the left atrial appendage. In general, all approaches use nonfluoroscopic mapping systems (NFMS); in some cases it is a great help and in others essential.
There are also a range of approaches possible in VT-AMI ablation. The procedure can be performed during tachycardia or in sinus (or basal) rhythm of the patient with or without guidance with an NFMS. The data collection form includes 2 options--the "traditional" approach with guidance among others, and the substrate-based approach aimed at identifying possible slow conduction pathways of the tachycardia circuit susceptible to ablation. The latter of these techniques allows ablation of ventricular tachycardias in patients with poor hemodynamic tolerance or those in whom tachycardia cannot be induced.7
The data on outcomes, presented below, are those obtained at the end of the procedure, and therefore lack subsequent clinical follow-up to analyze possible recurrence. The complications reported correspond to the period lasting until discharge from hospital. In line with the approach of previous coordinators, and for reasons already discussed, data for success rates for AF and VT-AMI substrates are not analyzed.
Also in line with previous registries, the data presented on human resources correspond exclusively to hospitals in the public sector. Finally, due to the characteristics of the data collection procedure, only epidemiological variables corresponding to centers that chose prospective data collection are presented.
Statistical Analysis
Quantitative variables were expressed as means (SD). Differences between different quantitative variables were assessed using the t test for dependent or independent samples as applicable. The χ2 test and the Fisher exact test were used to analyze possible differences between categorical variables. Statistical analysis of data was carried out with the SPSS statistical package, version 13.0. Statistical significance was established at P<.05.
RESULTS
In total, data were returned from 48 centers--corresponding to a larger number of participating centers compared to previous registries. Of these centers, 43 (89.5%) belonged to the public health sector and 5 (10.5%) to the private sector. One hospital treated exclusively pediatric patients. Compared to the previous year, 6 new centers participated in the registry (4 in the public sector and 2 in the private sector), whereas 4 centers stopped returning data (3 public ones and 1 private one).
One center started its activity at the end of the year and sent data for 6 procedures. The results and complications considered in this publication therefore correspond to 47 centers.
The total number of centers that returned retrospective data was 40 (83.3%), the 8 remaining centers did so prospectively.
With regard to the characteristics of the participating hospitals--very similar to previous years--it is noteworthy that the majority (approximately 90%) were tertiary hospitals and the cardiology service was responsible for sending the data. Three quarters of these hospitals were university hospitals and had heart surgery facilities.
Epidemiological Characteristics
Although epidemiological data were gathered exclusively from the 8 centers that returned prospective data, the acceptable sample size (1157 patients) and the similarity of these data with those from previous years meant that they were fairly representative.
The mean age of the patients was 53 (20) years; the youngest group was diagnosed with AP (37 [18] years) and the oldest underwent AVN ablation (71 [11] years). With regard to the sex distribution, AVNRT ablation was performed mainly in women (74%), whereas more men underwent AF ablation (84%) and ventricular tachycardia (70%) whether or not related to structural heart disease.
Although a history of structural heart disease was reported in 22% of the patients, left ventricular dysfunction, except in exceptional cases, was limited to patients undergoing AVN ablation and those with ventricular tachycardias related to heart disease. As was to be expected, the same distribution was found for patients who had an implantable cardioverter-defibrillator.
Composition and Operation of the Laboratories
Tables 1 and 2 present the data on the technical and human resources of the catheterization laboratories participating in the registry. Also presented are data on the availability of the laboratory and activities undertaken.
As data worth highlighting, 55% of the laboratories had digital radiology, 78% were dedicated full-time to ablation, and 71% of the laboratories also implant pacemakers and implantable cardioverter-defibrillators. Overall, 68.8% (31/45) of the catheterization laboratories were equipped with an NFMS, and 9 and 4 laboratories had 2 and 3 systems, respectively. Ten of these laboratories also had intracardiac ultrasound and 11 had cryoablation facilities.
The distribution of the personnel in the catheterization laboratories was very similar to that of previous years, with a full-time physician employed in the laboratories of 71% of the hospitals.
Overall Results
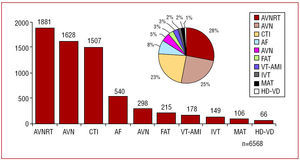
The total number of ablation procedures reported by a total of 47 laboratories, excluding the center with 6 ablations, was 6568 (Figure 1). This figure corresponded to a mean of 139 (75) ablation procedures per center (median, 124.5; range, 27-421).
Figure 1. Number of catheterization laboratories included in the Spanish Registry by number of ablation procedures carried out in 2006.
The overall percentage of successful outcomes was 92.27%, excluding AF and VT-AMI ablation.
A total of 92 complications were reported (including those arising from AF and VT-AMI ablation), corresponding to 1.4%. Only 1 patient--with known ischemic heart disease--died (0.015%) after AP ablation. The event was apparently related to acute myocardial infarction.
The arrhythmias most frequently treated were, in descending order, AVNRT, AP, and CTI (Figure 2). These results are the same as in previous years, as are the relative percentages with respect to the total for a given type of arrhythmia (Figure 3). AF ablation, as in 2005, remained at 8%.
Figure 2. Relative frequency of the different substrates treated by catheter ablation in Spain during 2006. AF indicates atrial fibrillation; CTI, cavotricuspid isthmus; AVN, atrioventricular node; FAT, focal atrial tachycardia; MAT-AFL, macroreentrant atrial tachycardia-atypical atrial flutter; AVNRT, atrioventricular nodal reentry tachycardia; VT-HD, ventricular tachycardia related to heart disease; IVT, idiopathic ventricular tachycardia; VT-AMI, ventricular tachycardia related to post-myocardial infarction scarring; AP, accessory pathways.
Figure 3. Relative frequency of different substrates treated since 2001. AF indicates atrial fibrillation; CTI, cavotricuspid isthmus; AVN, atrioventricular node; AT, atrial tachycardia; AVNRT, atrioventricular nodal reentry tachycardia; VT, ventricular tachycardia; AP, accessory pathways.
All centers did AVNRT, AP and CTI ablation (Figure 4), with a slight increase in the percentage of laboratories that treated AF and VT related to heart disease.
Figure 4. Number of catheterization laboratories included in the Spanish registry that treat the indicated substrates. AF indicates atrial fibrillation; CTI, cavotricuspid isthmus; AVN, atrioventricular node; FAT, focal atrial tachycardia; MAT, macroreentrant atrial tachycardia; AVNRT, atrioventricular nodal reentry tachycardia; VT-HD, ventricular tachycardia related to heart disease; IVT, idiopathic ventricular tachycardia; VT-AMI, ventricular tachycardia related to post-myocardial infarction scarring; AP, accessory pathways.
The overall results, both for success rates and complications, are shown in comparison with previous years in Figures 5 and 6.
Figure 5. Change in percentage of successful catheter ablation procedures by substrate since 2002. CTI indicates cavotricuspid isthmus; AVN, atrioventricular node; AT, atrial tachycardia; AVNRT, atrioventricular nodal reentry tachycardia; IVT, idiopathic ventricular tachycardia; AP, accessory pathways.
Figure 6. Percentage of major complications during catheter ablation procedures by substrate treated since 2002. AF indicates atrial fibrillation; CTI, cavotricuspid isthmus; AVN, atrioventricular node; FAT, focal atrial tachycardia; AVNRT, atrioventricular nodal reentry tachycardia; VT, ventricular tachycardia; AP, accessory pathways.
We will now discuss the data analyzed by specific arrhythmogenic substrate.
Atrioventricular Nodal Reentry Tachycardia
This substrate was treated in all centers, including the pediatric one. In total, 1881 ablation procedures were performed, with a mean per center of 38 (20) (range, 7-117). Of these 1851 were successful (98.4%) and 31 centers (66%) reported success in all procedures performed. In all, there were 12 (0.7%) major complications: 8 (0.4%) corresponded to AV block that needed definitive pacemaker placement, 2 to vascular access complications, 1 to stroke, and 1 to pericardial effusion. No deaths were reported related to the procedure. In 28 cases (1.5%), a standard ablation catheter (4-mm tip radiofrequency catheter) was not used. These nonstandard catheters were 27 cryoablation catheters and 1 8-mm tip catheter.
Accessory Pathways
In 2006, 1628 ablation procedures were undertaken. The outcome was reported in 1552 procedures, with success achieved in 1387 cases (92.3%). There were 22 cases of major complications, with 11 (0.68%) vascular complications, 6 AV blocks requiring definitive pacemaker placement, and 4 significant pericardial effusions. One patient (0.06%) died due to a myocardial infarction related to the procedure. A nonstandard catheter was used in 144 cases. The nonstandard catheters used were as follows: 24 8-mm tip catheters, 65 irrigated-tip catheters, and 55 cryoablation catheters.
As in previous registries, AP of the left ventricular free wall was the most common type of arrhythmia treated (48%), followed by inferior septal ablation (24%), ablation of the region around the His bundle and superior septum (15%), and right free wall ablation (13%). The success of the procedure depended on the site of the AP, thus 93% of free left wall ablation, 85% inferior septal ablation, and 93% of free right wall ablation, and 84% of the His bundle and superior septum ablation procedures were successful.
Atrioventricular Node Ablation
In total, 298 procedures were undertaken in 43 centers, and the mean number per center reported in 2005 was maintained (mean, 6 [5]; median, 4; range, 1-22). Success was obtained in 289 (99%) of the 290 procedures and no complication was reported. There were 37 cases in which a special catheter was used: 33 8-mm tip catheters and 4 irrigated-tip catheters.
Focal Atrial Tachycardia
A total of 215 procedures were undertaken, with a mean of 4.4 (3) procedures per center. This arrhythmogenic substrate was treated by 43 centers when originating in the right atrium, but only 21 centers treated those originating in the left atrium.
The number of successful procedures was 170 (79%). The FAT site was reported in 199 procedures, and success rates were similar for those originating in the right and left atrium: 78.5% (124/158) and 75.6% (31/41), respectively. Only 1 major complication occurred (pneumothorax). In 20 cases, a nonstandard catheter was used: 5 8-mm tip catheters, 13 irrigated-tip catheters, and 2 cryoablation catheters.
Cavotricuspid Isthmus
This was the third most frequently treated type of arrhythmia. Unlike the previous year, the pediatric center also carried out this type of procedure (once). The number of successful procedures was 1507 (mean, 30.7 [19]; range, 1-73). Success was achieved in 1447 cases (96%). There were 12 major complications (0.8%), the most frequently reported being those related to vascular access.8 In 1 case, definitive pacemaker placement was required due to AV block and no deaths were reported related to the procedure. Two patients suffered substantial pericardial effusion and 1 had a stroke. In 1394 cases (92.5%), a nonstandard catheter was used: an 8-mm catheter in 937 cases (67.2%), an irrigated-tip catheter in 396 cases, and a cryoablation catheter in 62 cases.
Macroreentrant Atrial Tachycardia/Atypical Atrial Flutter
This type of arrhythmia was treated in 24 centers (51%). A total of 106 procedures were undertaken (mean of 4 procedures per center; range, 1-23). The procedure was successful in 73 cases (68.8%). There were 2 complications, cardiac tamponade and femoral pseudoaneurysm.
In 99 cases, the MAT site was known: 42 were right side and 57 left side, with success rates of 71% and 75%, respectively. In 81% of the cases, a catheter other than a 4-mm tip catheter was used: 40 procedures with an 8-mm tip catheter and 41 procedures with an irrigated tip catheter.
Atrial Fibrillation
In total, 540 AF ablation procedures were performed in 26 participating centers (56.5%). These figures correspond to a mean of 20.7 procedures per center, although 3 centers undertook 1 procedure, and 1 center undertook 2.
Of the total number of procedures, we have information on the technical approach for 470 (88%). Thus ostial isolation of pulmonary veins was performed in 210 (44.6%) of the cases and circumferential ablation in 265 of the cases cases (55.4%). In 5 procedures, the right atrium was also ablated.
We have information on the ablation catheter used in 469 procedures; the irrigated-tip catheter was chosen in 75% of the cases and the 8-mm tip in the remaining cases. Cryoablation was used in 6 cases.
A total of 28 complications (5.1%) were reported. These were as follows: significant pericardial effusion/cardiac tamponade (16, 57%), acute coronary syndrome (4, 14%), vascular access complications (4, 14%), acute heart failure (3, 11%), stroke (1, 4%).
Idiopathic Ventricular Tachycardia
A total of 149 IVT ablation procedures were reported in 41 centers (mean, 3.6 ablations per center). Success was achieved in 119 procedures (80%) and only 1 complication (AV block requiring definitive pacemaker placement) was reported.
The type of VT was known in 134 procedures: 90 in the right ventricular outflow tract, 12 in the left ventricular outflow tract, 21 fascicular VT, and 11 classed as "other site," with success rates of 83%, 75%, 85%, and 72%, respectively.
In more than 80% of the cases, the ablation catheter used had a 4-mm tip.
Ventricular Tachycardia Related to Postmyocardial Infarction Scarring
A total of 36 centers (78%) undertook 178 VT-AMI ablation procedures (4.9 ablations per center). The following complications were reported (n=12, 6.7%): vascular access (3), AV block (2), significant pericardial effusion (2), stroke (2), acute heart failure (2), and acute coronary syndrome (1).
The type of ablation done was reported in 153 cases: in 107 the approach was conventional whereas a substrate-based approach was used in 46 cases. In 99 procedures (64.7%), the catheter used for ablation was nonstandard: 69 procedures used 8-mm tips and 30 used irrigated tips.
Ventricular Tachycardia Not Related to Postmyocardial Infarction Scarring
In total, 66 ablation procedures for this type of arrhythmia were performed in 26 laboratories. There were 2 complications (3%): cardiac tamponade and stroke.
Success was achieved in 62.7% of the procedures (37/59). The types of tachycardia treated were as follows: 14, right ventricular arrhythmogenic dysplasia; 10, bundle branch block; 26, dilated cardiomyopathy or ischemic heart disease; and 9 were reported as "other type." The overall success rates for these types of tachycardia were 71.4%, 90%, 42.3%, and 77.7%, respectively.
Almost half the procedures (44%) used a nonstandard ablation catheter: 18 procedures used an 8-mm tip catheter and 8 used irrigated-tip catheters.
DISCUSSION
The registry for 2006 was characterized by continuing the trend, seen in 2005, towards more procedures,5 after a certain downward tendency in previous years (Figure 7). With the participation of 1 more center than last year, 411 and 2421 more procedures were done than in 2006 and 2005, respectively. Apart from these tendencies, the rest of the analysis (outcome, complications, participation, and others) is characterized by being very similar to the registry of the previous year.
Figure 7. Change in the number of participating centers and the number of ablation procedures recorded in the Spanish Catheter Ablation Registry since 2001.
The technical facilities of the catheterization laboratories, in contrast to what was found between 2004 and 2005, remained stable, with the same number of mapping systems and additional techniques such as cryoablation or intracardiac ultrasound.4,5
Particular attention should be paid to the composition of the laboratories in terms of the medical staff. We have found a considerable increase in the overall number of ablation procedures performed, the acquisition of accompanying techniques by a substantial number of laboratories, and the treatment of increasingly complex substrates (atrial fibrillation, macroreentry atrial arrhythmias, or VT-AMI). In addition, 71% of the catheterization laboratories also implanted cardioverter-defibrillators and pacemakers (around 50% more than in 2001),1 with the corresponding health care burden that this implies. Despite this higher burden, the number of staff has not changed substantially since the registry started more than 6 years ago. Whereas in 2002 there were an average of 2.2 physicians per laboratory, with a mean of 1.6 with full-time positions,2 the corresponding figures for 2006 were 2.3 and 1.7, respectively. That is, we have still not reached the average of 2 full-time physicians working in catheterization laboratories in Spain. This analysis is very similar if we consider other variables such as the number of physicians in training, those with grants, nursing staff, and axillary staff.
With regard to the approach to specific substrates, the percentage is almost identical to the previous year. The most noteworthy figure is the 8% of ablations corresponding to atrial fibrillation. The number of centers that treat atrial fibrillation with ablation has increased only slightly this year (26 in 2006 compared to 24 in 2005),5 although there are 3 centers that have performed fewer than 3 procedures. The staffing limitations mentioned earlier can at least partially explain why the number of patients with this arrhythmia treated has increased slowly. Ablation of this type of arrhythmia takes on average at least 3 times longer than ablation of commonly treated substrates (AVNRT or AP).8 Likewise, there has been no significant increase this year in the number of ablations for ischemic ventricular tachycardia, perhaps because of the constant improvement in medical and interventionist treatment offered to patients with ischemic heart disease.
The high rates of success (>90%) with a really low rate of complications (approximately 1.5%) are nothing new in this registry. Deaths during ablation procedures were extremely uncommon, as in previous years (<1/1000). The success rates and rates of complications according to each type of arrhythmia are also similar to previous years. Noteworthy this year has been a slight decrease in complication rates for atrial fibrillation and a slight increase for ventricular tachycardia, probably reflecting the increasing complexity of patients with this type of arrhythmia.
CONCLUSIONS
The 2006 registry continues the upward tendency observed in the previous year. Thus, more than 6000 ablation procedures were performed, with constant success and complication rates. Data were collected from the majority (48 this year) of catheterization laboratories in Spain.
As in previous years, this year, the increase in the number and complexity of the ablations performed, as well as the laboratories that also implant devices has not been reflected by an increased number of staff.
ACKNOWLEDGMENTS
The coordinators of the registry would like to express their thanks to all who participated in the 2006 Ablation Registry, who have voluntarily sent data on their procedures; to the previous coordinators of the registry, in in particular to Dr Miguel Álvarez López, for his invaluable help; to Cristina Plaza for her excellent administrative support; and to Pilar Ara for her support in maintaining the database of the registry.
Catheterization Laboratories by Spanish Autonomous Regions and Provinces That Participated in the 2006 Spanish Catheter Ablation Registry (With the Responsible Physician in Parenthesis)
Andalusia. Cadiz: Hospital Puerta del Mar (Dr L Cano), Granada: Hospital Virgen de las Nieves (Dr M Álvarez), Huelva: Hospital Juan Ramón Jiménez (Dr P Moriña), Malaga: Hospital Clínico de Málaga (Dr A Barrera), Seville: Hospital Virgen de Macarena (Dr E Díaz-Infante), Hospital Virgen de Valme (Dr García Medina).
Aragon. Saragossa: Hospital Lozano Blesa (Dr G Rodrigo), Hospital Miguel Servet (Dr A Asso).
Asturias. Oviedo: Hospital Central de Asturias (Dr N Pachón).
Balearic Islands. Majorca: Hospital Son Dureta (Dr MC Expósito), Policlínica Miramar (Dr N Alvarenga), Hospital Son Llatzer (Dr X Fosch).
Canary Islands. Tenerife: Hospital Nuestra Señora de la Candelaria (Dr R Romero), Hospital Universitario de Canarias (Dr A Rodríguez González).
Cantabria. Hospital Marqués de Valdecilla (Dr FJ Rodríguez).
Castile-La Mancha. Toledo: Hospital Virgen de la Salud (Dr E Castellanos).
Castile and León. Burgos: Hospital General Yagüe (Dr J García); León: Hospital de León (Dr ML Fidalgo); Salamanca: Hospital Clínico Universitario (Dr J Jiménez); Valladolid: Hospital Clínico Universitario (Dr E.García Morán), Hospital Río Hortega (Dr B Herreros).
Catalonia. Barcelona: Hospital de Bellvitge (Dr X Sabaté), Hospital del Mar (Dr J Martí), Hospital Clínic (Dr L Mont), Hospital Vall d'Hebron (Dr A Moya), Hospital de la Santa Creu i Sant Pau (Dr E Rodríguez Font), Hospital San Juan de Dios (Dr J Brugada), Centro Cardiovascular Sant Jordi (Dr J Brugada), Clínica Sagrada Familia (Dr A Moya).
Autonomous Community of Valencia. Alicante: Hospital Universitario de Alicante (Dr JG Martínez); Valencia: Hospital Clínico (Dr R Ruiz Granell), Hospital General (Dr V Palanca), Hospital La Fe (Dr J Osca).
Galicia. A Coruña: Hospital Clínico de Santiago de Compostela (Dr JL Martínez Sande), Hospital Juan Canalejo (Dr L Pérez).
Madrid. Clínica Puerta de Hierro (Dr I Fernández Lozano), Hospital 12 de Octubre (Dr R Salguero), Hospital Clínico San Carlos (Dr N Pérez Castellano), Hospital Gregorio Marañón (Dr J Almendral), Hospital de Getafe (Dr A Pastor), Hospital Severo Ochoa (Dr A Grande), Hospital La Paz (Dr JL Merino), Clínica USP San Camilo (Dr JL Merino).
Murcia. Hospital Virgen de la Arrixaca (Dr A García Alberola).
Navarre. Clínica Universitaria de Navarra (Dr A Macías), Hospital de Navarra (Dr N Basterra).
Basque Country. Bilbao: Hospital de Cruces (Dr A Bodegas), Hospital de Basurto (Dr MF Arcocha).
ABBREVIATIONS
AF: atrial fibrillation
AP: accessory pathways
AV: atrioventricular
AVN: atrioventricular node
AVNRT: atrioventricular nodal reentry tachycardia
CTI: cavotricuspid isthmus
FAT: focal atrial tachycardia
IVT: idiopathic ventricular tachycardia
MAT: macroreentrant atrial tachycardia
NFMS: nonfluoroscopic mapping system
VT-AMI: ventricular tachycardia related to postmyocardial infarction scarring
VT-NAMI: ventricular tachycardia not related to postmyocardial infarction scarring
At the end of this article is a list of the centers and physicians that participated in the 2006 Spanish Catheter Ablation Registry.
Correspondence: Dr. I. García Bolao.
Irunlarrea, 13, 8.°-D. 31008 Pamplona. España.
E-mail: igarciab@unav.es