The article by Frigola-Capell et al.1 published in Revista Española de Cardiología reports the findings from a cohort study of 5659 patients with incident heart failure (HF) over a 3-year period in primary care practices (PCP) in the Catalonian region of Spain. The primary focus of this report are patients with a new diagnosis of HF during the 3-year period (incident HF). The cohort in this study required a diagnosis of HF and prescription of diuretics, which increased the likelihood of appropriate classification for the diagnosis of HF.
As would be expected, the patients were elderly (mean age of 77) and predominantly female (61%). In this PCP-managed cohort, most patients were receiving an angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (78%), but the use of beta-blockers was quite low (34%). We do not know how many had HF with preserved systolic function, in which the benefits of beta-blockers or other HF medications is not established. There was no reported measurement of ejection fraction, blood pressure, or New York Heart Association class, which is major limitation of this type of electronic record research.
Based on the population managed by the PCPs, approximately 1.3% of the population had HF either at baseline or developed HF during the 3 years of observation (13 008 HF patients/1 039 342 total patients). This prevalence of HF is lower than population estimates for the US (2.4% in the American Heart Association 2012 update) or the HF estimates reported in the National Health and Nutrition Examination Survey 2007-2008 (2.0%).2 In the US, the prevalence of HF increases with age and is around 7% at 60-79 years and around 12% at 80 years or more, concordant with most incident HF being in the elderly population, as seen in this cohort.2
The incidence of HF over the 3-year period was quite low (approximately 1.8 per 1000 person-years). In the younger population in the Multi-Ethnic Study of Atherosclerosis (mean age, 63 years), the incidence of HF was 3.1 per 1000 person years and varied by ethnic group (4.6, 3.5, 2.4, and 1.0 in 1000 person-years for African American, Hispanic, white and Chinese American).3 In the Kaiser Permanente cohort with age greater than 65 years, the incidence was 1.2 per 1000 person-years with only 22% receiving the intial diagnosis of HF in the outpatient setting.4 In the Catalonian cohort of ambulatory HF patients, the majority of patients (90%) were not hospitalized during the 3 years of observation, which is quite reassuring for ambulatory HF patients and contrasts with the high rate of readmission for patients discharged after an episode of acute decompensated HF.5 This result also contrasts with findings in Italy, where younger chronic HF patients had a 5.9% mortality rate but a higher (10%) hospitalization rate within 1 year.5
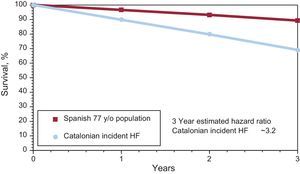
The prognosis for HF in this elderly Catalonian cohort is better than most other reported ambulatory HF populations. The mortality for incident HF vs the general Spanish population aged 77 years is shown in Figure. The authors report 31% mortality at 3 years after the diagnosis of HF vs approximately 11% mortality in the general population. Thus, the diagnosis of new HF is associated with an approximately 3.2-fold increase in the risk of death vs the general population. The approximately 12% annual or 31% over 3-year mortality for all patients with incident HF over 3 years is similar to the figures reported by some other observational studies of HF such as the Italian HF registry (∼6% mortality at 1 year in younger incident HF patients discharged from hospital)5 and Sweden (prevalent HF, 34% mortality at 3 years with 40% enrolled as ambulatory outpatients and 60% enrolled as inpatients).6 The incident HF survival of 90% at 1 year was superior to that reported in Framingham in 1990-1999 (∼26% mortality at 1 year)7 and in Kaiser-Premanente (∼30% at 1 year).4 Because of the cohort design, patients who had an incident HF diagnosis initially in the hospital and did not survive to follow-up with the PCP may not have had HF recorded in the PCP records and thus would not have been included in this analysis. Given the high 30-day mortality with incident hospitalized HF (∼9%-10% in Kaiser Permanente), the proportion of HF deaths that were not included in this analysis could have been sizable. Complete ascertainment of deaths is highly important, but, given the age of the population, it seems unlikely that large numbers would have relocated to other countries or areas of Spain and would have been lost to follow-up.
The survival for the general Spanish population at age 77 (www.mortality.org) is shown along with the observed survival for a new diagnosis of heart failure (incident) in a primary care clinic in Catalonia. The observed 3-year mortality was approximately 3.2 fold higher (31% vs 11%). HF, heart failure.
What is not appreciated by many is the marked difference in mortality depending on the when observation begins. In the Italian HF Registry, 1-year mortality was 4-fold higher in patients with acute decompensated HF than ambulatory outpatients with HF (24% vs 5.9%).5 In this same Italian HF cohort, admission for cardiovascular reasons over 1 year was approximately 25%-30% for acute decompensated HF (17% of ambulatory HF outpatients) compared with only around 6.5% (10.3% over 1.6 years of median HF observation) in the Catalonian cohort. What is quite remarkable is that the death rate was markedly higher than the hospitalization rate for cardiovascular reasons in Catalonia (31% vs 10%). This result contrasts with those of most other observational studies and trials, in which HF patients have a higher hospitalization rate than death rate (∼28% death and ∼48% hospitalization for cardiovascular reasons in the GISSI-HF trial [Effect of n-3 polyunsaturated fatty acids in patients with chronic heart failure] over 4 years)8 in Italy, another Mediterranean county.
The life expectancy for the general Spanish population at age 77 is approximately 11 years. It is quite reasssuring that ambulatory incident HF patients managed predominantly by PCPs have a life expectancy of approximately 5.5 years or a reduction of around 5.5 years due to HF estimated by a Gompertz type analysis.9
The Cox model findings are similar to those of many other prognostic models. Older patients with comorbidities (diabetes mellitus, chronic obstructive pulmonary disease, chronic kidney disease, and ischemic heart disease) have a higher risk of death. The authors’ overall c statistic for the model is 0.67, which is only modest discrimination. This model has simple variables without New York Heart Association or ejection fraction, which makes it more appropriate for large insurance database-type analyses. The authors have not provided a nomogram or another method to allow the user to estimate mortality for patients seen in the office. It is likely that inclusion of simple variables such as New York Heart Association class, ejection fraction, blood pressure, and measured creatinine would improve the predictive accuracy of the model.
What, then, are the characteristics of Catalonia that may improve the incidence of HF and subsequent survival in patients with HF? Ethnicity, at least Hispanic ethnicity in the Multi-Ethnic Study of Atherosclerosis trial (United States), was not associated with a lower incidence of HF.5 Certainly, the Mediterranean diet and lifestyle are prime candidates. A recent large randomized trial in Spain demonstrated a lower cardiovascular event rate (myocardial infarctions, stroke, and cardiovascular death) in persons consuming a Mediterranean diet supplemented with extra virgin olive oil or nuts.10 The Mediterranean diet has been associated with improved diastolic parameters in HF.11 Fish oil supplementation in a small randomized trial improved ejection fraction and exercise capacity and decreased HF hospitalizations.12 In the Cardiovascular Health Study, the highest vs lowest quartile of omega 3 fatty acid plasma phospholipid concentration was associated with a lower incidence of HF (1.8 vs 2.8 per 1000 patient years).13 However, in the large GISSI-HF trial, fish oil supplementation (1g/d) had a modest 7% cardiovascular hospitalizations and 9% mortality benefits (P<.05).8 Alcohol intake has been associated with a U-shaped relationship with lower deaths in those with light to moderate intake compared with no or higher alcohol intake.14 It appears that components of the Mediterranean diet (fish intake, wine, olive oil, and nuts) may contribute to the lower incidence of HF observed in Catalonia along with an improved 69% 3-year survival.
In conclusion, patients with incident HF seen in PCPs in Catolonia are predominantly elderly and female. They have approximately 10%-12% annual mortality with a very low rate of cardiovascular hospitalization (<7%/y). Achieving these cardiovascular hospitalization rates for HF patients in the US and other countries would decrease the enormous cost of managing HF patients. Rather than have our HF patients move to Catalonia, future research should endeavor to identify why Catalonian patients have a lower incidence of HF and improved survival.
Conflicts of interestNone declared.