We read with special interest the recent article in Revista Española de Cardiología by Rey et al.1 on a patient with acute coronary syndrome (ACS) and simultaneous thromboses in 2 coronary arteries in the context of coronavirus disease 2019 (COVID-19). We would like to report a case with similar characteristics, in which the patient was a 55-year-old man with a history of hypertension, type 2 diabetes mellitus, former smoker (30 pack-years), chronic obstructive pulmonary disease defined as Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 2A, and no known history of heart disease. Our patient presented to the Emergency Department with a history lasting several days of orthopnea and dry cough, describing dyspnea and squeezing chest pain that had lasted some days but had completely disappeared by the time he arrived.
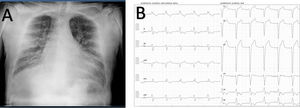
Electrocardiography revealed newly appeared left bundle-branch block (LBBB) that did not meet the Sgarbossa criteria. However, myocardial injury markers were elevated (high-sensitivity troponin T of 220 ng/L followed by 333 ng/L at 3h, with dynamics consistent with ACS). Point-of-care echocardiography showed severe left ventricular dysfunction with akinesia of the anterior, lateral, and posterior segments, inferior hypokinesia, and asynchronous contractility due to LBBB. Chest radiography revealed interstitial pattern and bilateral alveolar infiltrates, consistent with COVID-19 infection (figure 1). Two PCR tests for COVID-19 were negative.
The patient was admitted to the intensive care unit, and medical treatment was started for ACS along with diuretic, vasodilator, and inotropic therapy. Coronary angiography showed a severe lesion in the obtuse marginal artery, which was revascularized with a drug-eluting stent.
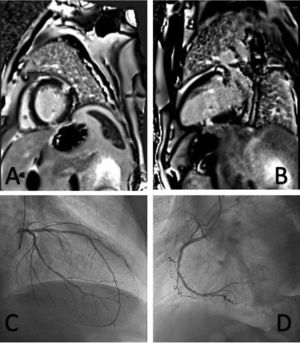
Once in the ward, the patient underwent comprehensive echocardiography showing severe systolic dysfunction due to general hypokinesia with considerable asynchrony (left ventricular ejection fraction by biplane Simpson's method, 29%), with no other findings of interest. Subsequent cardiac magnetic resonance imaging showed 2 foci of late transmural enhancement in the sequences: 1 in the short axis view, in the mid anterolateral and lower medial segments, and 1 in the 2-chamber long axis view, in the anterior basal and lower medial segments, which would be consistent with simultaneous acute infarctions, given that the edema sequences showed infarction in these regions (figure 2).
After the patient was stabilized, a decision was made to discharge him to home with medical treatment for ACS and heart failure with reduced left ventricular ejection fraction.
Outpatient follow-up with the heart failure unit of our hospital showed that the patient currently has no cardiovascular symptoms and has partially recovered left ventricular ejection fraction (40%) after the disappearance of LBBB. Because the admission radiograph was consistent with COVID-19 and there were transmural infarctions in several territories, a decision was made to perform a new PCR test for COVID-19 and serology testing by enzyme-linked immunosorbent assay (ELISA), which was positive for immunoglobulin G (IgG).
Coronaviruses and the remaining microorganisms causing acute respiratory infections are known to be key triggers for the development of ACS.2 The most common complications related to this virus are acute respiratory distress syndrome, secondary infections, and shock,2 but a number of case reports have been published on arterial thromboses secondary to the virus, including the article mentioned,1 possibly due to the virus-induced hypercoagulable state secondary, among other factors, to the cytokine storm or blood stasis caused by immobilization.3
The case we describe is similar to that reported in King et al.,1 except for the difference that coronary angiogram showed a severe lesion in only 1 epicardial blood vessel, but subsequent cardiac magnetic resonance imaging revealed 2 infarctions in different coronary territories.
This case underscores the importance of implementing screening and diagnostic techniques suitable for detecting this type of patient, as well as asymptomatic carriers (in our patient 3 PCR tests were negative, but IgG was positive for COVID-19).