To the Editor,
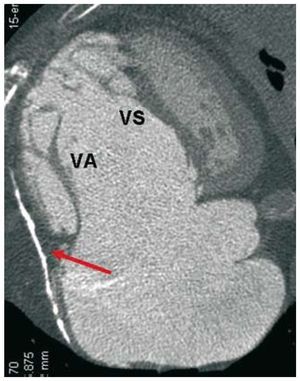
We present the case of a 52-year-old male, smoker who drinks approximately 60 g of alcohol daily and is under observation for atrial fibrillation and an Ebstein anomaly that was causing massive tricuspid regurgitation (TR) and right heart failure (RHF), treated with diuretics. He was admitted due to a notable clinical worsening with severe ascites. A chest radiograph showed the presence of a left pleural effusion (Figure 1A) and the lateral view demonstrated a sharp line of pericardial calcification, indicating pericardial constriction (Figure 1B, arrow).
Figure 1. Thoracic radiographs.
The pleural effusion proved to be transudative. Following multiple recurrences, a permanent intrapleural catheter was placed to drain the effusions as needed. Analysis of the ascitic fluid indicated that portal hypertension had caused the ascites. Although RHF could have caused it, we first had to ensure that it was not due to cirrhosis. The liver examination using ultrasound and fibroscan was inconclusive, and the laboratory tests (hemoglobin, platelets, creatinine, proteins, coagulation study, transaminases, and bilirubin) came back normal. Lastly, a transjugular liver biopsy showed that it was cirrhosis. The etiological study found no other causes in addition to those proposed a priori (alcohol and congestion), and the clinical, histopathological, and laboratory data indicated that congestion was the primary cause.1
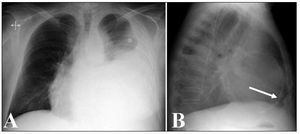
The echocardiogram still indicated a diagnosis of Ebstein anomaly, and underlined its functional repercussions, the massive TR, and consequent right heart overload, which hindered the evaluation of echocardiographic signs of pericardial constriction. The multislice computerized tomography provided an anatomical definition of the Ebstein anomalies, and revealed extensive calcification of the right pericardium2 (Figure 2). During the heart catheterization, coronary disease was ruled out and we performed the hemodynamic diagnosis of constriction.2
Figure 2. Multislice computerized tomography showing pericardial calcification around the severely dilated right chambers (arrow), insertion under the septal tricuspid valve (SV) and a long anterior tricuspid valve (AV) adhered to the free wall of the right ventricle.
After discussing the various treatment options, we proposed tricuspid repair with a right pericardiectomy.2,3 If the ascites is caused by the RHF, a class A-6 cirrhosis on the Child-Pugh scale would imply an acceptable surgical risk. However, if cirrhosis was the cause, class B-9 on the Child-Pugh scale would imply a high-risk procedure.4 Even so, a Model for End-Stage Liver Disease (MELD) score of 8 meant an improved prognosis.5
The patient's initial postoperative evolution was favourable, but RHF worsened on day 6. The echocardiogram showed severe residual TR and a large clot that was compressing the right ventricle. After another intervention, the patient's progress was slow. First, he suffered from hepatorenal syndrome requiring hemodialysis. He then had severe pulmonary sepsis that triggered death of the patient 1 week after the second procedure.
Ebstein anomalies and pericardial constriction can be considered as rare diseases.2,3 It is extremely rare for both conditions to simultaneously appear in one patient. Symptoms are not sufficient to be able to diagnose the 2 conditions, requiring imaging tests and hemodynamic data. Cardiac cirrhosis intensifies the clinical manifestations of RHF and complicates patient care.1 Both tricuspid valve surgery5 and pericardiectomy6 have high mortality rates. Morbidity after cardiovascular surgery is much higher if the patient has cirrhosis, and the prognosis is influenced by the functional state of the liver disease. Although the Child-Pugh classification system is very useful for this objective,4 the MELD score has also been used in recent years, and its value has been demonstrated in tricuspid valve surgeries.5