To the Editor:
Certain congenital heart defects with alteration of the right ventricular outflow tract require the surgical implantation of prosthetic valves that usually evolve towards stenosis, insufficiency or both, which generates ventricular dysfunction and the need for new surgery. Percutaneous pulmonary valves represent the most important advance in percutaneous treatment of congenital heart defects and can avoid or delay new surgery.1
The Melody® (Medtronic Inc) valve consists of a 35 mm platinum-iridium stent to which a valved bovine jugular vein graft has been attached. For its implantation, a specific introducer-liberator with a thickness of 22 Fr and 3 possible diameters of expansion2: 18, 20, and 22 mm is needed. It is indicated in dysfunctional valves with an original diameter of ≥16 mm, implanted in the right ventricular outflow tract, with invasive intervention or surgery. Contraindications are the impossibility to expand the stenosis through catheter-balloon, coronary compression, active infection, and an anatomical incompatibility with the appropriate adherence of a 22 mm stent.
Seven patients were selected in our hospital (average age, 19; range, 11-26). Diagnoses: transposition of great arteries with interventricular communication and pulmonary stenosis (3); tetralogy of Fallot with infundibular coronary artery (2); pulmonary atresia with interventricular communication (1), and double outlet right ventricle with pulmonary stenosis (1); 4 presented stenosis of a 17 mm (1) or 18 mm (3) aortic homograft and 1 was also insufficient; 2 had stenotic pulmonary homografts measuring 18 and 20 mm and in 1 a Gore-Tex valveless tube with severe insufficiency. They were all studied by echocardiography; an angiograph was performed on 4 via computerised tomography and in the remaining 3, magnetic resonance imaging.
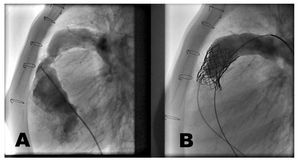
The implantation of the percutaneous pulmonary valve was performed with excellent results on 4 patients: 3 with predominant stenosis (Figure 1), in which the average systolic gradient went from 43 to 13 mm Hg and 1 with severe insufficiency, and it was not possible in 3: 2 due to coronary compression and 1 due to impossibility of expanding a severely calcified stenosis.
Figure. 1. A: severe stenosis of the homograft. B: resolution of the stenosis, no regurgitation.
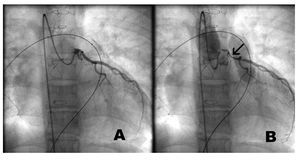
The risks of the percutaneous pulmonary valve implantation are related to the use of rigid guides and large calibre introducers, as well as those derived from the dilation of rigid and calcified stenotic structures. The possible compression of the adjacent coronary arteries, produced on expanding the dysfunctional valve with the stent implantation, should be carefully examined and avoided through selective coronary catheterisation while the balloon is dilated to the diameter of the chosen valved stent. Two patients presented coronary compression which impeded continuing with the procedure (Figure 2).
Figure 2. A: selective coronary catheterisation. B: the arrow indicates severe compression of the proximal area of the left coronary artery.
Percutaneous pulmonary valves are an alternative to surgery, with comparable results but less aggressive for the patient and although their evolution in the long-term is unknown, results from the first series of patients are encouraging.3
The ability of the right ventricle subject to prolonged volume overload to recover is limited and therefore the study of its function and morphology is complex,4 despite the significant advances obtained by magnetic resonance imaging. Percutaneous implantation of the pulmonary valve probably helps to delay the moment of treatment indicated in dysfunction of the previously implanted valves in the right ventricular outflow tract.5 The evolution of the devices will also help to enlarge the small group of patients who can currently benefit from this technique.6