Keywords
A list of the physicians in charge of each center´s data appears at the end of the article.
INTRODUCTION
This article details the findings of the IV Spanish Catheter Ablation Registry based on catheter ablation procedures carried out in 2004. This information was provided voluntarily by most of the electrophysiology laboratories in Spain.
MATERIALS AND METHOD
Similar to 2003,1 data were gathered retrospectively --via a questionnaire (paper or online) sent to all electrophysiology laboratories--and prospectively via a central computerized database containing specific information on each ablation procedure. The system for sending, processing, and forwarding data to the coordinators was similar to previous years. The form and database used in 20031 were barely modified and neither were the classification of the types of arrhythmic substrates and the success criteria for most substrates changed.2,3
Currently, there are different approaches to ablation of atrial fibrillation (AF) and to ventricular tachycardia related to post-acute myocardial infarction (AMI) scarring. They have different targets and as such can be used within the same procedure. On the other hand, the clinical outcome of some of these approaches cannot be analyzed in the short term. Thus, the data regarding success/failure in both substrates should be analyzed with caution. Nevertheless, we provide quantitative data obtained from the replies given by the specialists responsible for the procedure.
Statistical Analysis
Quantitave variables are expressed as mean± standard deviation. Qualitative variables and proportions were analyzed with χ2 and Fisher test when necessary. Quantitative variables were analyzed with the Student t test. The percentages of success and complications were calculated in relation to the number of patients. P-values <.05 were considered statistically significant. The statistical analysis was performed with the statistical software SPSS 11.0 (SPSS Inc. Chicago, Ill, USA).
RESULTS
A total of 36 centers submitted data; the characteristics of the participating centers are listed in Table 1 and their geographical distribution in Appendix. Some 31% (n=11) of the centers sent their data via the prospective registry form which was considerably less than in the 2003 registry.1
Infrastructure and Resources
A total of 97% of the centers were tertiary centers, 86% (n=31) were publicly funded, and 80% (n=29) offered cardiovascular surgery.
Digital radiology laboratories were available in 48.6% of the centers (n=17). Nevertheless, there were portable radiology systems in 40% of the laboratories which supplied answers to this variable (n=26). The radiology room was exclusively dedicated to electrophysiology procedures in 75% of the centers (n=27). A median of 5 weekdays were dedicated to electrophysiology (range, 1-5). Only 10 electrophysiology laboratories did not undertake device implantation techniques (pacemakers, defibrillators). External/internal electrical cardioversion was carried out in most (72%) laboratories.
Computerized polygraph systems were available in 94% of the laboratories. In addition, 6 laboratories offered intracardiac echocardiography. Radiofrequency catheter ablation was performed in all laboratories. Furthermore, 6 centers offered cryoablation.
Human resources in the publicly financed centers are listed in Table 2. Two or more staff physicians worked full-time in the electrophysiology laboratory in 61% of the centers (19/31). Sixteen centers (52%) also had fellows.
Of the 23 centers that performed transseptal catheterization, the electrophysiologist participated as operator in 17 centers, and was the only operator in nine. This technique was not performed in 12 laboratories and one center did not reply to this section. The mean waiting time needed after an effective radiofrequency application to consider the procedure definitively successful was 27±5 min (range, 1530; median, 30).
Non-Fluoroscopic Intracardiac Navigation Systems
Most laboratories (67%, n=24) had at least 1 non-fluoroscopic intracardiac navigation system (nFINS), four laboratories had 2 nFINS and 1 had 3. The total distribution of these devices was as follows: 7 centers had a CARTO system®, 13 had LOCALISA®, and 4 had NavX® and RPM® systems. Some 71% of the public centers had these systems versus 40% of the private ones (P=NS). In the public centers some variables were associated with the availability of some type of system. For example, this was more frequent in centers with heart surgery (79 vs 43%; P=.15), and digital radiology rooms (100% vs 50%; P<.01), in centers performing transseptal catheterization (90% vs 36.4%; P<.01), with intracardiac echocardiography (100% vs 64%; P=.14) and in centers performing more than 100 procedures per year (89.5% vs 42%; P<.05).
Overall Results
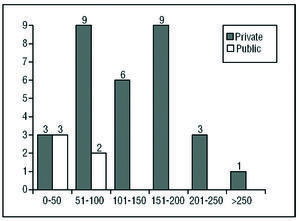
The total number of ablation procedures undertaken by the 36 centers (100% of all the centers analyzed) was 4147, which represents 115±66 procedures per center (median, 103; range, 25-270); the outcome was reported in 4092 procedures (success vs failure) and complications were reported in all of them. Figure 1 shows the distribution of the number of procedures per laboratory.
Figure 1. Number of electrophysiology laboratories in the Spanish Registry classified by number of catheter ablation procedures.
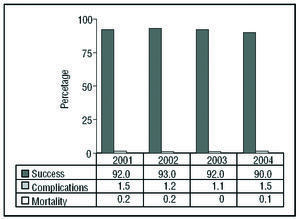
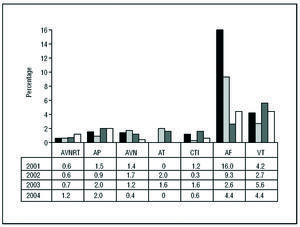
The global percentage of success was 90% (3685/4092 procedures), major complications 1.5% (n=61) and mortality 0.1% (n=3 patients). The data are similar to previous years (Figure 2). The 3 deaths registered were associated with the ablation of an accessory pathway (AP), a ventricular tachycardia of ischemic etiology, and a ventricular tachycardia of non-ischemic origin.
Figure 2. Comparison by outcomes (success, complications and mortality) observed since 2001.
Results by Substrate
The average number of different substrates treated in the same center was 7.4±1.8 (median, 7; range, 3-10); this number was significantly higher in publicly financed centers (7.7±1.6 vs 5.6±1.9; P=.016).
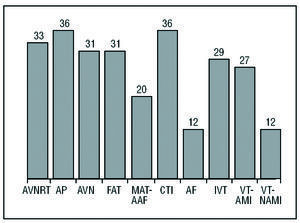
Only four centers (11%) treated all the substrates. All the centers treated patients with AVNRT, AP and cavotricuspid isthmus (CTI), whereas only 12 centers performed atrial fibrillation ablations (AF) (Figure 3).
Figure 3. Number of centers treating each type of substrate. CTI indicates cavotricuspid isthmus; AF, atrial fibrillation; AVN, atrioventricular conduction/node; FAT, focal atrial tachycardia; MAT-AAF, macroreentrant atrial tachycardia-atypical atrial flutter; AVNRT, atrioventricular nodal reentry tachycardia; IVT, idiopathic ventricular tachycardia; VT-AMI, ventricular tachycardia related to post-myocardial infarction scarring; VT-NAMI, ventricular tachycardia not related to post-myocardial infarction scarring; AP, accessory pathways.
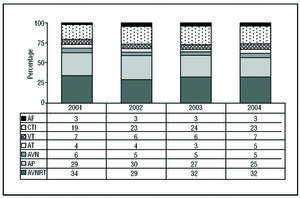
The most frequently treated substrate (as in earlier registries) was AVNRT, followed by AP and CTI ablation which together accounted for 80% of total ablation procedures performed in Spain. The remaining 20% was distributed among the other 7 substrates. No significant differences were observed regarding previous registries (Figure 4).
Figure 4. Comparison with early registries of relative frequency of substrates treated. AF indicates atrial fibrillation; CTI, cavotricuspid isthmus; AVN, atrioventricular conduction/node; AVNRT, atrioventricular nodal reentry tachycardia; AP, accessory pathways; AT, atrial tachycardia; VT, ventricular tachycardia.
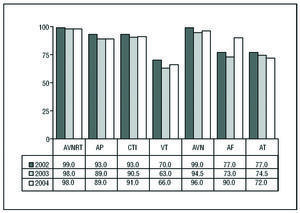
The most complex substrates were more frequently treated in centers with some kind of nFINS, although this only reached statistical significance in the case of VT unrelated to AMI. Table 3 shows the distribution of substrates per center, and Table 4 the percentage of success and complications by substrates. Figures 5 and 6 show how data compares with earlier registries.
Figure 5. Comparison with previous registries of the success percentage of the different substrates. AF indicates atrial fibrillation; CTI, cavotricuspid isthmus; AVN, atrioventricular conduction/node; AVNRT, atrioventricular nodal reentry tachycardia; AP, accessory pathways; AT, atrial tachycardia; VT, ventricular tachycardia.
Figure 6. Comparison with previous regisries of the complications percentage of the different substrates. CTI indicates cavotricuspid isthmus; AF, atrial fibrillation; AVN, atrioventricular conduction/node; AVVNRT, atrioventricular nodal reentry tachycardia; AP, accessory pathways; AT, atrial tachycardia; VT, ventricular tachycardia.
Atrioventricular Nodal Reentry Tachycardia
A total of 1286 ablation procedures were undertaken (36±21 per center; range, 5-94). The number of successful procedures was 1264 (98.3%). A total of 15 major complications occurred (1.2%), the most frequent being complete AV block (n=9; 0.7%).
Accessory Pathways
Some 1054 ablation procedures were performed (29±19 per center; range, 3-80). Success was achieved in 938 procedures (89%) and major complications occurred in 20 (1.9%). The most frequent (n=10; 50%) was arteriovascular complication (0.95%). In 4 cases substantial pericardial effusion occurred. One patient (0.09%) died 6 days after the procedure as a consequence of pulmonary thromboembolism.
Cavotricuspid Isthmus
A total of 973 procedures were performed (27±18 per center; range, 4-71). Success was achieved in 884 procedures (91%) and 6 complications occurred (0.6%), one of them being reported as ischemia.
Atrioventricular Node Ablation
Only the prospective registry differentiated between the type of procedure used (AVN modulation or ablation or permanent pacemaker implantation) since the results combine both procedures. A total of 227 procedures were performed (7±6 per center; range, 1-27). Success was achieved in 219 procedures (96%) and the only major complication was a pericardial effusion (0.4%).
Focal Atrial Tachycardia
Thirty centers treated this substrate (n=132 procedures; 4±3 per center; range, 1-14) and 29 reported the results of 129 procedures. Success was achieved in 101 of the 129 procedures (78.3%) and no major complication occurred. The same percentage of centers with or without nFINS treated this substrate.
Macroreentrant Atrial Tachycardia/Atypical Atrial Flutter
A total of 66 procedures were performed (3.3±3.3 per center; range, 1-14). Success was achieved in 41 procedures (62%) and no major complication occurred. This substrate was treated by 62.5% of the centers with nFINS versus 42% without such systems (P=.3).
Atrial Fibrillation
Twelve centers dealt with this substrate (n=137 procedures; 11±10 per center; range, 1-37) and 9 reported the outcome of 64 procedures. Success was achieved in 58 procedures (90%) and 6 complications occurred (4.4%): 1 pericardial effusion, 1 cardiac tamponade, 1 embolism, 1 transitory stroke/ischemic event, 1 arteriovascular complication, and 1 ischemic episode.
This substrate was treated by 42% of the centers with nFINS versus 17% without such systems (P=.26).
Idiopathic Ventricular Tachycardia
A total of 121 procedures were carried out in 29 centers (4±3 per center; range, 1-10) and 112 procedures were analyzed (28 centers), with success reported in 88 (78.5%). Four major complications occurred (3.3%), the most significant being 2 cases of pericardial effusion and 1 stroke.
Ventricular Tachycardia Associated With Postinfarction Scarring
Twenty-seven centers treated this substrate carrying out 110 procedures (4±5 per center; range, 1-24), and all but one reported on the outcome (n=86). Success was achieved in 64 procedures (74%) and there were seven major complications (6.3%). One patient (0.9%) died suddenly 3 h after the procedure. The same percentage of centers with or without nFINS treated this substrate.
Ventricular Tachycardia Not Associated With Postinfarction Scarring
Thirty-eight procedures were performed in 12 centers (3±1.9 per center; range, 1-7). Success was achieved in 28 procedures (74%). One patient (2.6%) died due to cardiogenic shock after ablation. This substrate was treated by 46% of the centers with nFINS versus 8% without such systems (P=.03).
DISCUSSION
The findings of the Spanish Catheter Ablation Registry established by the Spanish Society of Cardiology Working Group on Electrophysiology and Arrhythmias are reported for the fourth consecutive year. Although participation has been lower than in previous years,1-3 we have been able to analyze a high number of ablation procedures (>4000).
There may be several reasons for the drop in participation. As in previous years, participation in this registry was voluntary and thus involves additional work on the part of participating physicians. Two different formats were used for sending data--retrospective and prospective--and this might have led to some confusion. The Working Group is aiming at creating a single simple form that can be filled in prospectively case by case. This approach is also being implemented in Europe (CARDS Project)4 by the use of a common and prospective database.
In the current registry, the centers using the prospective registry were clearly fewer, which means that we were not able to analyze data regarding epidemiological variables, anticoagulation, etc., which were reported in the previous registry.1
Infrastructure and Resources
The number of full-time electrophysiologists in the laboratories (an average of 1.5, approximately) has not changed since 1997. As in earlier registries, publicly financed laboratories with at least 2 electrophysiologists undertake a higher number of ablation procedures (145±64 vs 94±53; P<.03); in fact, only 17% (2/12) of the centers with less than 2 electrophysiologists performed more than 150 ablations, compared to 58% (11/19) of the centers with 2 or more specialists (P<.05).
Each year we have observed an increase in the number of centers with nFINS (26% in 2001, 47% in 2002 and 71% in 2004). Although each system is based on a different approach, all of them are used to improve outcomes in complex procedures (AF, left atrial flutter, etc) and in fact only 2 laboratories carried out AF ablation without nFINS. Several variables probably influenced the availability of these systems. However, we have to point out that, even when bearing in mind the limitations of the analysis due to the low number of cases, the centers with a greater number of procedures (>100) and which carry out transseptal catheterization have a higher percentage of nFINS. Therefore, it is not surprising that the centers with nFINS deal with more complex substrates and more frequently. Although we lack data in this regard, it seems reasonable to assume that patients coming from hospitals where these kinds of ablations are not available are referred to such centers.
It is interesting to note the increasing use of cryoablation; 6 centers used it during 2004 in contrast to 2 in 2003 and 2002. The increasing number of substrates treated with this new source of energy (i.e., ventricular arrhythmias, cavotricuspid isthmus, and pulmonary veins), together with its proven advantages, suggest that cryoablation will become more widespread.5-7
Overall Results and by Substrate
No significant differences were found compared to previous years. In general, success was slightly higher than 90%, with a complications rate less than 2% and a mortality rate of 1-2 patients for every 1000 patients treated. These figures have remained constant since 2001.
The percentage distribution of the substrates treated has not changed significantly. Atrioventricular nodal reentry tachycardia, accessory pathways, and atrial flutter continue to be the arrhythmias more frequently treated in Spain. This makes sense because in these kinds of arrhythmias the indication for electrophysiological study and later ablation8 is fairly clear to the clinical cardiologist. However, the "curative" treatment of AF does not rise above 3% of all the ablation procedures, even though it continues to be the most prevalent arrhythmia seen in general outpatient clinics.8 Although some centers treating this substrate have not sent their data, this percentage is not expected to increase significantly. Evidence already exists in the literature that catheter ablation has greater efficacy than antiarrhythmic drugs in controlling AF.9,10 Knowledge concerning the results of AF ablation in Spain should help to increase the indication for interventionist treatment.
In the 2003 registry, the percentage of success in AP ablation reported by the centers that sent prospective data was lower than those following the retrospective method. Although no significant differences were found this year, after analyzing the prospective data, the percentage of success for this substrate was <90%. The greater reliability of the prospective data seems to be the most reasonable explanation for this fact.1
The percentage of success in AF ablation should be interpreted with caution, given the difficulties in defining the short-term target of ablation, the fact that some centers did not send data regarding the procedural success and the doubtful relationship between short-term success and clinical efficacy in the mid- or long term. However, in the last 3 years, the percentage of complications has remained less than 5%, a figure similar to the one reported in the world registry for AF ablation.11
CONCLUSIONS
Although participation in this registry was slightly less than in previous years, the analysis of over 4000 ablations confirms the stability of the outcomes of this procedure in Spain. The distribution of substrates and the success and complication rates are both similar to 2003. Compared to earlier years, there was a slight improvement in the technology used by the laboratories, which was not matched by an increase in electrophysiologists per center.
List of Physicians Responsible for Data Management in the Centers Participating in the Spanish Ablation Registry for 2004
N. Alveranga, J. Amador, M.F. Arcocha, A. Barrera, N. Basterra, L. Cano, E. Castellanos, S. del Castillo, J.J. Esteve, C. Expósito, I. Fernández Lozano, M.L. Fidalgo, A. García Alberola, I. García Bolao, D. García Medina, B. Herreros, M. López Gil, J. Martí, J.G. Martínez, J.L. Martínez Sande, J.L. Merino, J.L. Moríñigo, J. Osca, A. Pachón, V. Palanca, A. Pedrote, L. Pérez Álvarez, N. Pérez Castellano, F.J. Rodríguez Entem, E. Rodríguez Font, G. Rodrigo Trallero, R. Romero, X. Sabaté, L. Tercedor, and X. Viñolas.
ABBREVIATIONS
AF: atrial fibrillation.
CTI: cavotricuspid isthmus.
AVN: atrioventricular node.
nFINS: non-fluoroscopic navigation system.
FAT: focal atrial tachycardia.
AVNRT: atrioventricular nodal reentry tachycardia
VT: ventricular tachycardia.
AP: accessory pathways.
Correspondence: Dr. M. Álvarez López.
Unidad de Arritmias. Servicio de Cardiología. Hospital Universitario Virgen de las Nieves.
Avda. de las Fuerzas Armadas, 2. 18014 Granada. España.
E-mail: malvarez@secardiologia.es