To the Editor,
Lithium carbonate is the treatment of choice for relapse prevention in bipolar disorder. It has a narrow therapeutic margin and overdoses are potentially fatal. In one patient series, mortality due to acute intoxication was 25% and that due to chronic intoxication, 9%.1 The recommended therapeutic level is 0.6–1.2mEq/L for the prevention of manic episodes and 1.0–1.5mEq/L for the treatment of acute mania.
It has been reported that lithium has cardiotoxic effects, though they are infrequent and usually occur in patients with underlying heart disease. We present the case of a 69-year-old Caucasian woman who was admitted for permanent pacemaker implantation following investigations for dizziness, asthenia, adynamia, and frequent falling episodes without associated loss of consciousness.
Her clinical history revealed that she was overweight and was receiving olmesartan–amlodipine for high blood pressure, lithium, 400mg every 12h, for bipolar disorder, and venlafaxine and lamotrigine for anxiety and depression.
Twenty-four-hour Holter monitoring was carried out and showed bradycardia and frequent premature ventricular complexes, which led to admission to our center.
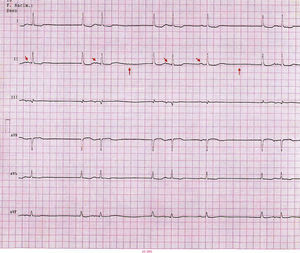
The patient was conscious at admission, her blood pressure was 130/60mmHg and her heart rate was 65beats/min. Cardiorespiratory examination was normal. She reported trembling, muscle weakness and hallucinations. The ECG revealed sinus node dysfunction (i.e. sinoatrial block, sinus pause and sinus bradycardia), premature ventricular complexes, and negative flat T waves in ECG leads in the extremities (Figure 1).
Figure 1. Baseline sinus rhythm at 60beats/min (oblique arrows indicate P waves). First-degree type-2 sinus node dysfunction (vertical arrows). Flattening of T waves.
Laboratory studies included measures of creatinine (0.84mg/dL), urea (37mg/dL), glucose (95mg/dL), Na (132mEq/L), K (4.1mEq/L), and therapeutic lithium (2.32mEq/L; normal range 0.6–1.2mEq/L), which confirmed the diagnosis of lithium intoxication. During hospitalization, the lithium regimen was suspended but venlafaxine and lamotrigine were continued on the recommendation of the psychiatry department.
Although the sodium channel blocker lamotrigine is known to be associated with arrhythmogenesis and a relationship has been reported between venlafaxine and a long PR interval and bundle branch block, the disappearance of neurological symptoms and the recovery of sinus rhythm at 60beats/min on normalization of the lithium level led us to attribute the bradyarrhythmia to lithium intoxication.
Chronic lithium intoxication generally presents with nonspecific symptoms and its diagnosis requires a high degree of diagnostic suspicion. In 2001, a review of the literature2 found that the most important predictors of lithium intoxication were: (a) diabetes insipidus (nephrogenic secondary to chronic lithium treatment); (b) age >50 years; (c) hypothyroidism, and (d) deterioration in renal function.
The symptoms most frequently associated with lithium intoxication are gastrointestinal (i.e. nausea, vomiting and diarrhea) and neurologic (i.e. neuromuscular excitability, trembling, muscle weakness, ataxia, and confusion or delirium). Cardiologic signs and symptoms appear in only 20%–30% of patients.3 The most frequent ECG findings are T wave changes (i.e. flattening). Bradyarrhythmias have also been described: namely, sinus node dysfunction and varying degrees of atrial block, which occasionally require temporary pacemaker implantation. In a series of 19 patients, Talati et al.4 reported a variety of symptoms associated with overdoses: syncope (7), dyspnea (2), central nervous system toxicity (4), atypical chest pain, and weakness or lethargy. Eight patients presented with a lithium concentration <1.5mEq/L. Sinoatrial block was the most frequent cardiac repercussion, followed by sinus bradycardia. In most patients, these changes were corrected by lithium withdrawal. The cardiovascular signs and symptoms of lithium toxicity typically appear after the neurologic symptoms. Although infrequent, arrhythmias, which are potentially fatal with lithium overdoses, have been reported.5
In conclusion, given that the cardiotoxicity induced by lithium is reversible once the concentration returns to normal, it is important to bear in mind that ECG changes observed in patients being treated with lithium may be linked to the plasma concentration, even in the absence of an overdose.
Corresponding author: juan.acostamartinez@yahoo.es