Although several factors associated with sex differences in the management and outcomes after acute coronary syndrome (ACS) have been reported, little is known about the influence of socioeconomic factors on sex disparities. Our aim was to evaluate the influence of country wealth and income inequality on national sex differences in mortality after ACS.
MethodsSex differences in 2-year postdischarge mortality were evaluated in 23 489 ACS patients from the EPICOR and EPICOR Asia registries. Adjusted Cox regression models by country-based terciles of gross national income per capita and income inequality were used.
ResultsWomen (24.3%) were older than men (65.5 vs 59.4 years, P <.001), had more comorbidities, were less often revascularized (63.6% vs 75.6%, P <.001) and received fewer guideline recommended therapies at discharge. Compared with men, a higher percentage of women died during follow-up (6.4% vs 4.9%, P <.001). The association between sex and mortality changed direction from hazard ratio (HR) 1.32 (95%CI, 1.17-1.49) in the univariate assessment to HR 0.76 (95%CI, 0.67-0.87) after adjustment for confounders. These differences were more evident with increasing country wealth (HRlow-incomecountries = 0.85; 95%CI, 0.72-1.00; HRmid-incomecountries = 0.66; 95%CI, 0.50-0.87; HRhigh-incomecountries = 0.60; 95%CI, 0.40-0.90; trend test P = .115) and with decreasing income inequality (HRlow-inequalityindex = 0.54; 95%CI, 0.36-0.81; HRintermediate-inequalityindex = 0.66; 95%CI, 0.50-0.88; HRhigh-inequalityindex = 0.87; 95%CI, 0.74-1.03; trend test P = .031).
ConclusionsWomen with ACS living in high socioeconomic countries showed a lower postdischarge mortality risk compared with men. This risk was attenuated in countries with poorer socioeconomic background, where adjusted mortality rates were similar between women and men.
Keywords
Several sex differences in access to care, management, and outcomes in acute coronary syndrome (ACS) have been described during the past decades,1–11 including longer delays in seeking and receiving attention. Compared with men, women are less likely to receive guideline-based therapies and have higher mortality rates,1–11 despite efforts to increase awareness of the problem and strategies to improve the cardiovascular health of women and reduce the gender gap.12–16 The reasons for these differences are multiple, including those related to patient characteristics (such as age and comorbidities), clinical presentation, and management (ie, lower or delayed access to diagnostic procedures and guideline recommended therapies). Although some socioeconomic factors, mainly related to income level, have been identified as risk factors for poorer prognosis in ACS patients,17,18 it is unknown whether these might influence sex differences in outcomes. Moreover, studies on sex differences in ACS patients come mainly from North America and Western Europe (largely high-income countries) with little data from other regions with a different socioeconomic background.19,20 As the influence of socioeconomic disparities across countries on sex differences in the clinical management and mortality of ACS patients is unknown, and most cardiovascular deaths occur outside Western Countries,21 it is important to consider the potential influence of socioeconomic background on top of the traditional clinical evaluation, to explain sex differences in mortality at a global level.
Our study aimed to: a) describe differences between women and men in 2-year mortality after discharge by country, and b) evaluate the influence of national wealth and national income inequality status on country differences in the gender gap in mortality after ACS.
METHODSStudy design and study populationEPICOR (long-tErm follow-uP of antithrombotic management patterns In acute CORonary syndrome patients, NCT01171404) and EPICOR Asia (NCT01361386) are two twin prospective, international, observational, real-world practice cohort studies comprising consecutive patients aged ≥ 18 years hospitalized for an ACS within 24 to 48hours of symptom onset who survived the index episode and were discharged from hospital.22,23 Exclusion criteria were secondary ACS (precipitated by a complication of surgery, trauma, gastrointestinal bleeding or percutaneous coronary intervention, or occurring during hospitalization for other reasons); unfeasible follow-up completion; <6 months life expectancy due to severe comorbidities; or previous enrolment in EPICOR or EPICOR Asia, or any randomized clinical trial. Patients were enrolled between September 2010 and March 2011 in EPICOR, and between June 2011 and May 2012 in EPICOR Asia. Informed consent was obtained from each patient and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
Individual data collection and follow-upData regarding baseline patient characteristics, clinical presentation of the index episode, in-hospital complications and management and discharge medication were homogenously collected from the 28 participating countries. Patients were followed up by centralized telephone interviews by trained native speakers of each patient's language, supervised by a Direct Patient Contact Manager up to death or 24 months after discharge. The primary outcome was all-cause mortality within the first 2 years after discharge. Given that all participants survived the index episode and were discharged, in-hospital mortality was not available by study design.
Socioeconomic analysis by countryThe national economic status per country was measured through the gross national income per capita (GNI) as provided by the World Bank Open Data using the contemporary Atlas (2011-2012).24 Countries were categorized into terciles based on their GNI. A sensitivity analysis was performed by grouping countries into high-income and middle-income countries,25 according to the World Bank income classification.26
Wealth inequality by country was evaluated by the Gini index provided by the World Bank Open Data (data corresponding to years 2011-2012).27 The Gini index measures the extent to which the distribution of income among individuals or households within an economy deviates from a perfectly equal distribution (a Gini index of 0% represents perfect equality, whereas an index of 100% implies perfect inequality). Of note, countries with unavailable Gini index (Hong Kong, Singapore, and Venezuela) were excluded from the analysis. Countries were categorized according to their income inequality level into terciles.
After applying these categorizations based on equal sized-terciles of countries, patients fell unevenly into these socioeconomic categories. For GNI, categories were: low-income countries (tercile 1: 10 countries, 15 133 patients), middle-income countries (tercile 2: 8 countries, 4 941 participants) and high-income countries (tercile 3: 8 countries, 3 415 patients). For the Gini index, categories for countries were: low inequality index (tercile 1: 9 countries, 3 813 participants), intermediate inequality index (tercile 2: 8 countries, 4 564 patients) and high inequality index (tercile 3: 8 countries, 14 327 participants).
Statistical analysisCategorical data are presented as frequency (%), while continuous data are presented as mean±standard deviation. Baseline comparisons by sex were performed using the chi-square or t test, as appropriate. Survival curves for 2-year mortality were obtained by sex for each socioeconomic level using the Kaplan-Meier method. Univariate Cox proportional hazards models were used to evaluate the association between sex and 2-year mortality thorough estimation of hazard ratios (HRs) and their 95%CI by each socioeconomic level.
Multivariate Cox proportional hazard regression models including covariates present in a 2-year mortality risk score previously derived from this cohort28 were performed to evaluate the association between sex and 2-year mortality. This risk model contains 18 predictors of 2-year mortality, ranked by predictive strength29: age, low ejection fraction at discharge, no coronary revascularization or thrombolysis, elevated serum creatinine at admission, poor quality of life (EuroQol 5 dimensions score), low hemoglobin, previous cardiac disease, previous chronic obstructive pulmonary disease, elevated blood glucose at admission, on diuretics at discharge, male sex, lower educational level, on aldosterone inhibitor at discharge, low body mass index, in-hospital cardiac complications, diagnosis of STEMI, Killip class, and region. The predictors of this risk score have been used for adjustment in previous studies.19,20,30 To avoid over-adjustment, the covariate region was excluded when other country-based categorizations were applied. To account for missingness of the covariates, a multiple imputation technique was applied using chained equations. Fifty imputed datasets were originally produced in the derivation of the risk score to deal with missingness in the 17 risk predictors included in the adjusted model.28 Percentages of missing values for each imputed factor are presented in table 1 of the supplementary data. This imputed dataset has been used in in previous studies.19,20,30
The fully adjusted multivariate Cox regression model was used to evaluate whether the association between sex and mortality risk was consistent across country-based categorizations (adding the interaction sex x income or sex x inequality, respectively) into the model and reporting the interaction P value for trend.31 Further modelling adjustment was performed by removing from the fully adjusted model some relevant clinical factors related to poor long-term survival in postACS patients (low ejection fraction, Killip class, in-hospital cardiac complications, on diuretics at discharge, and on aldosterone inhibitor at discharge). Adjusted HRs for 2-year mortality were obtained for each country. To avoid unreliable estimates, countries with fewer than 200 recruited participants or fewer than 3 deaths in 1 of their sex categories were excluded (Greece, Belgium, Denmark, Hong Kong, Luxembourg, Slovenia, Malaysia, Singapore and Vietnam). We then plotted each point estimate (HR) against their corresponding GNI and Gini index, and estimated the Pearson correlation coefficient for each comparison, weighted by group size, to determine the strength of the association between 2-year mortality and each country-based feature.28
The 2-tailed significance level was set at P <.05. All statistical analyses were performed using STATA software version 15.1 (Stata Corp, College Station, TX, United States). Results are reported according to the research reporting guidelines for observational studies (STROBE guidelines).
RESULTSSex differences in patient characteristics and mortalityIn total, 23 489 ACS patients were recruited from 774 hospitals in 28 countries across Europe and Latin America (EPICOR, 555 hospitals, 20 countries, n=10 567) and Asia (EPICOR Asia, 219 hospitals, 8 countries, n=12 922). Compared with men, women (n=5 712, 24.3%) were older, had more comorbidities, such as hypertension, hypercholesterolemia, diabetes mellitus and previous cardiac disease, and presented more often with non–ST-elevation ACS. Women less often received myocardial reperfusion therapies or coronary revascularization than men as well as guideline-based treatment at discharge (such as aspirin, any P2Y12 inhibitor, angiotensin converting-enzyme inhibitor or an angiotensin receptor blocker) and lipid lowering drugs. At discharge, fewer women showed reduced left ventricular ejection fraction. Further details on patient characteristics by sex are shown in table 1. Within 2 years after hospital discharge, 366 women (6.4%) and 879 men (4.9%) had died (HR, 1.32; 95%CI, 1.17-1.49; P <.001). However, after adjustment for other baseline variables, women had a more favorable mortality risk (adjusted HR, 0.76; 95%CI, 0.67-0.87, P <.001).
Baseline patient characteristics and early management of acute coronary syndrome by sex in the EPICOR registries (n=23 489)
| Women | Men | P | |
|---|---|---|---|
| Number of patients | 5712 (24.3) | 17 777 (75.7) | |
| Baseline characteristics | |||
| Age, y | 65.5±11.5 | 59.4±11.7 | <.001 |
| BMI <20 kg/m2 | 365 (7.2) | 597 (3.8) | <.001 |
| Hypertension | 3849 (67.9) | 9112 (51.8) | <.001 |
| Hypercholesterolemia | 1935 (35.5) | 5156 (30.2) | <.001 |
| Diabetes mellitus | 1699 (30.2) | 3867 (22.0) | <.001 |
| Family history of CAD | 1065 (20.9) | 3202 (19.8) | .083 |
| Previous heart disease | 1636 (29.2) | 4158 (23.9) | <.001 |
| Peripheral vascular disease | 166 (3.0) | 465 (2.7) | .22 |
| Chronic kidney disease | 160 (2.9) | 467 (2.7) | .45 |
| COPD/CLD | 276 (4.9) | 759 (4.4) | .064 |
| Education | <.001 | ||
| No formal | 749 (17.1) | 776 (5.6) | |
| Primary | 1649 (37.7) | 3884 (27.9) | |
| Secondary | 1601 (36.6) | 6413 (46.1) | |
| Tertiary | 373 (8.5) | 2836 (20.4) | |
| Clinical presentation | |||
| Final admission admission | <.001 | ||
| NSTEMI | 1758 (30.8) | 4800 (27.0) | |
| STEMI | 2189 (38.3) | 9370 (52.7) | |
| Unstable angina | 1765 (30.9) | 3607 (20.3) | |
| Killip class | <.001 | ||
| I | 3229 (78.9) | 11 658 (82.2) | |
| II | 563 (13.8) | 1664 (11.7) | |
| III | 199 (4.9) | 516 (3.6) | |
| IV | 102 (2.5) | 352 (2.5) | |
| Hemoglobin <13 g/dL | 2910 (53.8) | 3488 (20.7) | <.001 |
| Creatinine ≥ 1.2 mg/dL | 792 (14.6) | 4492 (26.5) | <.001 |
| Blood glucose> 160 g/dL | 1316 (26.2) | 3549 (22.7) | <.001 |
| LVEF <40% | 426 (8.1) | 1564 (9.5) | .003 |
| EQ-5D score at discharge | <.001 | ||
| 0 | 2568 (45.9) | 10 362 (59.4) | |
| 1 | 952 (17.0) | 2787 (16.0) | |
| ≥ 2 | 2074 (37.1) | 4287 (24.6) | |
| In-hospital complications | |||
| Any in-hospital cardiac complication | 969 (17.0) | 2837 (16.0) | .069 |
| Recurrent MI | 154 (2.7) | 468 (2.7) | .79 |
| Recurrent ischemia | 167 (3.0) | 447 (2.5) | .092 |
| Heart failure | 369 (6.5) | 910 (5.1) | <.001 |
| Atrial fibrillation/flutter | 232 (4.1) | 548 (3.1) | <.001 |
| Management | |||
| Coronary revascularization or thrombolysis | 3608 (63.6) | 13 378 (75.6) | <.001 |
| Aspirin at discharge | 5374 (94.2) | 17 067 (96.2) | <.001 |
| Any P2Y12inhibitor at discharge | 5043 (88.5) | 16 570 (93.4) | <.001 |
| BB at discharge | 4335 (76.2) | 13 704 (77.3) | .079 |
| ACE/ARB inhibitors at discharge | 3844 (67.6) | 12 349 (69.7) | .003 |
| Lipid lowering drugs at discharge | 5187 (90.8) | 16 379 (92.1) | .001 |
| MRA at discharge | 499 (8.8) | 1418 (8.0) | .061 |
| Diuretics at discharge | 1125 (19.8) | 2535 (14.3) | <.001 |
ACE/ARB, angiotensin converting enzyme inhibitor/angiotensin II receptor blocker; BB, beta blocker; BMI, body mass index; CAD, coronary artery disease; COPD/CLD, chronic obstructive pulmonary disease chronic lung disease; EQ-5D, EuroQol; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonist; NSTEMI, non–ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction; VF, ventricular fibrillation.
Data are expressed as No. (%) or mean±standard deviation.
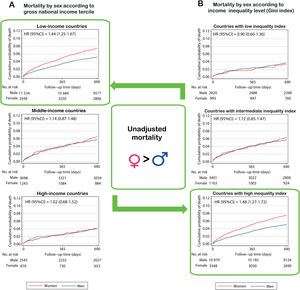
GNI and Gini index values for each country are shown in table 2 of the supplementary data. The classification of countries by terciles based on GNI and Gini index is shown in table 3 of the supplementary data. Survival curves and by sex unadjusted HRs (95%CI) for each level of analysis (GNI and Gini index) are shown in figure 1. Briefly, mortality rates were higher in women than in men in less wealthy countries (HRlow-incomecountries, 1.44; 95%CI, 1.25-1.67; P <.001), and in those with higher income inequality indices (HRcountrieswithhigh-inequalityindex, 1.48; 95%CI, 1.27-1.72; P <.001). The association between sex and mortality risk changed direction from an unadjusted HR of 1.32 (95%CI, 1.17-1.49) to an adjusted HR of 0.76 (95%CI, 0.67-0.87) after we took into account potential confounders, including age and comorbidities but also in-hospital and discharge therapies and acute complications.
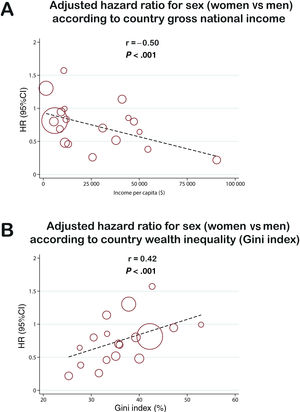
To assess the association between sex differences and 2-year mortality and each level of categorization at the country level, we plotted HRs (women vs men) for each country against their corresponding GNI and Gini index levels (figure 2). A Pearson correlation coefficient was estimated, obtaining a negative correlation between the sex-related increase in adjusted mortality risk per country and the national GNI (r=−0.50; P <.001) and a positive correlation with the income inequality index (r=0.42; P <.001) (figure 2).
Correlation between national sex-related increase in adjusted 2-year mortality risk (hazard ratios [HR]) and country gross national income per capita (A) and country level of income inequality by the Gini index (B). Correlation between the fully adjusted hazard ratios (women vs men) for 2-year all-cause mortality, according to country gross national income per capita and income inequality (Gini index). Each circle represents a country and its size is scaled according to its sample size (number of participants included in this registry for each country). 95%CI, 95% confidence interval.
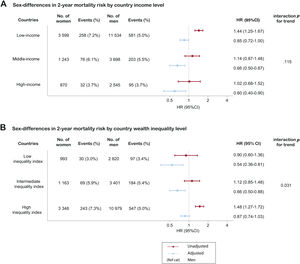
Multivariate analyses by GNI level showed that women living in the wealthiest countries were at lower mortality risk than men (HRhigh-incomecountries 0.60; 95%CI, 0.40-0.90; P=.014), while this advantage was smaller in intermediate wealthy countries (HRmid-incomecountries 0.66; 95%CI, 0.50-0.87, P=.003) and even smaller in the least wealthy countries (HRlow-incomecountries, 0.85; 95%CI, 0.72-1.00; P=.049); test for trend across HRs P=.115 (figure 3). When countries were classified as intermediate or high GNI level according to the World Bank, a large difference in mortality risk between women and men was found in high-income countries (HRhigh-incomecountries, 0.61; 95%CI, 0.48-0.78, P <.001), whereas a smaller difference was found in middle-income countries (HRmid-incomecountries, 0.85; 95%CI, 0.72-0.99, P=.036), overall P for interaction=.024). Women living in the countries with highest inequality indices showed a similar adjusted mortality to men in (HRcountrieswithhigh-inequalityindex 0.87; 95%CI, 0.74-1.03; P=.106), while those living in countries with less income inequality had a significantly lower adjusted risk for 2-year mortality (HRcountrieswithintermediate-inequalityindex 0.66; 95%CI, 0.50-0.88, P=.004; HRcountrieswithlow-inequalityindex 0.53; 95%CI, 0.36-0.81; P=.003); test for trend across HRs P=.031 (figure 3). Consistent findings were found after removal of some relevant clinical factors related to poor long-term survival in post-ACS patients from the confounders (tables 4-7 of the supplementary data). Further sensitivity analyses showed that differences between women and men in some relevant treatments (ie, revascularization) were consistent across socioeconomic categories (ie, women were consistently less revascularized than men in each strata; figure 1 of the supplementary data). Moreover, we estimated differences in incidence rates for women and men using multivariate Poisson models adjusted for the 17 potential confounders. This thorough analysis revealed that, although incidence rates varied for both women and men across socioeconomic categories, these variations were of different magnitude in men and women.
Forest plot with adjusted hazard ratio for 2-year mortality risk assessing the interaction between sex and country socioeconomic status. Assessment of the interaction between sex and socioeconomic background in terms of: (A) national wealth (countries were categorized into terciles based on their gross national income per capita) and (B) income inequality (countries were categorized into terciles based on their Gini index, a measure of income inequality). Risk of 2-year mortality expressed as hazard ratios (HR) with its 95% confidence interval (95%CI) after adjustment for 17 risk predictors included in the EPICOR risk model (age, low left ventricular ejection fraction, no coronary revascularization/thrombolysis, elevated serum creatinine at admission, poor EuroQol-5 dimensions score, low hemoglobin at admission, previous cardiac disease, previous chronic obstructive pulmonary disease, elevated blood glucose at admission, prescription of diuretic agents at discharge, lower educational level, prescription of an aldosterone inhibitor at discharge, low body mass index, in-hospital cardiac complications, type of acute coronary syndrome, and Killip class). In addition to these covariates, the interaction term “income x sex” and “inequality x sex” were introduced into each regression model, respectively.
Our study shows for the first time that national socioeconomic status influences the gender gap in mortality risk after ACS, particularly the Gini index, that is, the national level of income inequality. This is relevant as most efforts to reduce the gender gap in the management and outcomes of ACS have been, logically, focused on the health care system and health professionals. Our findings suggest that there is a systemic social component contributing to these differences that should be considered a target for action.
After ACS, women had higher crude mortality than men but, concordant with prior studies,4,5,10 they differed substantially from men with respect to a) baseline characteristics (they were older and had more comorbidities), and b) the treatments used during the index hospitalization, less often receiving coronary revascularization and guideline-based therapies at discharge. Thus, after adjustment for these confounders, the risk of all-cause death at 2 years after discharge was lower in women. To interpret correctly the lower risk of women after discharge, it is important to understand that our comprehensive model for adjustment includes not only the differences in patient characteristics but also their initial treatment and early in-hospital complications, so it does control for the presence of a potential initial gender gap in the management and its consequences. The difference between unadjusted and adjusted risks implies that if some differences in treatment were reduced, the differences in mortality between men and women might be further increased (ie, if women had a higher percentage of revascularization, they would have an even better prognosis).
Women living in wealthier countries and in countries with less income inequality were at the lowest risk for 2-year mortality compared with men, whereas this advantage was attenuated in poorer countries and in those with higher income inequality, where there was no significant difference in adjusted 2-year mortality risk between women and men. We hypothesize that social disparities may be partially rooted in the levels of national wealth and, more so, in the level of income inequality, which may be a surrogate for social gender inequity in general and for health care provision in particular, including ACS care, which may have an impact on sex differences in mortality. The inconsistent lower 2-year mortality risk in women compared with men across country wealth and income inequality categories suggests that women might be at a lower risk of dying after an ACS than men after controlling for the differences in early care and outcomes, although the socioeconomic background of their countries might attenuate this relationship. There was a steep gradient in sex differences in 2-year mortality across countries based on their unequal income distribution: women were at lower risk than men if they were living in less unequal countries, whereas there was no difference in terms of mortality between women and men if they were living in countries with high income inequality. The opposite happened for GNI: the higher the income per capita, the lower the risk of death for women compared with men. Although it was previously reported that patients from low-income countries with greater inequality had the highest mortality rates,25 this is the first large international registry reporting the impact of socioeconomic factors on sex differences in mortality in patients with ACS.
Country income and wealth distribution may have a major impact on the availability, access to, provision of, and affordability of relevant medical interventions, such as guideline-based therapies, but also on other meaningful factors, such as nutrition, education, employment and social care, all of them with an already known impact on general and psychological wellbeing, quality of self-care, and the outcome of cardiovascular diseases.32–35 For instance, income inequality, as assessed by the Gini coefficient, has already been associated with worse outcomes in heart failure patients, with an impact similar to those of major comorbidities.36 Our findings reinforce the need to improve health and social care in lower income countries, as well as in those with marked wealth disparities, where women might find it a harder to access quality health care services and there may be suboptimal use of secondary prevention medicines. These interventions might have an impact on women's health by reducing their risk of death to levels similar to those observed in countries with higher socioeconomic standards. Importantly, approximately 80% of worldwide cardiovascular deaths occur in low- or middle-income countries25 and policies aimed to improve health care and social provision, for which country income (per capita) and wealth distribution are thought to be surrogates, might have an overwhelming impact on improving women's health and reducing gender gaps in health care at a global level.
Study limitationsThis study has a number of limitations. Because of the observational nature of the data, the study design cannot show a causal relationship, but only an association between country socioeconomic backgrounds and sex differences in 2-year mortality. Nevertheless, these exposures (wealth levels and income inequality) cannot be randomized and can only be evaluated through this type of epidemiological study. More solid conclusions would be obtained from registries specifically designed to evaluate the association between socioeconomic level and sex disparities in outcomes at the individual level. Second, while both registries were designed to recruit representative patients from representative centers in each country, we cannot rule out a bias regarding the type of hospitals recruiting patients.19,20 It is likely that patients from countries with a lower income and higher inequality index recruited better off patients, hence the interaction between sex and mortality might be even greater. Some caution is needed to extrapolate our findings to countries with a similar socioeconomic background. For instance, the Gini index has some limitations: a) the size of the country may influence the index (smaller countries tend to show lower coefficients due to their lower diversity, whereas larger countries, more diverse, tend to have higher coefficients); and b) the composition of the population may also have had an impact on the index (younger populations tend to be associated with higher inequality due to their lower incomes, whereas the opposite happens for older populations). Some degree of correlation between income and wealth inequality might exist between countries. Finally, despite the wide geographic representation, some important regions were not included.
CONCLUSIONSIn a global population of ACS patients, women living in high socioeconomic countries have a lower postdischarge mortality risk than men, which disappears in countries with a poorer socioeconomic background (less wealthy countries or countries with higher income inequalities). Our findings highlight the need for renewed focus on achieving better health care for women in settings where poverty and/or unequal wealth distribution exist.
FUNDINGThe EPICOR and EPICOR Asia studies were funded by AstraZeneca.
AUTHORS’ CONTRIBUTIONSX. Rossello, C. Mas-Lladó, L. Vicent, J. Medina and H. Bueno conceived the study and X. Rossello conduced the analysis. S. Pocock provided statistical advice on study design and analyzed the data. J. Medina, H. Bueno and Y. Huo obtained research funding and supervised the conduct of the registry and data collection. F. Van de Werf, C. Tang Chin, N. Danchin, S.W.L. Lee, Y. Huo and H. Bueno undertook recruitment of participating centers and patients. X. Rossello drafted the article, and all authors contributed substantially to its revision.
CONFLICTS OF INTERESTX. Rossello has nothing to disclose. C. Mas-Lladó has nothing to disclose. S. Pocock has received research funding from AstraZeneca. F. Van de Werf has received consulting fees and research grants from Boehringer Ingelheim, Merck and Sanofi, and consulting and speaking fees from Boehringer Ingelheim, Roche, Sanofi, AstraZeneca, and The Medicines Company. C. Tang Chin has received consulting or speaking fees from AstraZeneca, Merck, Servier, and Medtronic. N. Danchin has received consulting or speaking fees from Amgen, AstraZeneca, Bayer, BMS, Boehringer Ingelheim, Intercept, MSD, NovoNordisk, Pfizer, Sanofi-Aventis, Servier, and UCB pharmaceuticals. S.W.L. Lee has nothing to disclose. J. Medina is an employee of AstraZeneca. Y. Huo has nothing to disclose. H. Bueno receives research funding from the Instituto de Salud Carlos III, Spain (PIE16/00021 & PI17/01799), Sociedad Española de Cardiología, AstraZeneca, Bayer, BMS and Novartis; has received consulting fees from AstraZeneca, Bayer, BMS-Pfizer, Novartis; and speaking fees or support for attending scientific meetings from Amgen, AstraZeneca, Bayer, BMS-Pfizer, Novartis, and MEDSCAPE-the heart.og.
Several sex differences in access to care, management, and outcomes in acute coronary syndrome (ACS) have been described over the past decades. Although some socioeconomic factors, mainly related to income level, have been identified as risk factors for worse prognosis in ACS patients, it is unknown whether a socioeconomic component might influence sex differences in outcomes.
WHAT DOES THIS STUDY ADD?Women living in wealthy countries or countries with low income inequalities have a lower risk of dying within 2 years compared with men, whereas mortality risks are similar between men and women living in countries with a poorer socioeconomic background. Our findings suggest that there is a systemic social component contributing to sex differences that should be considered a target for action. This is a change in the current paradigm, which focuses most efforts in reducing the gender gap in the management and outcomes of ACS on the health care system and health professionals.
CNIC is partially supported by a competitive grant from the Carlos III Institute of Health–Fondo de Investigación Sanitaria and the European Regional Development Fund (ERDF/FEDER) (PI13/01979), the Spanish Ministry of Science, Innovation and Universities (MICINN) and the Pro-CNIC Foundation and is a Severo Ochoa Centre of Excellence (MINECO award SEV-2015-0505).
Supplementary data associated with this article can be found in the online version available at https://doi.org/10.1016/j.rec.2021.05.006



![Correlation between national sex-related increase in adjusted 2-year mortality risk (hazard ratios [HR]) and country gross national income per capita (A) and country level of income inequality by the Gini index (B). Correlation between the fully adjusted hazard ratios (women vs men) for 2-year all-cause mortality, according to country gross national income per capita and income inequality (Gini index). Each circle represents a country and its size is scaled according to its sample size (number of participants included in this registry for each country). 95%CI, 95% confidence interval. Correlation between national sex-related increase in adjusted 2-year mortality risk (hazard ratios [HR]) and country gross national income per capita (A) and country level of income inequality by the Gini index (B). Correlation between the fully adjusted hazard ratios (women vs men) for 2-year all-cause mortality, according to country gross national income per capita and income inequality (Gini index). Each circle represents a country and its size is scaled according to its sample size (number of participants included in this registry for each country). 95%CI, 95% confidence interval.](https://static.elsevier.es/multimedia/18855857/0000007500000005/v2_202205130657/S1885585721001596/v2_202205130657/en/main.assets/thumbnail/gr2.jpeg?xkr=eyJpdiI6Ik8zSm1QeERwWHF2bkZDN0dBeUVWQ2c9PSIsInZhbHVlIjoiYUZRWU9lcTd6aSt0ZEh2STJkZWRyRUIwbXkrQlJrUEJQYlZNNDRGRW5oaz0iLCJtYWMiOiJiYmVlODM0NGE5M2FmYjUzOWI0YjdiNWJmNDRmNWUzYmZiNmI2OTBjNDBhYmE0ZGYxYzgyOGRiYTI5YjNhMzA5IiwidGFnIjoiIn0=)
